![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
144 Cards in this Set
- Front
- Back
|
What are the three primary forces that must be considered when evaluating a fracture and a fracture repair?
|
rotation
bending axial compression |
|
|
How does an avulsion fracture occur?
|
fragment distracted away by pull of tendon or ligament
tension band repair used to counter pull of muscles |
|
|
Why is open reduction essential for articular fractures?
|
direct fragment manipulation is required because joint must be aligned perfectly to preserve its function
|
|
|
What are the advantages of the open-but-do-not-touch approach to fracture stabilization?
|
preserves blood supply, leaves hematoma/callus, preserves all soft tissue attachments by not manipulating minor fragments
--> faster healing |
|
|
Name the components of an external skeletal fixator.
|
fixation pins
connecting bar single clamp |
|
|
Name the various ex fix systems.
|
KE (Kirshner-Ehmer) system: classic
Imex SK ESF Securos ESF circular (ring) fixators free form fixators |
|
|
Name & describe the different ex fix frame configurations.
|
unilateral (single bar type Ia): most common
-usually applied to medial surface of radius & tibia & lateral surface of femur or humerus unilateral double bar (double bar type Ia): stronger vs. bending unilateral 2 plane (quadrilateral type Ib): 2nd most common -applied most often to radius & tibia -modified type Ib fixator can be developed for the humerus bilateral (type II) -cannot be placed on femur or humerus b/c of adjacent body trunk -applied only to radius or tibia & are usually placed in a mediolateral plane bilateral 2 plane (type III) -cannot be applied to femur or humerus b/c of position of body wall type Ia, Ib, II, & III are successively stronger & stiffer combining external fixators w/ IM pins has gained popularity over recent years: “tie-in” configurations -to provide the strength & stiffness desired w/ complicated humeral or femoral fractures, a combination IM pin & Type Ia or Ib external fixator is often used strength & stiffness ↑ as size & number of connecting bars ↑ b/c bones are subject to bending in 2 planes (mediolateral & craniocaudal), biplanar fixators are more effective in resisting physiologic bending loads than are fixators w/ connecting bars aligned in a single plane |
|
|
Ex fix: how do you determine if a pin is not too big to be placed in a specific bone?
|
pin diameter: NOT > 25-30% of bone diameter
|
|
|
What is the optimum number of pins per fragment in an external fixator?
|
aim for 3 pins per major fragment
2 is essential, 3-4 distribute load to interface |
|
|
Ex fix: Why are triangular frame configurations stronger than bilateral frames?
|
a triangular plane (type III) provides excellent bending resistance b/c it has components in both planes
|
|
|
Ex fix: What is the best orientation of the clamp and why?
|
-↓ distance b’twn bone & fixation clamp ↑ fixator’s stiffness
-orienting clamp so that clamping bolt is closest to skin ↓ this distance |
|
|
What are some uses & properties of circular (ring) external fixators?
|
1º use: correction of limb deformities
can also be used for fx stabilization: most applicable for fractures of extremities below elbow & stifle also used for carpal & tarsal arthrodesis, bone lengthening, & bone transport small diameter (1-1.6 mm) wires thru bone (stiffened by tensioning) attached to rings around limb rings attached by threaded connecting bars the smallest ring that allows at least 2 cm in distance b’twn skin & inner circumference of ring at all point should be selected |
|
|
ex fix: Why is pre-drilling a pilot hole helpful prior to placing a pin?
|
pins are poor drills
-thermal damage & microcracking --> dead & damaged bone --> resorption & loosening pre-drill holes: slightly smaller than shaft of pin use slow insertion speeds |
|
|
What are some uses & properties of free form external fixators?
|
pins in any plane: good for irregular bone shapes (ex. mandible) or complex fx
small size: good for birds, toy breeds acrylic, epoxy putty used as connecting bars |
|
|
What are the differences b'twn KE, Imex, & Securos external fixator systems?
|
KE: metal clamps & connecting bar
Imex: adjustable clamp: can add at any location, carbon composite connecting bar Securos: adjustable clamp, metal stiffening plate |
|
|
internal fix: Explain how a “buttress” implant is different to a “neutralization” implant
|
neutralization
-neutralizes physiologic forces acting on a section of bone that has been anatomically reconstructed & stabilized -bone shaft rebuilt, 1º implant helps reduce load on fx -bone & implant both take the load thru the bone buttress -no real contact b’twn proximal & distal 1º fragments -implant must bear all load until bone heals -2º bone healing -much more common w/ biological fx management |
|
|
Why should an IM pin never be used in the radius?
