![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
|
Categories of Back Pain (7)
|
1. Mechanical (arthritis, spinal stenosis, muscular, disk disease)
2. Inflammatory spondyloarthropathies associated with inflammatory bowel disease, psoriasis, reactive spondylitis (following certain infections), and ankylosing spondylitis. 3. Active infections (such as epidural abscess, usually via hematogenous spread from another infection site) 4. Fracture (osteoporotic or traumatic) 5. Neoplastic (from bony metastasis of another primary cancer, or from a primary bone tumor) 6. Referred (often from abdominopelvic sources) 7. Functional (often associated with psychiatric diagnoses) |
|
|
Back Pain cancer types (mets) and quality
|
prostate, lung, breast, thyroid
focal pain - worse when pt is reclining/sleeping |
|
|
Risks for AAA
|
Male, HTN, smokers, >55yo
|
|
|
Duration of backpain classification
|
acute <6 weeks
subacute 6-12 weeks chronic >12 weeks |
|
|
Reiters Reactive Arthritis
|
Involves: eye, urinary system, hands/feet
appear 1-3wks post infection Eye = uveitis/conjunctivitis and is generally an early finding Possibly precursor to other joint diseases |
|
|
Triamterene + HCTZ
|
Diuretic (water pill) - used for HTN and edema in patients that are important to avoid low K levels. (K sparing)
|
|
|
No fever suggests?
|
less likely to be an infectious etiology
|
|
|
Radicular pain
|
This referes to pain that radiates like in sciatica where it goes down the leg.
|
|
|
Exam in leg w/ pain
|
Look for symetry to r/o radicular pain at hip level
MOTOR L3-4: inversion of the foot L4-5: big toe dorsiflexion L5-S1: foot eversion SENSORY L4: sensory changes around the medial malleolus L5: sensory changes around the third metatarsal S1: sensory changes around the lateral heel DTR L3-4: decreased patellar reflex L5-S1: decreased medial hamstring change S1-S2: decreased Achilles reflex S2-S4: decreased anal wink |
|
|
Alternative to straight leg raise
|
Seated leg raise is a confirmatory test for straight leg raise. Used to weed out the functional leg pain.
|
|
|
Prognosis of mechanical low back pain
|
90% of mechanical low back pain and 50% of acute back pain with sciatica resolve within a one-month period without specific treatment
-Acetaminophen or NSAIDs may help though muscle relaxants & narcotics are without efficacy - Spinal manipulation may help - Heat & Ice help in acute stage - PT is recommended at 1mo from onset |
|
|
Indication surgery in back pain
|
1. instability of vertabrae from trauma
2. tumor causing neurologic compromise 3. cauda equina syndrome |
|
|
Causes of spinal stenosis
|
Can progress to cause spinal stenosis:
1. Spondylosis (degenerative spine changes), 2. facet arthropathy, 3. bulging disks, and 4. hypertrophy of the ligamentum flavum, |
|
|
Chest pain differential
|
Cardiovascular
-Ischemic (ACS) vs non ischemic Chest wall - MSK - Skin (herpes) GI - esophageal - pancreatobiliary - Peptic ulcer disease Pulmonary - vasulature - parenchyma - airways (bronchospasm) - pleurisy Mediastinal Dz - inflammation - tumor - air present Psych (Anx/dep/panic/munchausen) |
|
|
Chest Pain Ddx in cardiovascular realm (2-4)
|
Ischemic
- Hyperadrenergic (cocaine, amphetamine, pheochromocytoma ) - Prinztmetals (atypical variant angina) - Stable/Unstable angina - Acute MI Non-Ischemic - Pericarditis - Aortic dissection - Valvular heart dz - arrhythmia |
|
|
Chest Pain Ddx in gastrointestinal realm (3)
|
1. Esophageal
- GERD - esophagitis - esophageal dysmotility 2. PancreoBiliary - atypical cholangitis - atypical cholecystitis - pancreatitis 3. PUD |
|
|
Chest Pain Ddx in pulmonary realm (4-2)
|
1. Vasculature
- PE - Cor pulmonale/pulmonary HTN 2. Parenchyma - PNA - pleural effusion 3. Airways (bronchospasm) - asthma - COPD 4. Pleura - plurisy - spon. pneumo |
|
|
What to do if suspect ACS ?
