![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
what is immune mediated disease
|
a broad term which covers any disorder in which tissue damage is due to the immune response.
|
think broad!
|
|
|
name the types of hypersensitivity skin reactions and what each one means in a few words.
|
Type I : immediate
(anaphylactic) eg midge bite Type II : cytotoxic antibody dependant Type III : immune complex mediated Type IV : cell-mediated (delayed) |
1st and last are partly in their name!
I C I C David!! immediate/ cytotoxic/ Immune complex/ cell mediated delayed!!!! |
|
|
explain the path. of type 1 hypersensitivity, give 2 examples and what are the 2 possible outcomes and which is more common
|
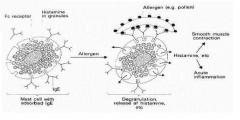
Type I : immediate (anaphylactic) eg midge bite or food allergy
cell fixed Ab ( mainly IgE bound to mast cells or basophils) -animals B cells produces IgE ( after being stimulated by TH2 cells) which is specific for the foreign antibody -IgE binds to mast cell membranes -re-exposure to antigen -mast cell degranulation ( eg histamine causes acute inflammation and smooth muscle contraction and others ) -pruritis, self-trauma,eosinophils and mast cells results in....... severe systemic reaction ( anaphylaxis) or mild local reaction- more common note this is the basis for atopy |
think IgE and think mast cells !!
|
|
|
explain the path. of type 2 hypersensitivity and give examples
|

Type II : cytotoxic and anitbody dependant
>exposed antigens on body tissues ( endogenous or hapten attached to cell surface) >binding of antibody (IgG or IgM) +/- complement-cytotoxicity or cytolysis (( aka ADCC- antibody dependant cell mediated immunity ) eg exposure of wrong blood type! / haemolytic anaemia/ thyroiditis |
think blood type!
|
|
|
explain the path. of type 3 hypersensitivity and give examples
|

Type III : immune complex mediated.
Ab directed against soluble antigens - Ab-Ag complexes deposited in tissue - causes complement fixation and neutrophil chemotaxis- tissue damage due to enzymes (proteolytic and hydrolytic ) ... either systemic (aka serum sickness) or local ( aka arthus reaction) eg a vaccine reaction which may be either. note a vaccine reaction could also be type 1 or a reversion to virulence of an attenuated organism. also cutaneous vasculitis |
think phagocytoses
|
|
|
explain the path. of type 4 hypersensitivity
|
Type IV : cell-mediated (delayed) ( NOT dependant on Ab)
THE SAME PROCESS AS THE RESPONSE OF CELL MEDIATED IMMUNITY TO A MICROBIAL INFECTION the tissue damage will occur if the stimulus is great or unusually persistent. ( if really persistant then a granuloma will form ) 'sensitisation phase '-TH1 cells are sensitised after the ininial contact with the antigen via APCs ( Macs or langerhans cells) 'effector phase'>re-exposure to antigen-sensitised TH1cells causes release of cytokines ( aka lymphokines) -macrophages and cytotoxic T cell infiltration which cause cell damage. |
|
|
|
how can the defense response cause tissue damage. how is the process started in any nornal response. and which cell usually tries to control this.
|

Pathogen-activated DCs present pathogen-derived antigens to T cells and promote the differentiation of naive T cells to various subtypes of effector CD4+ ( TH1 or 2) and CD8+ T cell.
1. excessive inflammation ( uncontrolled pro inflammatory cytokines released from innate immune cells and TH1 cells). 2.allergic reactions ( eosinophilia - uncontroled TH2 cell response). 3. host cell killing ( CD8 cytotoxic t cells and NK Cells) regulatory T cells usually try to control these effects |
|
|
|
what is the role of CD4 (TH1 and TH2) cells and what determines the level of production of each
|

-CD4+ T helper 1 (TH1) cells secrete interferon-γ (IFN-γ ), which activates the anti-microbial activity of macrophages and helps B-cell production of IgG antibodies and helps NK cells and is associated with autoimmunity.
Whereas TH2 cells provide help for B-cell production of IgG, IgA and IgE and is assocaited with alergic reactions ( eosinophil recruitment). production is determined by the receptors activated on the naive T cell by the dendritic cell |
think of the pic!!
|
|
|
what is the role of CD8 T cells
|
CD8+ T cells lyse host cells infected with viruses, intracellular bacteria or parasites.
AKA cytotoxic t cells |
aka.....!!!
|
|
|
what is the role of regulatory T cells in normal individuals
|
In normal individuals, regulatory T cells (both natural regulatory T cells circulating in the periphery and those induced by infection) help to control these effector functions and the associated damage to host tissues.
in lecture 2 ... T reg cells are stimulated at a steady state which maintains homeostasis and during infection different t cells called T effector memory t cells will be activated to proliferate. over all maintain a balance. |
in the name! they control others!!
|
|
|
what are the 2 types of immune mediated disorders and can they overlap. define them both
|
hypersensitivity reactions and autoimmune disease and they can overlap
hypersensitivity- an exagerated response to a mild pathogen or one which does not even exist autoimmune disease- a specific humoral or cell mediated response against the body's own tissue. |
|
|
|
draw the process of type 1 hypersensitivity to a food allergy
|
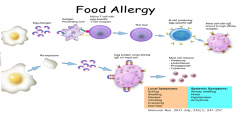
note small amount needed second time
|
|
|
|
type 1 hypersensitivity ( immediate ) may either result in
anaphylaxis or mild local reaction- more common- . what is anaphylaxis and what parts of the body might it involve |
severe systemic allergic reaction , which is rapid in onset and may cause death.
skin +/- mucosal tissue, res. system, GI, decreased BP- note these are species dependant |
one of them is the title of the lecture series!
|
|
|
is it true that not all anaphylactic triggers may cause IgE production. give an example and other examples.
|
yes- some triggers stimulate the mast cells directly eg snake venom .
other triggers include food/meds/unidentified |
|
|
|
describe how mast cells are activated and degranulated, how does this affect the response and what is a sensitized mast cell?
|

