![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
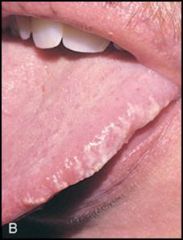
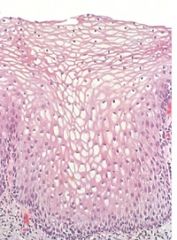
Diagnosis?
|
Hairy leukoplakia
|
|
|
What is hairy leukoplakia associated with?
|
HIV infection or other immunocompromised states. It is caused by EBV infection.
|
|
|
What is the distinctive microscopic appearance of hairy leukoplakia?
|
Hyperparakeratosis and acanthosis with "balloon cells" in the upper spinous layer.
|
|

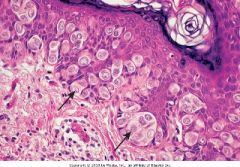
Diagnosis?
|
Leukoplakia with invasive SCC
|
|
|
What is the definition of leukoplakia?
|
A white patch or plaque that cannot be scraped off and cannot be characterized clinically or pathologically as any other disease.
|
|
|
What are patients with leukoplakia at risk for developing?
|
Leukoplakia is precancerous and these patients are at risk for developing SCC.
|
|

Diagnosis?
|
Mucocele
|
|
|
Describe the histology of mucocele.
|
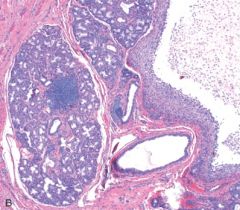
Cystic spaces filled with mucin and inflammatory cells such as macrophages.
|
|
|
What is a ranula?
|
Histologically, it is identical to a mucocele, but specifically refers to a mucocele when the duct of the sublingual gland is damaged.
|
|

Diagnosis?
|
Ranula
|
|
|
Describe the epidemiology of nasopharyngeal carcinoma.
|
a) Most common malignant tumor of the nasopharynx
b) Male dominant c) Increased incidence in China (adult) and Africa (children) |
|
|
What is the cause of nasopharyngeal carcinoma?
|
EBV
|
|
|
What are the pathological findings associated with nasopharyngeal carcinoma?
|
SCC or undifferentiated cancer that metastasizes to cervical lymph nodes.
|
|
|
What is Candida albicans associated with in the female genital tract?
|
It is a normal part of the vaginal microbiota and is a common cause of vaginitis. Risk factors include diabetes, antibiotics, pergnancy, and OCPs.
|
|
|
What is Trichomonas vaginalis associated with?
|
It is a flagellated protozoan that produces vaginitis, cervicitis, and urethritis.
|
|
|
What is Treponema pallidum associated with?
|
It is a gram negative spirochete that causes syphilis.
|
|
|
What are the three types of syphilis?
|
Primary: solitary painless indurated chancre.
Secondary: maculopapular rash on trunk, palms, soles. Tertiary: Neurosyphilis, aortitis, gummas |
|
|
What is HSV-2 associated with?
|
It is a virus that remains latent in sensory ganglia. It causes recurrent vesicles that ulcerate.
|
|
|
How can HSV-2 be diagnosed?
|
Tzanck preparation: Scrapings from base of ulcer yield multinucleated squamous cells with eosinophilic intranuclear inclusions.
|
|
|
What non-cervical lesion is HPV associated with?
|
Types 6 and 11 are associated with genital warts (condyloma acuminata).
|
|
|
What are some obvious microscopic changes seen with HPV infection of the skin?
|
Koilocytic changes in squamous epithelium.
|
|
|
What are five different vulvular tumors?
|
1) Papillary hidradenoma
2) Vulvar intraepithelial neoplasia 3) Squamous cell carcinoma 4) Extramammary paget's disease 5) Malignant melanoma |
|
This is a biopsy from a red crusted vulvar lesion. What is the diagnosis?
|
Extramammary Paget's disease forming intraepithlial adenocarcinoma. The malignant Paget's cells contain mucin (PAS +).
|
|
|
Which vulvar carcinomas is HPV associated with?
|
VIN which may then develop into SCC.
|
|
|
How can malignant melanoma be distinguished from extramammary Paget's disease?
|
MM is PAS negative.
|
|
|
Describe the clinical picture of a patient with sarcoma botryoides.
|
Also known as embryonal rhabdomyosarcoma, this is a grape-like mass protruding from the vagina of girls < 5 y/o.
|
|
|
A patient whose mother was treated with DES for attempted abortion presents with vaginal adenosis. What is she at risk for developing?
|
Clear cell adenocarcinoma.
|
|
|
What does DES do?
|
It inhibits mullerian differentiation leading to the persistence of remnants. This leads to vaginal adenosis which is a precursor lesion for clear cell adenocarcinoma.
|
|
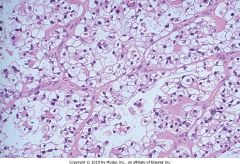
This is a vaginal biopsy, what is the diagnosis?
|
Clear cell adenocarcinoma
|
|
|
What is the transformation zone?
|
The region in the cervix where the pH changes and the squamous metaplasia occurs. This are is particularly susceptible to dysplasia.
|
|
What is the diagnosis?
|
Normal cervical tissue
|
|
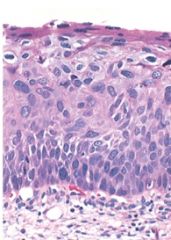
What is the diagnosis?
|
CIN II
|
|
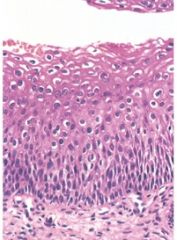
What is the diagnosis?
|
CIN I
|
|
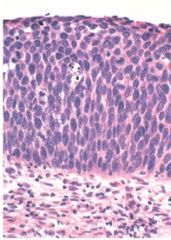
What is the diagnosis?
|
CIN III
|
|
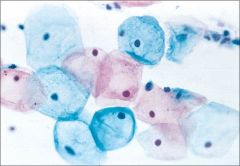
What is the diagnosis?
|
Normal Pap smear
|
|
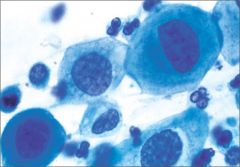
What is the diagnosis?
|
HSIL: CIN II
|
|
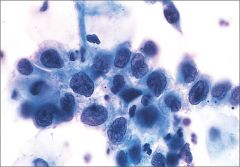
What is the diagnosis?
|
HSIL: CIN III
|
|
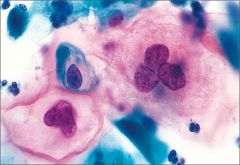
What is the diagnosis?
|
LSIL: CIN I
|
|
|
What is the most common cause of death in cervical cancer?
|
Renal failure due to cancer causing obstruction of the ureters.
|
|
|
What is the most common cause of dysfunctional uterine bleeding?
|
An anovulatory cycle.
|
|
|
How does an anovulatory cycle cause dysfunctional uterine bleeding?
|
Failure of ovulation results in prolonged, excessive, endometrial stimulation by estrogens with an absence of the progestational phase.
|
|
|
What is the diagnosis?
|
Endometriosis of the colon.
|
|

