![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
97 Cards in this Set
- Front
- Back
|
Aging causes
|
Oxidative Stress, Free radicals, cellular damage, slow cell manipulation, loss of tissue elasticity that affects most organs, loss of physiologic reserve (decreased kidney function), Atherosclerosis, Degnerative disorders, Psychologically people become very habitual
|
|
|
Mortality
|
Females 84
Males 83 |
|
|
compression of morbidity
|
Onset of morbid disease to death
- area between the curves contains 90% of the healthcare $ |
|
|
Bullet
|
Things that you do that result in a physical finding
"lungs are clear" |
|
|
Element
|
historical finding- symptoms that you write down
"smoker, non-somoker, etc" |
|
|
medical decision making
|
Includes assesment and plan- shows responsible decision making
|
|
|
Pain QRST
|
o Pain: PQRST
Provocation, Quality, Region radiation, Severity, Temporal pattern |
|
|
o Chief complaint
|
o Chief complaint
|
|
|
o Medications
|
o Medications: include dosage and frequency (how much and how often)
|
|
|
o Allergies
|
o Allergies: list the adverse effects to differentiate intolerance
|
|
|
o Past/Family/Social
|
o Past/Family/Social 3 elements
Past Medical History • Address the issues that they bring up with Physical findings, etc. |
|
|
o ROS
|
o ROS- 10 systems with 3 elements each including negatives
|
|
|
o Physical Exam
|
o Physical Exam 9 systems with 3 bullets each
Inspection Palpation Percussion Auscultation Combine eyes with ENT and mouth |
|
|
o Impressions
|
o Impressions: Reflect the highest risk factors (HTN, Chest Pain)
|
|
|
o Plan
|
o Plan: reflect the highest risk/decision making (order x labs, order x test, admit, call x)
|
|
|
o Do Not Say
|
o Do Not Say “Unremarkable or None, WNL” Say unabtainable, blah blah
|
|
|
o Directives
|
o Directives: DNR report/religion
|
|
|
Points in the Geriatric H/P
|
Chief Complaint/Pain/PQRST
medications Allergies PMH FMH SH ROS Physical Assessment Plan |
|
|
Detrusor pressure
|
60cm H2o
|
|
|
Normal Bladder Volume
|
400-500mL
|
|
|
Residual Volume
|
<200mL
>200= overflow incontinence |
|
|
Requirements of continence
|
Cognitive function
Moblility and dexterity Environment Motivation |
|
|
Bladder parasympathetic innervation
|
Parasympathetic- Cholinergic- Bladder Contraction and urination: S2-4
• Anticholinergics for spastic bladder- Get dry mouth, etc, don’t want to give to Elderly |
|
|
Bladder sympathetic innervation
|
Sypmathetic- αAdrenergic- Bladder relaxation, sphincter contraction: T11-L2
• αAdrenergic blocker for obstruction- BPH |
|
|
Bladder Somatic innervation
|
Somatic- voluntary pelvic floor muscular contraction: Pudendal Nerve
• Kegels- start emptying bladder and stop intermittently |
|
|
hyperactive/hypersensitive bladder
|
Failure to store
o Hyperactive bladder/Hypersensitive bladder: Detrusor Instability, Hypersensitive bladder UTI irritation in the lining will make detrusor contracts and you can’t help it. Detrusor instability- muscle decides to just go off on its own. |
|
|
Incompetent sphincter
|
Failure to store
o Incompetent sphincter- Gal whose got 10 kids with a relaxed pelvis bends down to pick up a sack of groceries and coughs at the same time. Pudendal N is important here! Throw in that this same lady has been having burning sx when she urinates: UTI on top of it. |
|
|
Failure to store categories
|
Hyperactive/Hypersensitive bladder
incompetent sphincter |
|
|
Failure to empty categories
|
Underactive bladder/overactive sphincter
Obstruction |
|
|
Underactive bladder/overactive sphincter
|
Failure to empty
o Underactive bladder/ Overactive Sphincter: Spinal Cord trauma or lesion |
|
|
Obstruction
|
Failure to empty
o Obstruction: BPH is most common problem in older males. Male takes antihistamine and ends up in the ER begging for a catheter. |
|
|