|
- Aspirin unless contraindicated
- serial ECG - Cardiac troponins q6-12H (detectable for 24H post myocyte death biut takes 4-6H after insult) - Nitroglycerin (ONLY if CURRENTLY having CP) - +/- o2 supplementation |
|
|
Chest pain Ddx menominc
|
-- CHEST PAIN --
Cocaine/Costochondritis Hyperventialtion/Herpes Zoster Esophagitis/Esophageal spasm Stenosis of aorta Trauma Pulmonary embolism Pericarditis/Pancreatitis Angina/Aortic dissection/Aortic aneurysm Infarction (myocardial) Neuropsychiatric dz |
|
|
Suspected ACS history points
|
Pain timing and location
-atypical presentation MC in women, elderly, DM Associated symptoms - nausea, diaphoresis, SOB Risk Factors - Smoking, HTN, HLD, DM, FHx, vascular dz |
|
|
Suspected ACS PE points
|
VS (HR and BP)
Cardiac Exam (murmur, S3, S4) |
|
|
PNA - PE and HPI
|
fever, crackles, decreased breath sounds, cough
|
|
|
How to construct a summary statement
|
A summary statement should:
1. Be a concise statement that accurately highlights the most pertinent features in a case without omitting any significant points: • Epidemiology (age, gender, risk factors) • Key clinical findings (symptoms, signs, data) 2. Transform specific details into medical terms (example: "tachycardia" rather than "heart rate of 150"). 3. Use qualifying adjectives to describe key findings better: • Diagnostic considerations: diffuse vs focal; monoarticular vs polyarticular • Severity: mild vs severe • Temporal pattern: acute vs chronic Ultimately, a good summary statement should provide the basis for developing an appropriate differential diagnosis. |
|
|
What are the componets of this summary statement?
Susan Johnston is a 60-year-old obese woman with a past history of hypertension and dyslipidemia and a family history of cardiac disease who presents with a three month history of intermittent burning anterior chest pain associated with SOB, but only variably associated with exertion. Other than hypertension, her physical exam is unremarkable. |
The ideal summary statement concisely highlights the most pertinent features without omitting any significant points. The summary statement above includes:
Epidemiology and risk factors: 60-year-old obese woman with history of hypertension and dyslipidemia and family history of cardiac disease. Key clinical findings about the present illness using qualifying adjectives and transformative language: burning chest pain three months of intermittent symptoms association with SOB variable association with exertion physical exam unremarkable other than hypertension Top DDx = GERD/ANGINA |
|
|
Aortic Dissection - PE and HPI
|
tearing/radiating to the back, risks = HTN/smoking/over age 60
|
|
|
Pericarditis - PE and HPI
|
worse on inspiration, positional alleviation (foward), non exertional, ECG=diffuse concave upward ST seg. + depressed PR seg.
|
|
|
Pulmonary Embolism
|
Pain= sharp + pleuritic, Common presentation is CP + SOB, ECG = 70% abnormal (S1Q3T3 -or- RBBB -or- T wave inversion)
|
|
|
Classical Angina
|
retrosternal CP onset w/ exertion and relieved by rest or nitroglycerin
|
|
|
Stable angina vs unsatble angina vs Acute MI
|
Acute MI - rupture of plaque that occludes with myocyte necrosis (onset is once and immediate onset)
Stable vs. Unstable Angina Angina occurs when myocardial oxygen demand exceeds supply. When angina is thought to be present it is important to further characterize it as stable angina vs. unstable angina since these two syndromes are managed very differently. Stable angina pectoris is a predictable pattern of chest discomfort that usually occurs with exertion or extreme emotion. It is relieved by rest or nitroglycerin in less than 5-10 minutes. Unstable angina is a more serious condition characterized by chest pain that occurs at rest or with increasingly less exertion. New onset angina (within 4-6 weeks) and angina that has worsening severity, frequency or duration is also c |
|
|
Treatment in suspected unstable angina
|
Sublingual then IV nitro - unless hypotenive
Beta blocker decrease hearts work unless hypotenive |
|
|
Leads for anterior wall MI
|
ST segment elevation V1-V4 compared to PR segment
|
|
|
What is TIMI Score (Thrombolysis In Myocardial Infarction)
|
Used to determine medical tx vs. early intervention
Higher score = Higher rates of events in the next 14 days (all cause mortality, new/recurrent MI. severe recurrent ischemia requiring revascularization) 1 point if YES 0 if NO (Max is 7pts) ------------------------------- Age ≥65 years Presence of at least three risk factors for coronary heart disease (CHD) Prior coronary stenosis of ≥50 percent Presence of ST segment deviation on admission ECG At least two anginal episodes in prior 24 hours Elevated serum cardiac biomarkers Use of aspirin in prior seven days |
|
|
TIMI Score percentages of events next 2weeks
|
Score of 0/1 – 4.7 percent
Score of 2 – 8.3 percent Score of 3 – 13.2 percent Score of 4 – 19.9 percent Score of 5 – 26.2 percent Score of 6/7 – 40.9 percent |
|
|
Leads for Inferior MI
|
ST segment elevation 2, 3, aVF compared to PR segment
|
|
|
Leads for lateral wall MI
|
ST segment elevation in 1, aVL, V5, V6 compared to PR segment
|
|
|
Leads for septal wall MI
|
ST segment elevation in V1, V2 compared to PR segment
|
|
|
CP and STEMI -or- new LBBB on ECG warrants what?
