![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
What is the most common mechanism of antiviral medicines?
|
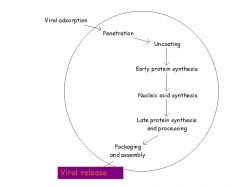
The most common mechanism of antiviral agents is interfering with DNA or RNA synthesis.
|
|
|
What is Enfuvirtide’s mechanism of action with regards to HIV-1?
|
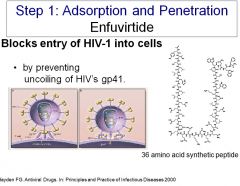
Enfuvirtide blocks entry of HIV-1 into cells (preventing adsorption and penetration) by preventing the uncoiling of HIV’s gp41.
|
|
|
Which two drugs stop influenza uncoating from happening?
|
Amantidine and Ramantidine block Influenza’s M2 protein, a proton-pumping pore, which stops influenza uncoating.
|
|
|
What drug blocks synthesis of the early proteins required to regulate CMV gene expression?
|
Fomivirsen blocks early protein synthesis of proteins for CMV. It’s complementary to mRNA, but otherwise its mechanism has not been elucidated. Given systemically, the drug is toxic. It can be injected into eyeballs of pts with CMV retinitis, and it can act locally
|
|
|
How do purine and pyrimidine analogues inhibit nucleic acid synthesis (2 mechanisms)?
|
Purine and pyrimidine analogues:
1) Block viral polymerase 2) Some also cause chain termination |
|
|
What drug would be used to treat a flare up of herpes zoster, and what are its mechanisms?
|
Acyclovir: 1) inhibits viral DNA polymerases and 2) acts as a chain terminator (same mechanisms as other purine and pyrimidine analogues).
|
|
|
What are the 5 antiviral drugs given for CMV?
|
1) Purine analogues (also effective against HSV and VZV)
a. Ganciclovir i. Mechanism of action: viral enzymes phosphorylate the drugs to the monophosphate derivative. Ganciclovir triphosphate inhibits viral polymerase b. Valganciclovir 2) Cidofovir 3) Foscarnet 4) fomivirsen |
|
|
What is the mechanism of action for Foscarnet, and what illnesses can it be used to treat?
|
Foscarnet directly inhibits viral DNA polymerase, and it can be used for HSV 1 and 2, varicella-zoster virus and cytomegalovirus.
|
|
|
What would you use to treat acyclovir-resistant HSV?
|
Foscarnet would be used to treat acyclovir-resistant HSV. It directly inhibits viral DNA polymerase.
|
|
|
How do Zanavir and Oseltamivir work, and what virus are they used against?
|
Zanamivir and Oseltamivir work by inhibiting influenza (A&B) neuraminidase, and they both:
• block the release of virus from the host cell • block spread within the respiratory tract • promote viral clumping. |
|
|
Why couldn’t you use amantadine or rimantadine to treat influenza B?
|
Amantadine and rimantidine only treat influenza A, because only influenza A has the M2 pore. Both drugs work by blocking Influenza A’s M2 proton-pumping pore.
|
|
|
What is the composition of HAART in terms of drug classes?
|
HAART is a “drug cocktail” composed of at least 3 drugs from at least 2 different classes.
|
|
|
Can you name one nucleoside reverse transcriptase inhibitor and its mechanism of action?
|
Zidovudine is an NRTI, and it works by inhibiting the unique reverse transcriptase enzyme (RNA->DNA).
|
|
|
Can you name a non-nucleoside reverse transcriptase inhibitor and its mechanism of action?
|
Efavirenz is a non-nucleoside reverse transcriptase inhibitor, and it binds to a site distant from the nucleotide binding site of reverse transcriptase enzyme and causes a conformational change that inactivates the reverse transcriptase enzyme.
|
|
|
Can you name a protease inhibitor for treatment of HIV and its mechanism of action?
|
atazanavir is a protease inhibitor, and it inhibits HIV protease. If the polyprotein remains uncleaved, the virions which are assembled are non-functional. A protease is essential for post-translational cleavage of gag and gag-pol polyproteins, producing active viral core proteins.
|
|
|
What are 3 situations where HIV infection could be prevented by HIV antiviral medications?