|
joint surfaces over both surfaces of bone, so no good way to pet pin in w/o damaging carpus
|
|
|
Why is one cerclage wire not mechanically useful?
|
need a minimum of 2 wires: 1 wire alone provides poor resistance to bending, fragments can rotate around 1 wire
|
|
|
Why are two pins usually used for avulsion fragments?
|
2 small pins or K wires used to prevent rotation of fragment
|
|
|
Explain how all three forces acting on a fracture are resisted by an interlocking nail
|
very strong in bending: nail provides bending support
bolts resist compressive & rotational forces: locked w/ screws both proximally & distally |
|
|
If an IM pin is use in a comminuted fracture, what other techniques could be used to counter rotation and collapse?
|
rarely used by themselves: often need external fixator or bone plate as adjunct to counter all forces
|
|
|
How many screws should engage the major fragments when using a plate?
|
must attach w/ screws: 6 cortices per main fragment
3 screws above & 3 screws below fx: go thru cortex twice |
|
|
internal fixation: Explain the difference between a “lag” screw and a “position” screw.
|
lag screw: used to apply compression b’twn fragments
-screw doesn’t engage near cortex (only far cortex across fx) -can use glide hole or partially threaded screw -optimal position of lag screw in perpendicular to fx line -threads of screw will glide thru hole in near cortex (glide hole) & purchase bone in far cortex (thread hole) -as the threads purchase far cortex, fx line is compressed position screw: used to hold 2 fragments in anatomic alignment when compression would cause 1 fragment to collapse into marrow cavity |
|
|
What is the first step in the development of osteochondrosis?
|
begins w/ failure of endochondral ossification in either physis or articular epiphyseal complex that is responsible for long bone epiphyseal formation
|
|
|
An osteochondrosis lesion becomes painful following what event?
|
pain caused by inflammation in subchondral bone d/t contact w/ joint fluid
|
|
|
Which 4 joints can develop OCD?
|
shoulders, elbows, stifles, & hocks
|
|
|
What is the most common site for OCD of the stifle?
|
piece of cartilage & subchondral bone is usually observed that involves medial surface of lateral femoral condyle (most common) or medial femoral condyle
|
|
|
Name 3 breeds commonly affected with UAP.
|
large growing dogs (labs, rotties, GSDs, etc.)
|
|
|
What is the youngest age at which UAP can be diagnosed?
|
anconeal process does not fuse to ulna until 4-5 mo
dx of UAP cannot be made before then |
|
|
What is the short and long term prognoses for joint function after surgical removal of a FCP?
|
short term: possible surgical complications: iatrogenic infection, soft tissue irritation by implants
guarded px for return to full function b/c of progressive DJD, which develops regardless of tx method most dogs function as pets & are only intermittently lame |
|
|
Name 4 breeds commonly affected with FCP.
|
labs, rotties, Bernese mountain dogs, newfies, goldens, GSDs, chows
|
|
|
Should dogs with FCP be used for breeding?
|
both hereditary & environmental influences play part in development: animals should not be used for breeding
|
|
|
Which portion of the humeral condyle is most commonly affected with OCD?
|
flap of cartilage covering a defect in surface of trochlear ridge of medial humeral condyle is usually seen
|
|
|
What is the prognosis following surgical removal of a shoulder OCD flap in a young dog?
|
44 dogs treated surgically to remove cartilaginous flap: 75% had excellent function, 22.5% had good function on long term evaluation
after sx, most dogs become sound w/in 4-8 wks |
|
|
What can happen to a flap that breaks free from an OCD lesion?
|
free cartilage flaps can lodge in joints & may ↑ in size w/ calcification until they become radiographically visible joint mice (some flaps are eventually resorbed)
does not apparently cause clinical signs until a loose cartilage flap forms |
|
|
Why should you strongly consider radiographing both shoulders of a young dog that you suspect has OCD?
|
despite unilateral lameness, condition is often bilateral
|
|
|
What is the most common site for OCD of the tarsus in all breeds except Rottweiller?
|
large piece of cartilage & subchondral bone usually observed involving medial (most common) or lateral trochlear ridge
|
|
|
What is the most common traumatic joint luxation?