Types of urinary incontinence
|
Acute and Chronic
|
|
|
Acute Urinary Incontinence
|
o Acute- Transient or reversible factors are present
Factors: (DRIP) Delirium; Restricted Mobility or Retention; Infection, inflammation, fecal impaction; (DKA) Polyurea, pharmaceuticals • Pharmaceuticals- diuretics; pshycotropics; anti-cholinergics (OTC antihistamines), narcaotics and CCBs impair contractility |
|
|
Categories of chronic urinary incontinence
|
Stress
Urge Overflow Functional |
|
|
Stress incontinence
|
• Females: Poor anatomical support/ urethral dysfunction due to many factors
• Males: Sphincter damage from prostate surgery or radiation therapy o Tx: (kegels, Bladder training), αAdrenergic drugs, estrogen, surgery |
|
|
Urge Incontinence
|
Urge: “gotta go … oops, too late”
• Local GU conditions that irritate the inside of the bladder: Stones, obstruction, Chronic infection, adjacent inflammation o “Old lady with urgency, dysruia, frequency: has a few wbcs in the urine, culture shows no growth b/c she drinks cranberry juice- Bug won’t grow. Abx” • CNS disorders: Stroke, dementia, parkinsonism, spinal cord lesions w/ impaired symp innervations • Idiopathic: detrusor instability without underlying disorders o Tx: Behavioral therapies (kegels, Bladder training), bladder relaxant anticholinergic drugs |
|
|
Overflow Incontinence
|
Overflow “gotta go … oops, too late but it’s a Growing problem, not a Going problem.”
• Anatomical Obstruction: BPH, urethral stricture, large cystocele • Poor contractility: DM, Spinal cord injury with impaired Parasymp innervations • Neurogenic: detrusor-sphincter dyssynergy o The bladder doesn’t contract so you have a large residual and small expulsion volume. Pt will randomly just “dribble” urin. o Tx: Surgery, Catheterization, Cholinergic Agonist, αAdrenergic antagonists |
|
|
Functional Incontinence
|
Functional
• Chronic impairments of Cognitive function, mobility, dexterity (can’t physically do it) • Environmental Factors • Psychological Factors o Tx:, Garments, Pads, Catheters, Behavioral therapy: Scheduled toileting, Habit training, Prompted voiding |
|
|
o Pt develops urge incontinence with painless hematuria
|
o Pt develops urge incontinence with painless hematuria: Think cancer- do cytology/culture and send to urologist.
|
|
|
Chronic Catheterization Indications
|
• Chronic Catheterizaiton indications: Significant irreversible urinary retention; Skin disorders; Patient comfort/preference, immobility
o Using intermittent reduces UTIs |
|
|
o 1. Gotta Go Gotta Go, oops it’s too late. Bladder culture neg, PVRV: 0
|
Classic Urge Incontinence
|
|
|
o 2. Gotta Go Gotta Go, oops it’s too late. Bladder culture neg, PVRV: 400cc
|
Obstructive incontinence
|
|
|
o 3. Sneezing/going up stairs, urinalysis normal, PVRV: 0.
|
Stress incontinence
|
|
|
o 4. Dribble all the time, urinalysis normal, PVRV 400cc, Digital Rectal BPH.
|
Overflow incontinence
|
|
|
o 5. Younger married lady with one kid, hope to have more, had to go a lot over the last 3 days, burns, 30wbc/hpf, PRV:0.
|
UTI urge incontinence
|
|
|
o 6. Carrying groceries and sneezing I dribble, recently increased frequency, burns when pee, PVRV: 0, 20wbc/hpf.
|
UTI and Stress incontinence.
|
|
|
Myopia
|
Nearsighted
|
|
|
Hyperopia
|
Farsighted
|
|
|
Astigmatism
|
distorted vision
|
|
|
Presbyopia
|
inability to focus on near objects due to aging
|
|
|
Accomodation
|
• Accommodation- the lens “rounds up” by the contraction of ciliary muscles (loosening the zonules) while the pupil becomes smaller to see near objects (this is difficult conceptually)
|
|
|
Convergene
|
eyes move together so they both see close objects
|
|
|
• Presbyopia-
|
• Presbyopia- impaired accommodation- it’s a lens problem, they get old and hardened and the ciliary body can’t contract as well- difficulty focusing on near objects.