|
1) Maternal-infant transmission
2) Needle stick injuries 3) Sexual partner infection |
|
|
What is the definition of a noncompetitive allosteric site antagonist?
|
The allosteric site is accessible in the absence of the agonist.
|
|
|
What is the definition of an uncompetitive allosteric site antagonist?
|
The allosteric site requires receptor activation before it becomes accessible to a drug.
|
|
|
What is the definition of the therapeutic index?
|
LD50/ED50 (therefore, a higher Therapeutic index is better).
|
|
|
What does a Schild analysis do?
|
A Schild analysis provides an agonist-independent measure of the equilibrium constant, Kb.
|
|
|
What are 3 things that confer the selectivity of drug action?
|
1. Drug structure
2. Receptor distribution 3. Pharmocokinetics |
|
|
Which way do Spare receptors shift the concentration curve?
|
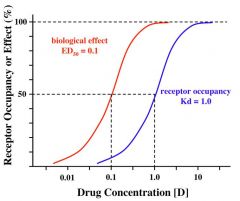
Spare receptors shift the curves to the right.
|
|
|
How does the curve for a spare receptor vary in the presence of noncompetitive antagonists?
|
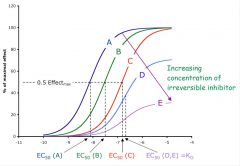
It looks like the curve for increasing concentration of inhibitory antagonist.
|
|
|
What is the law of mass action?
|
The rate of a chemical reaction is directly proportional to the product of the effective concentrations of each participating molecule.
|
|
|
How do noncompetitive antagonists affect the dose-response curve?
|
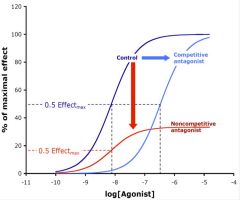
It shifts it down, because the antagonist either binds irreversibly or at a site distinct from the agonist binding site such that it decreases the ability of the agonist to bind to its site. Thus, there is effectively less receptors available for the agonist to bind.
|
|
|
How does a competitive antagonist affect the dose-response curve and why?
|
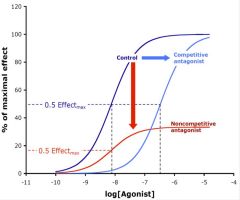
Competitive agonists shift the dose-response curve to the right, because the bind reversibly, increasing the concentration of agonist necessary to achieve the same response as before.
|
|
|
Describe the action of inverse agonists.
|
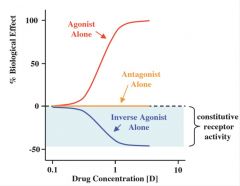
Inverse agonists reduce constitutive activity of receptors.
|
|
|
What’s the molecular nature of most drug targets?
|
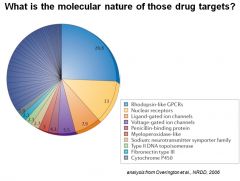
Most drugs target GPCRs
|
|
|
What type of channels are GABA channels, and what type of molecule passes through them?
|
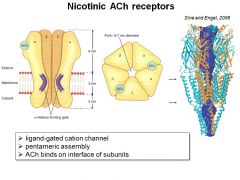
GABA channels are chloride ionotropic channels with inhibitory activity (i.e., they hyperpolarize the membrane). They also happen to be pentameric.
|
|
|
What type of stimulus is provided by glutamate receptors?
|
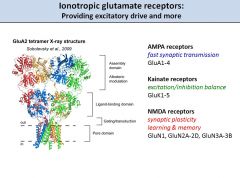
Glutamate receptors provide excitatory stimulus, unlike GABA receptors.
|
|
|
What’s the difference between the time scale of action of ionotropic versus metabotropic receptors?
|
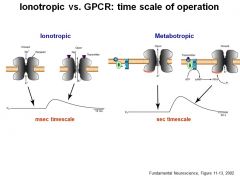
Ionotropic receptors act quickly (msec), whereas metabotropic receptors act more slowly (seconds-minutes)
|
|
|
What does tachyphylaxis mean?
|
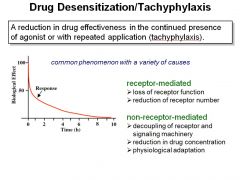
Tachyphylaxis is a reduction in drug effectiveness in the continued presence of agonist or with repeated application (tachyphylaxis).
|