|
coxofemoral joint is most common joint to be traumatically luxated
|
|
|
Why are good quality radiographs important before deciding the best course of treatment of a luxated joint?
|
rads: look for small bone fragments
|
|
|
How can we tell whether or not the medial and lateral collateral ligaments of the elbow joint are intact after reduction of a dislocated elbow?
|
valgus stress test: used to evaluate integrity of medial collateral ligament
-patient in lateral recumbency -1 hand used to stabilize femur while other grasps distal tibia & applies upward force (abduction) -if medial joint restraints are torn, opening of medial joint line is apparent varus stress test: used to evaluate integrity of lateral collateral ligament -patient in lateral recumbency -1 hand used to stabilize femur while other grasps distal tibia & applies inward force (adduction) -if lateral joint restraints are torn, opening of medial joint line is apparent |
|
|
What structure is damaged when there is hyperextension of the carpal joint?
|
damage to palmar fibrocartilage --> hyperextension (acute or chronic)
|
|
|
What are the general surgical principles of arthrodeses?
|
remove articular cartilage: want bone on bone
bone graft: take bone from elsewhere (usually proximal humerus) & pack around arthrodesis site rigid stabilization in a functional position |
|
|
Describe one suture pattern that would be appropriate to use for a severed medial collateral ligament of the stifle in a 50 lb dog.
|
locking loop suture pattern w/ small non-absorbable suture used to repair ligament
|
|
|
What is the difference between strain and sprain when describing an injury?
|
strain: injury to tendon or muscle resulting from overuse or trauma
sprains: injuries to ligaments (attach bone to bone) |
|
|
What are the characteristics of a 1st degree sprain?
|
mild
only a few fibers involved little pain or swelling no bone lesions no instability tx: rest + NSAIDs |
|
|
What are the characteristics of a 2nd degree sprain?
|
moderate
most fibers damaged: some failed, some stretch painful, swollen, inflamed rarely bone lesions little instability |
|
|
What are the characteristics of a 3rd degree sprain?
|
severe
complete rupture pain, swelling, inflammation avulsion fragments on bone possible joint instability/dysfunction |
|
|
How are joint luxations usually diagnosed?
|
PE: CREPI
|
|
|
What are the general tx principles for shearing injuries?
|
flush w/ dilute chlorhexidine: 60cc syringe, needle, 3 way stopcock
debride apply wet to dry bandage: change q 24 hrs for 3-4 d. (until granulation bed forms) |
|
|
What are tx options for elbow luxation?
|
most luxated elbows can be reduced w/ closed manipulation if treated w/in 1st few days after injury
after reduction, elbow placed in extension w/ a soft padded bandage & spica splint for 2 wks |
|
|
What is tx of choice for carpal luxation or subluxation?
|
arthrodesis (hard to get fibrocartilage to heal)
need for sx based on presence of persistent hyperextension or presence of fractures |
|
|
How can OCD be prevented in puppies?
|
diet: large dog growth formulations (control calories, high protein, balance minerals)
-applies to all puppy orthopedic conditions exercise: avoid vigorous stimulated activities (lots of jumping, etc.) select the right parentage |
|
|
How is OCD diagnosed?
|
pain of joint manipulation & evidence of subchondral bone changes are usually sufficient to recommend arthrotomy
|
|
|
What is the pathogenesis of OCD?
|
thickened cartilage --> cleft develops --> cartilage separates from calcified base --> flap edge breaks free --> subchondral bone in contact w/ synovial fluid --> pain, sclerosis, inflammation, release of pro-inflammatory molecules --> synovitis, pain
|
|
|
What are ways in which cranial crucial ligament injury may present?
|
acute injury: less common
semi-acute: look for bilateral dz chronic: assoc. w/ development of DJD “paraplegic”: bilateral: 2nd rupture is acute & more debilitating partial tears: hard to dx in early stages |
|
|
Which band of the CCL is the primary restraint against cranial drawer motion?
|
craniomedial band is the 1º restraint against cranial drawer motion
|
|
|
What percentage of dogs are likely to have meniscal injury at the time of surgery?
|
damage to caudal body of medial meniscus seen in 50-75% of patients w/ a torn CCL
|
|
|
Clinical studies have shown that an equal percentage of dogs return to good or excellent function after all techniques for CCL replacement or reconstruction. What is that percentage?
|
80-90% have good to excellent function following sx
|
|
|
What percentage of dogs are likely to injure their opposite CCL once they have ruptured one?