o Tx: Reading glasses or bifocals, it is acceptable to send them to walmart or the optometrist. |
|
|
Cataracts
|
• Cataracts- “Dirty Glasses,” Makes driving at night especially difficult- “Christmas trees.”
o Increase w/age, DM, smoking, EtOH o Tx: Phacoemulsion w/ intraocular lens implants Opacification w/ blurring post tx- YAG laser capsulotomy • Darnit- looks like my cateracts came back |
|
|
Macular Degeneration
|
• Macular Degeneration- m/c cause of blindness in the elderly
o Peripheral vision saved (excellent), central loss Predisposed: age, genetics, smoking, HTN, fair skin o Dry- drusen (yellow products of metabolism) accumulate UNDER the macula o Wet- Drusen + angiogenesisis and choroidal neovascularization (wet= new bvs), the worst o Tx: Beta Carotene (CI in smokers), VitE, VitC, Zinc Laser phototherapy to tx the neovascularization (wet macular degeneration) Intra-vitreal VEGF injection |
|
|
Diabetic Retinopathy
|
o Ischemia + neovascularization (tiny vessels in the cup) + microaneurysms + hemorrhage
o Annual Opth exam o Control glucose and HTN |
|
|
Glaucoma
|
• Glaucoma- 2nd m/c cause of blindness in elderly
o Central vision saved “tunnel vision” Increased incidence w/family history, AAs o Optic nerve head damage ( may or may not have high intraocular pressure) Increased pressure is due to Aqueous drainage impairment Cup/disk is usually < 1:2 • Glaucoma- >1:2 (much greater) |
|
|
Open Angle Glaucoma/ Closed Angle
|
o Open angle- drainage is slow, asymptomatic, slow subtle peripheral vision loss
Tx: BB eyedrops o Closed angle- drainage is blocked, acute and symptomatic, Sx: eye pain, headache, noticeable vision deterioration, nausea and vomiting May be provoked by Myadriatics, etc. recognize Sx. Emergency Tx required: iridectomy o Tx: Beta-blocker eyedrops, increase drainage, decrease production (epi, pilocarpine, Pgs) |
|
|
Eye Compare and Contrast
|
• Compare and Contrast
o Presbyopia- need cheaters- get around 40yo o Cataracts- dirty glasses: Lens implant with following YAG o Macular degeneration- most common cause of blindness in the elderly- central vision loss, preserved peripheral vision o Glaucoma- can be acute or subtle, Generally tunnel vision, can cause vision loss. |
|
|
Low vision rehab
|
• Low vision rehab
o Magnification, improved lighting, optical devices w/ training to use eccentric (off center) viewing, talking devices, Braille. |
|
|
Conductive hearing loss
|
• Conductive Hearing loss
o Cerumenosis- thicker, drier, more adherent cerumen o Middle ear pathology: tympanosclerosis, otosclerosis (fusion of the ossicles within the innerear) |
|
|
Sensorineural hearing loss
|
• Sensorinerual hearing loss: Generally from past exposure but could be from drugs or physical damage
o Presbycusis- symmetrical and bilateral loss of High Frequency (no need to yell, just articulate) o Phonemic regression- permanent loss of hearing at CNS due to lack of stimulation If a person gets a hearing aid, but their brain has forgotten high pitches, they won’t hear them even with the aid. |
|
|
Audiometry
|
• Audiometry
o Conductive hearing loss: Air conduction needs to be louder than bone conduction to be heard o Sensorineural: air and bone conduction loudness is the same Frequency change: High frequencies are heard less (like presbicussis) o Consonant sounds are in the >1000hz range which is difficult for geriatric hearing (PBZT) |
|
|
Amplification
|
• Amplification
o Cheap= worse than nothing (better to have nothing than a cheap-o) o Digital (best and not covered by medicare) |
|
|
Cognitive impariment exam
|
Examination:
• Critical questions in the newly confused patient: How long has this been going on, How abruptly did it start? Has the patient’s functional status changed? If the situation is progressing, how fast is it? |
|
|
Geriatric Delerium
|
Geriatric Delirium- Tripping balls; Confusional state + altered consciousness and attention
• Signs/Sx o Acute illnesss- Caused by direct physiological consequence of a general medical condition, drug withdrawal, or sundowner syndrome. Etiologies include metabolic, toxic, septic, hypoxemic, electrolyte imbalance, fever, glucose, etc. o Excess Sympathetic activity (Tach, diaphoresis, tremor, mydriasis, HTN) • Exam: Check vitals, SaO2 and/ or ABGs, CBC, CMP, UA, etc |
|
|
Geriatric dimentia types
|
Vascular
Alzheimers parkinsons CJD C Lewy bodies |
|
|
Vascular dimentia
|
• Vascular dementia: Stroke, mini stroke, trauma, etc. Check Hx and look for focal neurological sign.