|
Dx coronary angiography
goal of angioplasty within 90 minutes (time is myocardium) |
|
|
Fibrinolytic -vs- Angioplasty
|
Angioplasty is preferred if expert operator within a certain time frame. However fibrinoloytic may be best given time frame of onset and time to availability for angioplasty.
|
|
|
Contraindications to Fibrinolytic tx
|
Major are: bleeding or hemorrhagic stroke
- Strong suspicion of dissection of the aorta Pericardial effusion - Active gastrointestinal or other internal bleeding - Brain tumor, arteriovenous malformation, or aneurysm - Ischemic stroke in preceding 6 months (a verified transient ischemic attack (TIA) is an exception) - Previous intracerebral hemorrhage or subarachnoid hemorrhage - Intracranial procedure or recent head trauma - Severe known bleeding disorder: coagulation abnormality, thrombocytopenia, etc. |
|
|
GP IIb/IIIa inhibitor
|
abciximab or eptifibatide - improve oputcomes in STEMI patients despite their increase risk of bleeding
|
|
|
What are the complications of acute MI
|
Complications of acute myocardial infarction include:
-arrhythmias (bradyarrhythmias and tachyarrhythmias) -reduced ventricular function -cardiogenic shock (hypotension) -papillary muscle dysfunction with acute valvular dysfunction -ventricular free wall rupture -recurrent thrombosis |
|
|
ACS what meds should they be on when discharged?
|
Aspirin (A) therapy should be started promptly in all patients with a suspected acute coronary syndrome and should be continued indefinitely.
- Administer aspirin, 160 to 325 mg, immediately upon presentation with suspected acute coronary syndrome (ACS) and continue daily aspirin at a dose of 75 to 325 mg/day. Clopidogrel (B) should be continued for a year after stent placement in addition to aspirin to prevent stent thrombosis. β-adrenoceptor blockers (C) should be started early in all patients with suspected ACS unless there are significant contraindications. - Begin with oral β-blockers within a few days of the event, if not begun acutely, and continue them indefinitely. Goal heart rate is <70 and blood pressure <130/80. HMG CoA reductase inhibitors (statins) (D) should be started while in the hospital in patients with ACS with a target LDL of <100. Sublingual nitroglycerin (F) should be sent home with patients post-admission. ACEi - only if clinical HF or anterior |
|
|
GERD - PE and HPI
|
Pain is "burning", not a/w exertion, but a/w obesity
|
|
|
Define Typical Angina
|
The Three Criteria for Typical Angina
Substernal chest discomfort with a characteristic duration and features Exertional in nature Relief with rest or nitroglycerin |
|
|
Define Atypical Angina
|
Atypical Angina
Patients who have diabetes, women, and the elderly are more likely to present with atypical features. Occasionally they will present with only weakness or shortness of breath on exertion. Those symptom are considered "anginal equivalents". |
|
|
Value of an ECG
|
With an electrocardiogram, you can:
1. rule out an ST elevation MI, 2. look for evidence of prior infarction (pathologic Q waves) 3. occasionally, make other diagnoses such as pericarditis. |
|
|
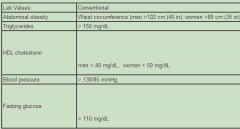
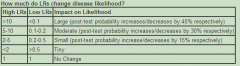
Met X Criteria from ATP3 study
|
|
|
|
What is seen in a positive stress test (heart)? What would be the next step?
|
An example is on ECG =
2mm downsloping ST segments in leads II, III, aVF, V2, V3, V4 and V5 Next step = Cornoary angiogram to determine candidacy for per-cutaneous interventions |
|
|
Rx treatment for angina ?
|
- Beta blockers (A) decrease myocardial oxygen consumption by slowing heart rate and decreasing blood pressure, and thus reduce angina.