|
~30-40% of affected dogs will rupture ligament on opposite leg w/in 2 yrs
|
|
|
If you elicit a “click” from the joint while evaluating range of motion, what structure might be injured?
|
clicking sound: usually d/t medial meniscal injury
|
|
|
What are the four landmarks for finger position for eliciting drawer motion?
|
landmarks: patella, fabella, tibial crest, head of fibula
|
|
|
If a dog has a painful stifle, how does he protect it as he sits?
|
“sit test”: watch dog go from standing to sitting
animal won’t want to flex the painful stifle: will plop down w/ leg out to side |
|
|
What are surgical tx options for CCL injury?
|
intracapsular reconstruction
-over the top technique extracapsular reconstruction -fabella-tibial crest suture -fibular head transposition leveling procedures -TPLO, TWO, TTA, TTO |
|
|
What are the goals of sx when treating CCL injury?
|
debride ligament fragments
check meniscus: excise damaged portions stabilize: eliminate drawer or neutralize functional drawer overall: slow progression of DJD |
|
|
What post-op care is required after repair of CCL injury?
|
+/- bandage: perhaps for 2-3 d. for extra-articular suture to ↓ swelling
strict confinement for 4-6 wks a rigorous progressive physical therapy program may enhance recovery after stifle sx -cold pack, ROM, massage, hydrotherapy (underwater treadmill), electrostimulation (to maintain muscle mass), deep heat therapy |
|
|
What is the most common direction of patellar luxation?
|
medial
|
|
|
What is the grading system for patellar luxation?
|
1: rarely clinical, needs to pushed from groove
2: frequently luxates, returns easily to groove, some tibial crest rotation -usually the most painful: patella frequently going in & out of groove --> cartilage damage, exposed subchondral bone --> PAIN 3: dislocated most of the time, can be relocated, moderate crest rotation 4: permanent dislocation, marked crest rotation |
|
|
What are indications for surgical repair of luxating patella?
|
advised in symptomatic immature or young adult patients b/c intermittent patellar luxation may prematurely wear articular cartilage of patella
indicated at any age in patients showing lameness & is strongly advised in those w/ active growth plates, b/c skeletal deformity may worsen rapidly |
|
|
What surgical procedures may be included in repair of patellar luxation?
|
to fix patella displacement: medial release, lateral retinacular imbrication (tightening), patella stabilizing suture
to fix shallow trochlear groove: trochleoplasty to fix tibial crest rotation: antirotational suture (if small amt. of rotation) or tibial crest transposition may also need to relocate origin of rectus femoris m. to fix significant femoral & tibial angulation: corrective osteotomy |
|
|
What direction would you transpose the tibial crest to correct a medial patella luxation?
|
tibial crest transposed laterally to correct a medial patellar luxation
|
|
|
What portion of the joint capsule is released when correcting a medial patella luxation?
|
release of medial retinaculum may be necessary to allow patella to stabilize in deepened trochlear groove
|
|
|
What associated anatomical abnormalities may be present in dogs w/ medial patellar luxation?
|
associated anatomical abnormalities: rotation of proximal tibia, shallow trochlear groove of femur
other possibilities: coxo vara, altered rectus femoris m. origin, bowing of femur, bowing of tibia, joint tilted |
|
|
What soft tissue injuries are fairly often associated with pelvic fractures?
|
muscle separation or avulsion of bony insertion of rectus abdominis m. & herniation of abdominal viscera may occur
bladder & urethral rupture may occur concurrent w/ pelvic fractures impaired sensory & motor functions of lumbosacral plexus or sciatic n. may result from ilial fx |
|
|
What factors are involved in deciding to treat a pelvic conservatively or surgically?
|
indications for conservative tx
most important consideration: minor fragment displacement minimally displaced, stable fractures of ilium isolated ischial or pubic fractures sacroiliac luxations & fractures w/ minimal patient discomfort & minimal displacement of the hemipelvis small dogs unstable patient unilateral fractures sx is cost prohibitive indications for surgical tx large or giant breed dogs, working dogs animals w/ concurrent orthopedic problems all acetabular fractures ilial fractures w/ suspected nerve entrapment ilial fractures w/ moderate to severe displacement & instability animals w/ bilateral pelvic limb injury ischial or pubic fractures assoc. w/ soft tissue herniation sacroiliac luxations & fractures w/ significant narrowing of the pelvic outlet animals w/ pelvic canal collapse females w/ breeding potential |
|
|
What are the potential complications of pelvic canal collapse after pelvic fracture?