o Had DIA- memory drops, has another, memory drops again |
|
|
Alzheimers
|
• Vascular dementia: Stroke, mini stroke, trauma, etc. Check Hx and look for focal neurological sign.
o Had DIA- memory drops, has another, memory drops again |
|
|
Geriatric Depression/Pseudodimentia
|
• Signs, SX
o Depressed mood o Diminished interest/pleasure in activities o Wt/Sleep changes o Psychomotor agitation or retardation w/loss of energy o Indecisiveness, poor concentration, thoughts of suicide or death |
|
|
Depression: Very important Associated Diseases
|
• Very Important Associated diseases: Cushings, HypOthyroidism (with other sequelae), Hyperparathyroidism, Hypogonadism, Addisons disease, Cerebral tmors, Viral infections, Stroke
o Pt with hair falling out, wearing sweats in the middle of the summer in the desert, complaining of a memory problem: Order TSH, Hypothyroidism. |
|
|
Mini Mental Status Exam
|
• 30 is gold standard
o Draw parallellagram, >27 normal, <20 moderate, <17 severe o Draw clock at 4:20 |
|
|
Compare and Contrast Dimentia, Depression, Delerium
|
Dimentia- aggressive cognitive decline, often the pt forgets that he forgets
Depression- vegetative sx, flat affect, vegetative sx, Get up and Go, got up and left. Delerium- tripped out, acute onset, hallucinations, delusions |
|
|
o 75yo widow gives a detailed account of her poor memory ever since the death of her husband 6 months ago.
|
Pseudodimentia with depression
|
|
|
o 70yo man’s wife who is complaining of his worsening memory over the past couple years and increased irritability and gets lost driving the car. He most likely has
|
MOST likely Alzheimers
|
|
|
o 76yo man’s wife complains that his memory had never been the same since his previous doctor gave him “rat poision” for several spells of confusion. Had TIAs with atrial fibrillation with irregularly irregularly heartrate.
|
He most likely has MultiInfarct dementia
|
|
|
o Depressed 80yo widow complains that her memory has worsened over the past 6mo. She has pedal edema, cold intolerance, easy bruisability, exercise intolerance
|
Hypothyroidism depression
|
|
|
o Healthy 70yo man drank a little more than usual at the club where he goes every night. He then fell and fractured his hip which was pinned 3 days ago. Nurse calls b/c he is agitated and claims that the CIA has bugged his hospital.
|
This guy has delirium and sees snakes/etc.
