![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
CVAD – NOTES/ POSSIBLE TQ
|
X
|
|
|
When should a CVAD be used instead of a peripheral catheter? Examples.
|
- Need high fluid vol./high caloric needs (TPN)(Burns, Cancer, Sepsis)
- Extremely irritating meds (Cancer, Sepsis) - Hemodynamically unstable (Sepsis) - complicated surgical procedures (CABG) |
|
|
Why is CVAD chosen for certain meds or TPN?
|
- Inserted in large vessels w/ high blood flow
- Concentrated or irritating solutions are rapidly diluted by the blood in these vessels. |
|
|
Central Venous Access Veins
|
see pic
|
|
|
Which blood vessels are typically chosen for the CVAD? Why?
|
-Internal jugular vein, subclavian vein, & femoral vein (last choice)
|
|
|
Why are pts w/ Crohn’s disease, ciliac disease, & tropical sprue good candidates for a central line?
|
These are mal-absorption diseases. Unable to absorb nutrients from the GI tract. So TPN is ordered
|
|
|
Why would pts w/ acute pancreatitis or extensive bowel surgery require a central line?
|
they need “bowel rest”, so TPN is ordered
|
|
|
What are some goals of Parenteral Nutrition?
|
-establish a positive nitrogen status
-improve nutritional status -maintain muscle mass -promote weight maint. or gain -enhance the healing process |
|
|
What happens if the nitrogen status in negative?
|
the body breaks down muscle for energy
|
|
|
Nursing considerations for parenteral nutrition:
|
-Assess the site & dressing
-Assess for fluid volume overload -Order changed daily -Hang D10 or D5 if TPN or PPN (respectively) “run out” before more is made -Check blood blucose -Know if it is continuous or cycled |
|
|
What is the difference between Continous vs Cycled Parenteral Nutrition
|
-Continous is given all day
-Cycled is generally given at night when sleeping, eat regular meals during the day |
|
|
How often is an ordered changed?
|
daily – very pt specific, pt’s status & requirements could change often
|
|
|
What is done when TPN or PPN “runs out” before the next bag is prepared?
|
hang a D10 bag until the TPN is ready – the pancrease is used to the TPN or PPN w/ a lot of dextrose and will keep producing the same amount of insulin as if it’s still getting it. The D10 will hold it over until the TPN comes.
|
|
|
Categories of Central Lines are related in terms of:
|
length of therapy
|
|
|
What are the categories of Central Lines?
|
1. Short-term = up to 30 days
2. Intermediate = 30 – 45 days 3. Long-term = greater than 45 days |
|
|
Which is the choice Central Line Catheters?
|
PICC: Peripherally Inserted Central Catheter
|
|
|
Types of Central Line Catheters?
|
-PICC: Peripherally Inserted Central Catheter
-Non-tunneled -Tunneled -Implanted Ports |
|
|
Describe Non-Tunneled & Tunneled Central Line Catheters
|
-Non-Tunneled
-sutured in place at the insertion site, directly through the skin & into the vein -catheter & attachments protrude directly - multiple lumens -Tunneled -Long-term -goes under skin for a length before hit vein |
|
|
Nontunneled CVC Line
|