|
severe pelvic canal narrowing can result in pelvic canal stenosis, which can cause obstipation & dystocia
|
|
|
Why is a neurological examination of dogs with pelvic fractures so critical? Describe the general steps of that neurological examination.
|
impaired sensory & motor functions of lumbosacral plexus or sciatic n. may result from ilial fx
neuro exam: perineal sensation, patellar reflex, withdrawal reflex (hock flexion), deep pain |
|
|
What options should you offer to the owner of a dog with a 1-day-old 3-piece acetabular fracture?
|
anatomic reconstruction of articular surface & rigid stabilization are MANDATORY to restore acetabular joint function & minimize DJD
plate & screw fixation is preferred approach for acetabular reconstruction --> ↓ pain, encouragement of early motion specially designed curved canine acetabular plate is available conservative therapy may result in less than optimal limb function |
|
|
Outline the principles of conservative management of pelvic fractures.
|
enforced rest for 1st 3 wks after injury
after 3 wks: supervised activity on a leash for additional 4 wks, w/ amt. of exercise gradually ↑ NSAIDs maintain animal on well padded bedding that is changed frequently to prevent decubital ulcers & urine scalding monitor bowel movements & give stool softeners PRN physical therapy: passive flexion & extension of hip, stifle, & tarsal joints -used to prevent joint & muscle contracture -as healing progresses, can be replaced by more active therapy (ex. swimming, walking up a grade) |
|
|
What is the "line of force" of the pelvic limb?
|
wt. of dog pulling belly down
counteracting this: femoral head --> acetabulum --> ilium --> sacroiliac joint --> sacrum fx of hip joint displaces line of force of pelvic limb: requires very good repair |
|
|
What surgical procedures are indicated for tx of:
a. sacroiliac luxations & fractures b. ilial, ischial, & pubic fractures |
a. surgical stabilization can be accomplished w/ bone screws or small IM pins
b. bone plates are the only implant that can be curved to mimic shape of lateral surface of ilium -restoring curve of ilium prevents collapse of pelvic canal |
|
|
What are the general options for repair of mandibular fractures?
|
conservative tx: tape muzzle, bonding the maxillary & mandibular canine teeth together in anatomic alignment w/ acrylic
surgical tx: interdental wires, interfragmentary wires, bone plates & screws, external skeletal fixators, acrylic fixators |
|
|
How can we make sure that proper occlusion has been re-established after mandibular fx while the patient is under general anesthesia?
|
endotracheal tube can be repositioned through a pharyngotomy incision (requires special tube that can bend w/o collapsing)
allows mouth to be completely closed during sx, which facilitates determination of adequate dental occlusion |
|
|
What are the goals of surgical repair of mandibular fractures?
|
preserve normal occlusion
restore masticatory function |
|
|
What are the indications for internal fixation of fractures in skeletally immature dogs?
|
used for following types of acute fractures:
-fractures causing rotational deformity or excessive shortening -fractures resulting in incongruency of an articular surface -fractures affecting physeal plate & thus future bone growth -fractures of femur, esp. in large breeds |
|
|
Describe or draw the five types of Salter fractures.
|
I: fx runs thru physis
II: fx runs thru physis & portion of metaphysis III: fx runs thru physis & epiphysis & is generally an articular fx (rare) IV: articular fx running thru epiphysis, across physis, & thru metaphysis V: crushing injuries of physis not visible radiographically but that become evident several weeks later when physeal function ceases |
|
|
What are the most common locations for Salter 1? Salter 2? and Salter 4 fractures?
|
I: femoral head, proximal tibia, greater trochanter, distal radius, distal femur, distal humerus
II: distal femur, femoral head, distal radius, proximal & distal tibia, distal humerus IV: distal humerus, distal femur, proximal tibia |
|
|
What are the general principles of fracture treatment in immature dogs?
|
gentle technique: approach & manipulation
-closed reduction & fixation are preferable when possible: cases must be seen early & have minimal displacement early repair: reduce physeal fractures as early as possible minimal fixation -younger the animal, the less reduction & fixation are needed -small diameter, smooth Steinmann pins or K wires are adequate fixation in most cases do NOT bridge physis w/ any fixation that prevents an ↑ in bone length short immobilization (implant removal) |
|
|
What is the general pathogenesis of radius curvus in dogs?