|
|
|
Consequences of falls
|
• Mortality 60-70% consequence of injury d/t fall
• Morbidity: fracture (5-10%); soft tissue injury (30-40%); subdural hematoma; hypo/hyperthermia; undiscovered fall (rhabdomyolysis renal failure); lost confidence; pt/family anxiety; expensive • LOST INDEPENDENCE – Falls number 1 reason for lost independence Long Term Care |
|
|
Etiology of Falls
|
Etiology of falls:
• 37% Accidents/environment • The other 63% are medical issues: o Weakness/balance; drop attack (sudden movement of head/neck) o Dizziness/vertigo o Orthostatic hypotension (drugs that cause that) o Syncope o Drugs: TCAs, anti-psychotics, benzos, diuretics, laxatives, diltiazem |
|
|
Pt with risk of falls
|
• LE weakness increases risk by 400%
• Hx of falls risk • Gait/mobility disorder • Meds |
|
|
Sentinel Event
|
Falling -
|
|
|
Post fall evaluation
|
• Vitals c orthostatic BP (should not see systolic BP drop >20mm)
• Px: sensory fxn; evidence of trauma, CV, musculoskeletal, neuro and gait evaluation |
|
|
Spastic hemiparesis
|
People with hemiparesis often have difficulties maintaining their balance due to limb weaknesses leading to an inability to properly shift body weight. This makes performing everyday activities such as dressing, eating, grabbing objects, or using the bathroom more difficult. Hemiparesis with origin in the lower section of the brain creates a condition known as ataxia, a loss of both gross and fine motor skills, often manifesting as staggering and stumbling. Pure Motor Hemiparesis, a form of hemiparesis characterized by sided weakness in the leg, arm, and face, is the most commonly diagnosed form of hemiparesis.[1]
|
|
|
Scissor gait
|
This gait pattern[2] is reminiscent of a marionette. Hypertonia in the legs, hips and pelvis means these areas become flexed to various degrees, giving the appearance of crouching, while tight adductors produce extreme adduction, presented by knees and thighs hitting, or sometimes even crossing, in a scissors-like movement while the opposing muscles, the abductors, become comparatively weak from lack of use. Most common in patients with spastic cerebral palsy, usually diplegic and paraplegic varieties, the individual is often also forced to walk on tiptoe unless the plantarflexor muscles are released by an orthaepedic surgical procedure.
|
|
|
Steppage Gait
|
o Steppage (Lower motor neuron disease- Neuropathies)
|
|
|
Ataxic Gait
|
posterior column disease; cerebellar degeneration; peripheral neuropathy)
People with cerebellar ataxia may initially present with poor balance, which could be demonstrated as an inability to stand on one leg or perform tandem gait. As the condition progresses, walking is characterized by a widened base and high stepping, as well as staggering and lurching from side to side.[1] Turning is also problematic and could result in falls. As cerebellar ataxia becomes severe, great assistance and effort are needed in order to stand and walk.[ |
|
|
Parkinson Gait
|
Parkinsonian gait is characterized by small shuffling steps and a general slowness of movement (hypokinesia), or even the total loss of movement (akinesia) in the extreme cases.[2][3][4] Patients with PD demonstrate reduced stride length and walking speed during free ambulation while double support duration and cadence rate are increased.[5][6][7][8] The patient has difficulty starting, but also has difficulty stopping after starting. This is due to muscle hypertonicity.[9]
|
|
|
Gait assistive devices
|
o Assistive devices
3-4 Wheel walkers (For: ataxia, hemiparesis, scissor gait) 2 wheel walkers (For: Parkinson’s) Cane: (For: antalgic gait) Maladaptive device (ataxic gait) |
|
|
Understand the difference between IADLs and bADLs
|
IADLS: SHAFT
shopping, housekeeping, accounting, food preparation/meds, telephone/transportation BADLs: DEATH Dressing, Eating, Ambulating, Toileting, Hygiene |
|
|
What is most likely to put you in the nursing home?
|
o what’s likely to put you in the NH is falls, mobility disorders, falls, incontinence, anxiety, depression
|
|
|
Photocoagulation
|
tretment for wet diabetic macular degeneration
nota goodthing or wet macular degeneration in diabetics b/c you are sacrificing some vision when you do that but you are doing it to not have the vessels break but you lose some vision at the macula with this. |
|
|
Vasular dimentia: Review
|
someone with atrial fib or some other reason, carotid stenosis, or whatever, multiple TIA, or just one good stroke.
|
|
|
Depression: review
|
Depression- vegetative sx, happens to ppl that get alzheimers or another poor diagnosis.
• Sx: get up and go got up and left, I don’t know-mia, get up early go to bed late, can’t go back to sleep, flat affect, diminished libido |
|
|
Delerium vs dimentia
|
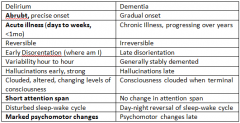
|
|
|
Age Vs Alzheimers
|
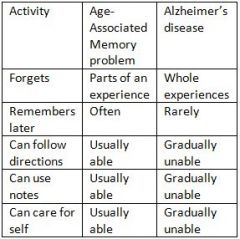
|
|
|
Dimentia vs depression
|
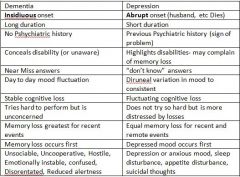
|