see pictures
|
|
|
Tunneled CVC Line
|

see pictures
|
|
|
Where are nontunneled percutaneous CVCs inserted?
|

-jugular, subclavian, or femoral veins
|
|
|
Why would tunneling be preferred over non-tunneling?
|
less chance for infection
|
|
|
What is required for all Central Lines before beginning use? Why?
|
X-Ray – ensure hit superior vena cava
|
|
|
Describe a Multilumen Subclavian Catheter
|
-non-tunneled percutaneous central catheter
-short-term, up to 30 days -has 1 – 4 lumens -increased risk of infection from that of tunneled |
|
|
Possible complication (other than infection) w/ catheter in subclavian vein?
|
pneumothorax
|
|
|
When would you use the femoral vein for a central catheter?
|
If the subclavian line is contraindicated (critical care & ER settings)
|
|
|
What primary considerations go with a Femoral Line?
|
-VERY short term, 1 – 2 weeks
-move location as soon as possible |
|
|
Why is the Femoral line the least desireable?
|
-High risk for complications & infections
-accounts for most catheter-related blood stream infections |
|
|
How long can a PICC line stay in?
|
3 – 6 months
|
|
|
PICC Line
|
see pictures
|
|
|
PICCs are only replaced as needed, what reasons might cause a change?
|
no longer patent or site looks infected
|
|
|
Why are some benefits to using a PICC?
|
-less risk of complications (infection/pneumothorax) due to peripheral insertion
-cost effective while providing adequate hemodilution for meds |
|
|
Two types of Tunneled Central Catheters?
|
-open ended (Hickman/Broviac)
-valved (Groshung catheters) |
|
|
Why would Tunneled Central Catheters be the choice for Dialysis pts?
|
because they are long-term (several years)
|
|
|
What is special about the Groshung catheter?
|
some have one-way pressure valves (no need to clamp)
|
|
|
Hickman Catheter
|

see pic
|
|
|
Groshung Catheter
|

see pic
|
|
|
Port-a-Cath, # of lumen & length of use?
|
-can stay in for several years
-has one lumen -may have an internal pump to release meds slowly |
|
|
Port-a-Cath, type of needle to access?
|
Huber needle
|
|
|
Implanted Ports
|
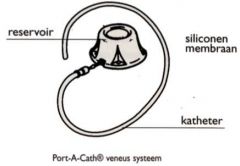
see pics
|
|
|
Complications with CL?
|
-sepsis/infection (mask & sterile technique)
-thrombosis (blood clot) -phlebitis (redness, irritation) -Air embolus, more common in CL than peripheral (from flushing/priming, etc.) -occluded |
|
|
Which type of central catheter has least risk of blood-stream infections?
|
implanted ports
|
|
|
Interventions if CL is occluded
|
-sit up, raise arm
-cough -TPA [tissue plasmin activator (small anti-coagulant)] -change cap -do not force |
|
|
What should you check if pt is uncomfortable?
|
-infusion (going to vein, rate too fast?)
-pt position -pt’s circulatory status -pt anxiety |
|
|
How often should a Central Line be flushed?
|
q8h & after each use (check hospital policy)
|
|
|
Size syringe & how much to flush with?
|
-10cc syringe, flush q/ 3-10 cc or NS
-After blood draws, flush w/ 20cc |
|
|
Flushing w/ valved vs. non-valved catheters
|
-non-valved, maintain pressure w/ plunger while clamping (necessary)
|
|
|
Main concern when changing a valved cap on valved catheter?
|
-clamp when changing
-flush new cap before attaching |
|
|
When removing a central line, what position should pt be in?
|
lying flat
|
|
|
Indications for removal of a CL?
|
-improvement of status
-infection -length of time |
|
|
Complications when removing a CL?
|
-Catheter not intact
-resistance |
|
|
Difference in concentration between TPN &PPN (hypertonic, hypotonic & isotonic)?
|
-TPN is hypertonic while PPN is isotonic.
|
|
|
TPN contains the 3 primary components of nutrition: ______, ______& ____________? As well as: ______, __________, & _________?
|
- protein, carbs, & fats
-electrolytes, vitamins & trace elements |
|
|
What would be the best position of the pt when working with a PICC line? Why?
|
-comfortable positions w/ arm extended from the body below heart level.
-reduce risk of air embolism |
|
|
What’s the main purpose of the clear dressing?
|
protects site, prevents accidental dislodgement or removal of needle
|
|
|
To do if PICC is dislodged during dressing change?
|
-If not all the way out, notify the PCP. Will most likely want X-ray to see location of line’s end. Before X-ray, reapply dressing so doesn’t further dislodge.
|
|
|
To do if purulent drainage is noted at the insertion site when dressing is removed?
|
-obtain a culture, clean area, reapply dressing, notify PCP (before sending culture).
-prevents line from being open while notifying PCP and the culture is obtained w/o removing the dressing again if PCP wants the culture. -if PCP doesn’t want the culture, discard it |