|
cone shaped distal ulnar physis frequently injured during forelimb trauma
Salter Harris type V crushing injury --> complete physeal closure --> shortening of ulna w/ cranial bowing, external rotation, shortening of radius w/ varus angulation of carpus |
|
|
What are some differences in bone biology b'twn immature & mature dogs?
|
growth
rapid & intense turnover & healing decreased stiffness: bone is softer d/t less mineral |
|
|
What are some options for tx of forelimb deformities in dogs?
|
conservative tx, periosteal stripping, stapling, osteotomy/ostectomy (ex. ulna), linear external fixator, plate, ring external fixator (simultaneously corrects angular limb deformities & lengthens limbs)
|
|
|
What is the classification scheme for open fractures?
|
1st degree: small (piercing) wound, inside-out
2nd degree: moderate trauma, outside-in 3rd degree: severe trauma, outside-in |
|
|
What are the principles of tx for 1st degree open fractures?
|
w/in ~6 hrs of occurrence, tx like a closed fx: “golden period”
rigid fixation: plating or ex fix cancellous grafts may be beneficial wound closure: 1º closure at sx |
|
|
What are the principles of tx for 2nd or 3rd degree open fractures?
|
bandage for a few days 1st: debridement
rigid fixation: ex fix or (sometimes delayed) plating cancellous grafts are beneficial wound closure delayed for 4-7 d. |
|
|
What are some complications associated w/ fractures?
|
fixation failure
delayed union nonunion malunion osteomyelitis fracture dz (muscle contracture & fibrosis) compartment syndrome fracture assoc. OSA re-fracture after implant removal |
|
|
What are some etiologies & causes of osteomyelitis?
|
bacterial: Staph, Strep, E. coli, Pseudomonas, Proteus, Klebsiella
fungal: Blasto, etc. viral: distemper? pathogenesis: iatrogenic, trauma, extension of local wounds, hematogenous (rare) |
|
|
What is the tx for osteomyelitis?
|
ABs based on C/S for at least 28 d., application of warm packs may be effective
if sequestra or pockets of exudate are present, drainage & debridement of necrotic tissue are necessary acute: ABs, debridement & lavage, closed suction drains or delayed surgical closure, maintain (or provide) rigid fixation chronic: entails maintaining or providing fx stability, removal of loose implants & sequestered bone, cancellous bone grafting of bony deficits, & appropriate ABs for 4-6 wks |
|
|
What is the pathogenesis of fracture dz (muscle contracture & fibrosis)?
|
quadriceps contracture occurs most commonly after distal femoral fx in young dogs
-inadequate fx stabilization, excessive tissue trauma during sx, or prolonged limb immobilization w/ stifle in extension may contribute -joint stiffness develops as result of fibrous adhesions b’twn quadriceps & fx callus -w/ time, adhesions form b’twn joint capsule & distal femur, limiting limb use & causing quadriceps muscle to atrophy |
|
|
What is the difference b'twn malunion, nonunion, & delayed union?
|
malunion: healed fractures in which anatomic bone alignment was not achieved or maintained during healing
nonunion (psuedarthroses): diagnosed when there is radiographic evidence that bone healing is not occurring or cannot occur delayed union: fractures that are uniting, although more slowly than anticipated |
|
|
What is the cause of fx associated OSA?
|
= 1º bone tumor at previous fx site
occurs d/t complicated or disturbed healing process: comminuted fractures, delayed unions, nonunions, osteomyelitis, metal ion induced carcinogenesis (Jonas intramedullary splint) |
|
|
What are signs of hip dysplasia in young animals?
|
usually sudden onset of unilateral dz --> sudden ↓ in activity assoc. w/ marked soreness of hindlimbs
difficulty rising after rest, exercise intolerance, intermittent to continual lameness (may be non-weight bearing), may be reluctant to jump up, climb stairs may have “bunny hopping” gait in rear quarters while running |
|
|
What are signs of hip dysplasia in older animals?
|
= signs d/t DJD
lameness usually bilateral difficulty rising, exercise intolerance, lameness after exercise, waddling gait, bears weight old dog that is NOT bearing wt. on hind limb: think cruciate rupture, OSA atrophy of thigh & pelvic mm --> ↑ prominence of greater trochanters shoulder mm. hypertrophy d/t cranial wt. shift & ↑ use of forelimbs |
|
|
What is the etiology of hip dysplasia?