Diagnosis?
|
Endometriosis of the colon.
|
|
|
What is adenoacanthoma?
|
Endometrial carcinoma which contains glands as well as foci of squamous elements. (20% of endometrial carcinoma)
|
|
|
What is the most common form of endometrial carcinoma?
|
Adenocarcinoma.
|
|
|
What are the two types of endometrial carcinoma and what are they associated with?
|
Type I: increased estrogens, PTEN protein absent, well-differentiated, good prognosis.
Type II: endometrial atrophy, papillary serous Ca, poorly differentiated, poor prognosis. |
|
|
What is a leiomyoma?
|
A benign smooth muscle tumor that is relatively common, usually in multiples (fibroids), and respond to estrogen.
|
|
|
What is a leiomyosarcoma?
|
An uncommon, de novo tumor of the uterus. Malignancy depends on number of mitotic figures per field (> 5), tumors metastasize and poor prognosis.
|
|
|
What may mucinous tumors of the ovary cause?
|
They resemble endocervix or intestinal tissue, and due to secretion of mucin into the peritoneum, cause pseudomyxoma peritonei (jelly belly).
|
|
|
Where do mucinous tumors of the ovary usually arise from?
|
They usually arise from spread of pancreatic mucinous tumors.
|
|
|
What is a teratoma?
|
A dermoid cyst containing hair, tooth, cheesy material, thyroid tissue, and bone. Usually benign and contains at least 2 types of tissue.
|
|
|
List the four types of germ cell tumors.
|
Teratoma, choriocarcinoma, dysgerminoma, endodermal sinus tumor (yolk sac tumor)
|
|
|
What markers do all germ cell tumors express?
|
alpha-fetal protein, hCG, alpha1-antitrypsin
|
|
|
What are some important findings in granulosa-theca cell tumors?
|
Call-Exner bodies (follicles with coffee-bean nuclei), estrogen production, and Inhibin and Calretinin expression.
|
|
|
How do complete hydatidiform moles develop.
|
Loss of genetic material in ovum and either fertilization with a single sperm that undergoes chromosomal duplication or dispermy.
|
|
|
How do partial hydatidiform moles develop?
|
Fertilization of normal ovum with two sperm yielding triploidy.
|
|
|
What are the critical abnormalities that occur in preeclampsia?
|
Diffuse endothelial dysfunction, vasoconstriction (leading to HTN), and increased vascular permeability (resulting in proteinuria and edema).
|
|
|
If preeclampsia develops to eclampsia, what may happen?
|
HELLP syndrome. Hemolysis, Elevated Liver enzymes, and Low Platelet
|