a senstized mast cell is just a mast cell which has IgE bound to its Fc receptors on its membrane.
When the specific antigen cross links 2 IgE molecules which are bound to a sensitized mast cell the mast cell will degranulate and activate production of the Arachidonic acid pathway from the plasma membrane and signal for cytokine gene activation. The immediate response is due to the immediate degranulation eg of histamine- vasodilation, vascular leakage, smooth muscle spasm. The 'late' phase response is mediated by cytokines and prostaglandins and leukotrienes derived from the arachidonic acid from the plasma membrane |
|
|
|
give examples of type 1 hypersensitivity in animals (immediate). what is the most common in SAs
|
Atopic Dermatitis and flea bite hypersensitivity are the most common of all skin diseases and the most common type 1 hypersensitivity in SAs
others are other insect bite hypersensitivities eg midges causing sweet itch in horses also drug eruptions and food allergy |
|
|
|
what is canine atopic dermatitis and what is a common allergen which is part of the cause.
how do they present clinically |
the definition of an atopic syndrome is a predisposition toward developing certain allergic hypersensitivity[1] reactions.
a multifactorial and muli- layered disease. Involves genetic predisposition and environmental factors. The clinical presentation is associated with IgE usually directed against environmental allergens ( commonly house dust mites ). It is Type 1 hypersensitivity. pruritic dermatitis ( face, feet and ventrum ) and otitis possibly with conjuctivitis. much cell trauma ( so histo is variable) |
define a atopic syndrome!
|
|
|
which breeds are predisposed to canine atopic dermatitis
|
westies / cairns/ boxers/ scotties
|
|
|
|
list some specific factors of skin in atopic dermatitis
|

overall a defective epidermal barrier which allows allergens to penetrate.....
mutation in the FLG gene (which codes for profilaggrin which is broken down by proteases to Filaggrin and then to AAs which are natural moisturising factors.) limited and discontinuous lipid bylayer as there is a decrease in synthesis of lipid lamellae. increased resident protease activity within eipdermis and also from pathogens ( eg house dust mites and staph)-cleave corneodesmosome junctions. decreased anti-microbial peptides ( altered expression) a predominant Th2 cell response.( the allergens are presented by DC cells to helper T cells which recruit more CD4 cells. The activated DC cells and IL 4 released from CD4 cells can promote TH1 to TH2 cells. The many TH2 cells will release pro-inflammatory cytokines and increase IgE) |
i.e what makes it an 'atopic' syndrome!!
|
|
|
what insects can cause insect bite hypersensitivity and in which animals is it seen. In which animals is it considered atopic and why. What class of hypersensitisation is it.
|
Horses and SAs
( considered an atopic ( predisposed towards it ) in horses) caused by fleas/ biting midges/ black flies and mosquitoes. mostly type 1 but can be type 4 |
|
|
|
describe the class of hypersensitivity seen in flea allergy dermatitis the legions seen and the region of the body they are found in.
|
type 1 and / or type 4.
pruritic papular dermatitis. dorsal lumbosacral area, neck, inner thighs and Ab. |
|
|
|
describe allergic contact dermatitis pathogenesis. what regions are usually affected.
|

type 4 ( delayed type cell mediated) hypersensitivity.
a small molecule binds to epidermal proteins to form the allergen which is capable of causing an immune response. areas with less hair especially the ventrum. also feet/legs/ perineum/scrotum/chin/pinnae. |
|
|
|
with type 4 hypersensitivity ( cell mediated and delayed ) what would lead to a granuloma formation and draw the cellular structure of a granuloma
|

prolonged stimulation by allergen ( more than 2 weeks)
As the response develops, macrophages fuse to form multinucleated giant cells, and fibroblasts are stimulated to synthesize collagen, resulting in the formation of a granuloma. |
|
|
|
what is hypersensitivity
|
when the immune response over reacts to a foreign antigen.
|
|
|
|
what is cutaneous vasculitis. what sp is it seen in, how does it happen
|
a type 3 hypersensitivity reaction.
rare except in dogs and horses. Ab-Ag complexes form due to infection or drugs and lead to immune complexes being deposited inthe walls of small blood vessels. Causes oedema, heamorage and ischaemia |
|