|
multifactorial etiology: both hereditary & environmental factors involved
hip joints are normal at birth failure of muscles to develop & reach functional maturity concurrently w/ skeleton --> joint instability rapid wt. gain & growth thru excessive nutritional intake may cause a disparity of development of supporting soft tissues, leading to hip dysplasia factors that cause synovial inflammation (i.e. mild, repeated trauma) may also be important synovitis --> ↑ volume of joint fluid --> ↓ joint stability hip joint laxity & subsequent subluxation |
|
|
What radiographic views are used to confirm hip dysplasia?
|
views that give a good look at pelvis: extended VD, lateral
views that give a good look at femurs: craniocaudal horizontal beam, open leg lateral other views: dorsal acetabular rim (DAR), distraction view |
|
|
What is the Ortolani maneuver & how is it performed?
|
w/ animal is dorsal recumbency, place hands over stifles
hold femurs parallel to each other & perpendicular to table subluxate femoral head by pushing stifle toward pelvis while maintaining pressure, abduct limb as femoral head returns to acetabulum, a click will be felt most affected young dogs will have a positive Ortolani sign Ortolani sign is rarely present in older dogs d/t fibrosis of joint capsule & shallowness of acetabulum |
|
|
What is hip dysplasia?
|
abnormal development of coxofemoral joint characterized by subluxation or complete luxation of femoral head in younger patients & mild to severe DJD in older patients
|
|
|
Why is the OFA registry an underestimation of the actual number of dogs with hip dysplasia?
|
not very sensitive b/c only uses extended VD view: insensitive for detecting coxofemoral subluxation
good for ID of excellent & horrible hips, not so good for those in b'twn |
|
|
What is the dorsal acetabular rim view?
|
skyline view across dorsal acetabular rims
permits the visualization of the dorsal acetabulum, the weight bearing portion of the acetabulum advantage of this position is correlating what is found on palpation under anesthesia to what is evidenced on radiographs |
|
|
What are complications assoc. w/ total hip replacement?
|
luxation, infection, implant loosening, fx adjacent to implants
|
|
|
What are tx options for young dogs w/ hip dysplasia?
|
conservative therapy
triple pelvic osteotomy (4-8 mo.) juvenile pubic symphysiodesis (< 5 mo.) |
|
|
What are tx options for older dogs w/ hip dysplasia?
|
conservative therapy
total hip replacement femoral head & neck ostectomy |
|
|
When should closed reduction be attempted for coxofemoral luxation?
|
closed reduction should be attempted before open reduction in most animals unless there is radiographic evidence of severe hip dysplasia or fx
best to attempt as soon as general anesthesia can be administered safely |
|
|
What are indications for open reduction of coxofemoral luxation?
|
failed closed reduction, multiple limb injuries, femoral/acetabular fx, hip dysplasia? (controversial), chronic cases
|
|
|
What is the post-op management after repair of coxofemoral luxation?
|
closed reduction: +/- Ehmer for 3-5 d., confinement for 14 d.
open reduction: +/- Ehmer for 7-10 d., confinement for 21 d. FHO: ROM, supervised exercise starting immediately post-op |
|
|
What are repair techniques for coxofemoral luxation?
|
capsule reconstruction (capsulorrhaphy): should always be performed if enough joint capsule remains
capsular imbrication & reinforcement: suture b’twn greater trochanter & cranial aspect of acetabulum o joint reconstruction joint capsule may be shredded to a degree that 1º suturing is impossible -in such cases a prosthetic capsule, toggle pin, or transacetabular pin (should be avoided if possible) can be used to maintain reduction during healing of fibrous joint capsule translocation of greater trochanter FHO or total hip replacement: if luxation is not repairable |
|
|
What is the pathogenesis of Legg Calve Perthes dz?
|
non-inflammatory aseptic necrosis of femoral head that occurs in young patients before closure of capital femoral physis
results in collapse of femoral epiphysis b/c of an interruption in blood flow after cell death occurs, reparative processes begin bone substance is weakened mechanically during revascularization period & normal physiologic wt. bearing forces may cause collapse & fragmentation of femoral epiphysis when this happens, incongruence of femoral epiphysis & acetabulum --> DJD |
|
|
What is the most common direction for coxofemoral luxation and what are the other directions of luxation?