- Calcium channel blockers (B) dilate coronary arteries and increase coronary blood flow while also decreasing myocardial oxygen consumption. - Nitrates (D) dilate systemic and coronary arteries and venodilatory effects also decrease cardiac work. |
|
|
Side effects of HCTZ
|
dehydration, hyponatremia, hypokalemia, renal dysfunction, increases serum uric acid which may precipitate gouty attack
|
|
|
Side effects of ACEi (Lisinopril)
|
cough, renal dysfunction, angioedema, hyperkalemia
|
|
|
Side effects of Statins
|
myositis, myalgias, hepatitis (requires initial measurement of transaminases and an initial creatinine phosphokinase (CPK) level. Additional CPK levels are indicated with symptoms of muscle soreness.)
|
|
|
Signifigance of Fever temperature and if present?
|
Fever is an important part of the history in a patient with cough because it makes an infectious cause more likely. The severity of fever (e.g., 100.4 vs. 104.0) is not specific and therefore does not help distinguish between different causes of inflammation. Fever is both detrimental and beneficial. It leads to increased metabolism, which can cause dehydration, promote inflammation, and inhibit function of proteins at very high temperatures. The primary potential benefit of fever is to decrease bacterial reproduction and growth, because most bacteria function best in a limited temperature range. Patients are unable to accurately assess their temperature based on touch.
|
|
|
What is Pleurisy and PE findings ?
|
If the chest pain is due to a pulmonary process, then you can be certain that the pleura are involved and inflamed (because the pulmonary parenchyma is insensate). Such a condition is called pleurisy and the chest pain is worse with deep inspiration or coughing, which is most commonly unilateral.
|
|
|
Significance of hemoptysis ?
|
Hemoptysis is a non-specific finding of cough. It is important to determine whether a patient has massive or life-threatening hemoptysis, which is defined as greater than 100 mL over a 24-hour period. Patients often do not estimate the amount of their hemoptysis accurately, so it is difficult to make this determination by history alone.
|
|
|
What are chills and rigors and physiology?
|
Chills are non-specific and can occur in any inflammatory state that leads to cytokine release. Certain cytokines cause the hypothalamus to change the body's temperature set point to a higher level. To achieve this new set point, peripheral blood vessels vasoconstrict, and this can give the patient a sense of being cold. The body also may try to increase the temperature set point by having the muscles contract (shivering) and the patient may feel this as rigors
|
|
|
Significance of wheezing ?
|
Wheezing may suggest reactive airways disease, such as chronic obstructive pulmonary disease (COPD), but it is non-specific. If an infection causes bronchiolitis or significant mucus production, wheezing can occur even in patients without a history of asthma or COPD
|
|
|
Lung Exam Key Points
|
Lungs (C)
Careful percussion and auscultation of the lungs is critical to assess for the presence of dullness, increased or decreased breath sounds, crackles, rhonchi, or other abnormal sounds. It is important to remember to listen over the right middle lobe, which will be missed if your exam is done on the posterior thorax only. The right middle lobe is an anterior and lateral structure so the best place to listen to it is lower portion of the right anterior thorax. |
|
|
Orhtostatic Hypotension Defintiion and etiology ?
|
Orthostatic hypotension
Although expert definitions of orthostatic hypotension vary, any of the following indicate an inability to compensate for postural changes: - fall in systolic blood pressure of >20 mm Hg with standing - increase in pulse of >30 beats/min with standing - inability to stand long enough for vital signs because of dizziness Causes of orthostatic hypotension can include medications, hypovolemia, cardiac insufficiency, and diabetic neuropathy. |
|
|
What is egophony ?
|
Egophony (assess for consolidation)
Ask the patient say "eeeee" for about 3-5 seconds. Auscultate the lungs and listen for a change in the character of the sound from that of "E" to "A." |
|
|
Difference between Vesicular and Bronchial Breath sounds ?
|
Vesicular breath sounds
Normal breath sounds in the lung, characterized by a long inspiratory phase followed by a short expiratory phase. Bronchial breath sounds Compared to vesicular breath sounds, bronchial breath sounds have a louder, shorter inspiratory phase and louder, prolonged expiratory phase. This is a normal finding when heard over the trachea. However, when bronchial breath sounds are heard in a location other than the trachea, it is suggestive of pulmonary consolidation (C) (meaning the alveoli are full of something other than air such as pus, water, or blood). |
|
|
What to do if suspect decreased lung sounds?
|
decreased breath sounds, percuss out the lungs. Dullness to percussion in an area of decreased breath sounds suggests pleural effusion (A), whereas hyperresonance suggests pneumothorax (B).
|
|
|
Writing a summary statement example.