|
typically results in craniodorsal displacement of femoral head (~75%)
ventrocaudal displacements occur less often |
|
|
What instrument or equipment can be used to cut the femoral neck when doing an FHO?
|
to ensure accuracy of bony cut, predrill series of 3 or more holes along line of ostectomy
use osteotome & mallet to complete cut OR use an oscillating saw |
|
|
What is tx of choice for Legg Calve Perthes dz?
|
FHO
|
|
|
What is the incidence of bilateral disease in dogs with Perthes disease?
|
occurs bilaterally in 10-17% of patients
|
|
|
What nerve should you be concerned about when dealing with a femoral fracture?
|
sciatic n.
|
|
|
For each device listed, what forces do they resist
a. external fixator b. bone plate c. interlocking nail d. IM pin |
a. rotation, compression, and bending (to a certain degree)
b. rotation, compression, and bending (to a certain degree) c. resists rotation, compression, and bending d. resists bending, but not compression or rotation |
|
|
What 4 radiographic views are done to most accurately examine the hip joint?
|
Lateral pelvis, ventrodorsal pelvis, distraction view, and dorsal acetabular rim (DAR) view
|
|
|
How does the Triple Pelvic Osteotomy create stability in a dog with hip dysplasia?
|
The procedure is designed to rotate the acetabulum, improving dorsal coverage of femoral head. Reestablishing congruity of joint and correcting forces acting on joint.
|
|
|
Why is the carpal joint a good candidate for arthrodesis?
|
There is limited motion in the joint. Also, there are not a lot of soft tissue structures on surgical approach. In addition, the complexity of the support structure makes it difficult to reconstruct.
|
|
|
What are some possible repair techniques for fractures of the radius?
|
ESF: Ia, Ib, II, III, ring
bone plate |
|
|
What are some possible repair techniques for fractures of the humerus?
|
IM pin + cerclage
interlocking nail bone plate ESF: Ia, Ia + IM pin |
|
|
What are some possible repair techniques for fractures of the femur?
|
IM pin + cerclage
interlocking nail bone plate bone plate + IM pin ESF: Ia, Ia + IM pin |
|
|
What are some possible repair techniques for fractures of the tibia?
|
ESF: Ia, Ib, II, III, ring
bone plate IM pin + cerclage (careful of CCL insertion) interlocking nail (careful of CCL insertion) |
|
|
What are some indications for ESF?
|
well suited for stabilization after closed reduction of comminuted fractures
free form: pins in any plane: good for irregular bone shapes (ex. mandible) or complex fractures ring fixator: fractures below elbow or stifle |
|
|
What are some indications for cerclage?
|
ideal for long oblique fractures: fx line > 2x bone diameter
only works when all fx fragments interlock to rebuild shaft: NOT for comminuted fractures NOT a sole repair method |
|
|
What is an indication for skewer pin & cerclage?
|
used to compress short oblique fractures
NOT a sole repair method |
|
|
What are some indications for bone plates?
|
good for axial skeleton, fractures involving joints, & patients with fx dz
any time you want post-op comfort & early limb use must shape to bone surface requires open reduction: can use OBDNT |
|
|
What bones can be repaired w/ IM pins or interlocking nails?
|
humerus, femur, tibia (if careful of CCL insertion)
NOT radius |
|
|
What type of Salter Harris fx is this?
|
type 1
|
|
|
What type of Salter Harris fx is this?
|
type 1
|
|
|
type 1
|

What type of Salter Harris fx is this?
|
|
|
type 2
|

What type of Salter Harris fx is this?
|
|
|
type 3
|

What type of Salter Harris fx is this?
|
|
|
type 4
|

What type of Salter Harris fx is this?
|
|
|
type 5
|

What type of Salter Harris fx is this?
|
|
|
type III
|
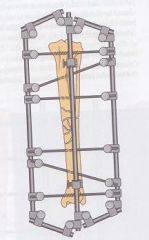
What type of external fixator if this?
|
|
|
type II
|
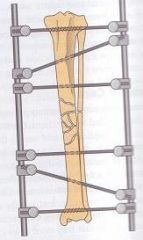
What type of external fixator if this?
|
|
|
type Ib
|
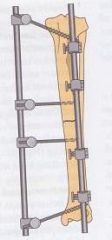
What type of external fixator if this?
|
|
|
type Ia
|
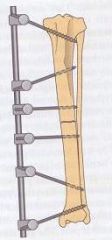
What type of external fixator if this?
|