|
The ideal summary statement concisely highlights the most pertinent features without omitting any significant points. The summary statement above includes:
1. Epidemiology and risk factors: 71 year-old man with history of tobacco use 2. Key clinical findings about the present illness using qualifying adjectives and transformative language: fever with chills productive cough dyspnea hemoptysis right pleuritic chest pain hypoxia orthostasis tachycardia borderline hypothermia evidence of RLL consolidation. Example is: Mr. Groszek is a 71 year-old man with a history of tobacco use who presents with a two-day history of fever with chills, productive cough, dyspnea, hemoptysis, and right pleuritic chest pain. His vital signs reveal hypoxia, orthostasis, tachycardia, and borderline hypothermia, and there is evidence of RLL consolidation on lung exam. |
|
|
What do you see in acute aspiration pneumonitis ?
|
Typically occurs in patients who are debilitated, have neuromuscular problems affecting swallowing, or with altered mental status including excessive alcohol use.
Patients often have concomitant periodontal disease and more indolent symptoms of a putrid cough, fever, and dyspnea evolving over days to weeks. |
|
|
Lung Cancer Presentation ?
|
Lung cancer can obstruct the diameter of a bronchus leading to a post-obstructive pneumonia, thus both diagnoses can sometimes co-exist. Lung cancer alone would not cause symptoms of infection and pulmonary findings of consolidation.
Hemoptysis is associated with pulmonary malignancy, but it is neither sensitive nor specific for this diagnosis |
|
|
What is the role of CBC in PNA ? SIRS criteria.
|
CBC (A) has limited utility in terms of the diagnosis of pneumonia. Patients with pneumonia usually have an elevated white blood cell count with a neutrophil predominance and a left shift (i.e., increased percentage of bands), but the absence of these do not rule out pneumonia. The CBC can be helpful in assessing the severity of pneumonia because a WBC <4.0 cells x103/μL (<4.0 cells x109/L) or >12.0 cells x103/μL (>12.0 cells x109/L) is a criterion for the systemic inflammatory response syndrome (SIRS). SIRS suggests the patient has a very severe infection.
|
|
|
Tests to order in suspected PNA?
|
CBC, Gram stain & sputum cx, blood cx, CXR
|
|
|
When to order a ABG ?
|
The two situations where an ABG can be useful are:
(1) when a clinician is on the fence about intubating a patient, and (2) when there is a concern the patient is retaining excess carbon dioxide. |
|
|
How do you know if CXR is of good quality ?
|
RIP
Rotation - Measure the distance of each clavicle from the spinous processes at that level. If they are equidistant, the patient is not rotated. Inspiration - A good inspiratory effort is present if you can count nine posterior ribs within the lung fields before you reach the diaphragm. Penetration - The ability to visualize the intervertebral spaces within the heart boundaries. If the intervetebral space has a similar density to the vertebrae themselves, then the film is underpenetrated and all the shadows will appear denser than they actually are. |
|
|
Healthcare associated PNA compared to CAP.
|
Risk factors for healthcare-associated pneumonia
- Hospitalization for two days or more in the preceding 90 days (A) - Home infusion therapy (including antibiotics) (B & D) - Chronic dialysis within 30 days (C) - Home wound care (D) - Residence in a nursing home or extended care facility (E & G) - Family member with multidrug-resistant pathogen |
|
|
CURB 65 Score
|
Prognostic score for PNA severity that can be used to aid in the decision of whether or not to hospitalize patients with community-acquired pnuemonia.
CURB-65 stands for: Confusion blood Urea nitrogen (>19 mg/dL) Respiratory rate (>30 breaths per minute) Blood pressure (systolic <90 or diastolic <60 mmHg) age (65 or older) |
|
|
Characteristics of TB ?
|
Tuberculosis is unlikely because it rarely presents acutely and the location of the infiltrate is usually in the upper lobes
|
|
|
What types of PNA are highly contagious ?
|
Influenzae and TB types but NOT bacterial
|
|
|
Common complications of PNA ?
|
Bacteremia, Sepsis, Pleural Effusion
|
|
|
When to order CT in a PNA patient ?
|
The chances for an alternate diagnosis (e.g., pulmonary embolism, malignancy) are low, based on the initial history and physical exam findings.
If after 72 hours, he does not seem better or is getting worse, a chest CT could be reasonable to assess for complications such as cavitary disease or smaller pleural effusions not visualized on chest x-ray. |
|
|
Does pneumovax decrease PNA rates ?
|
pneumococcal vaccine (Pneumovax) has not shown any reduction in the risk of developing community-acquired pneumonia, but it can reduce the risk of invasive disease; including bacteremia, meningitis, or infection of other sterile sites.
|

