![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
What’s an important difference between the cell membranes of fungi and human cells?
|
Fungi contain ergosterol rather than cholesterol
|
|
|
What are the two forms that fungi could have?
|
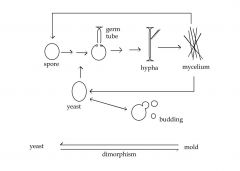
Fungi can exist as molds or yeast
|
|
|
What is the fungal major reproductive unit?
|
The fungal major reproductive unit is the spore, which is generally what’s transmitted to humans and causes infection.
|
|
|
What is the mechanism of amphotericin b?
|
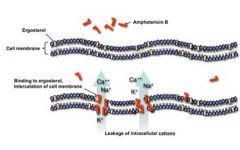
Polyenes like Amphotericin B (also nystatin) directly attacks ergosterol in the fungal cell walls, permitting loss of electrostatic potential through electrolyte leakage.
|
|
|
What is the mechanism of azoles?
|
Azoles block cell wall synthesis by blocking fungal cytochrome p450 enzymes, which interrupts sterol synthesis steps
|
|
|
What is the mechanism for Allylamines (e.g., Terbinafine)?
|
Allylamines (e.g., Terbinafine) attack an earlier step in ergosterol synthesis (squalene epoxidase)
|
|
|
What is the mechanism of action of Flucytosine (5-FC)?
|
Flucytosine (5-FC) is a pyrimidine analog that’s transported by a fungal-specific permease. It gets converted into RNA and DNA and inhibits DNA synthesis.
|
|
|
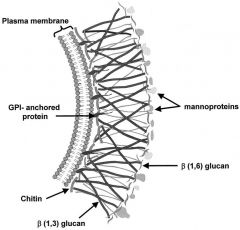
What is the mechanism of action of Echinocandins?
|
Echinocandins impair beta-1,3 glucan production, impairing cell wall stress tolerance
|
|
|
What is the mechanism of action of Griseofulvin?
|
Griseofulvin forms a complex with keratin-producing cells (hairs, nails), resulting in site-specific anti-fungal properties. It binds tubulin in fungal cells and impairs mitosis by impairing microtubule synthesis.
|
|
|
What’s an example of a superficial mycosis?
|

Superficial mycoses involve the stratum corneum and are caused by members of the Malassezia genus. Hypo and hyper-pigmented regions can develop, e.g., pityriasis versicolor.
|
|
|
What are pathogens that cause cutaneous mycoses, and how would you treat them?
|

Three major genera (Trichophyton, Microsporum, and Epidermophyton) cause superficial mycoses. Representative infections are the tinea family (capitis, pedis, cruris), misnamed “ringworm.” Treatment would consist of cleansing, dry conditions, and topical (miconazole, clortrimazole) or systemic (griseofulvin, ketoconazole, itraconazole) therapy.
|
|
|
What are examples of subcutaneous mycoses, and how would you treat them?
|

Sporotrichosis (caused by Sporothrix schenkii) is a subcutaneous mycosis. Subcutaneous mycoses are generally self-resolving, but itraconazole or amphotericin B is effective.
|
|
|
What are the major systemic (non-opportunistic) mycoses?
|
1. Coccidiodomycosis
2. Histoplasmosis 3. Blastomycosis 4. Paracoccidiodomycosis These organisms are generally found in nitrogen-rich soil fertilized by bird droppings and represent the major serious mycotic diseases. Disease is acquired by inhalation of spores and is usually asymptomatic and self-limiting. |
|
|
What are the opportunistic mycoses?
|
1. Candidiasis
2. Cryptococcosis 3. Aspergillosis 4. Mucormycosis 5. Pneumocystosis These have only marginal pathogenicity and generally co-exist with the host, and generally progress during conditions of host immunosuppression or alterations in the bacterial niche (i.e., someone uses antibiotics. |
|
|
What is the most common of the systemic fungal pathogens?
|
Candidiasis is the most common of the systemic fungal pathogens.
|
|
|
Coccidiomycosis
|
Endemic in the south US and latin America. Generally asymptomatic. 40% develop influenza-like symptoms, and 15% develop hypersensitivity reactions with rash and adenopathy. Treatment: itraconazole or amphotericin.
|
|
|
Histoplasmosis
|
Endemic to central and eastern US, notably Ohio and Mississippi River valleys. Generally self-limiting. High doses can result in acute pulmonary disease. Virulence factors include cell wall alpha 1,3-glucan. Treatment: itraconazole or amphotericin B
|
|
|
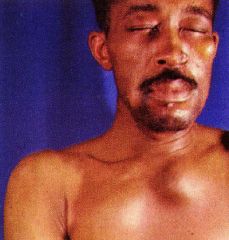
Blastomycosis
|

Endemic in North American and Canada, also present in Africa, South America and Asia. Pulmonary focus may result in a non-specific lower airway infection. Dissemination often to the skin, resulting in ulcerated granulomatous lesions. May spread to CNS, gonadal tissue/testis and bone. Treatment: itraconazole or amphotericin B
|
|
|
Paracoccidiodomycosis
|

Pulmonary infection, strongly male predominant, restricted to South America. Long dormance (decades), then reactivation with advanced pulmonary disease and/or dissemination. Treatment: itraconazole, ketoconazole+trimethroprim-sulfa, and amphotericin B
|
|
|
Candidiasis
|

The most common of the systemic mycoses, caused by Candida albicans, parapsilosis, and tropicalis. Colonize mucosal surfaces of all humans at birth and following trauma or unchecked proliferation (i.e. antibiotics) may cause disease. Clinical, superficial (mucosal and cutaneous): thrush and vulvovaginitis, chronic mucocutaneous resulting from childhood immunodeficiency and systemic (disseminated) as the result of barrier penetration in an immunocompromised individual. Systemic spread may result in infections of the heart, kidneys, eyes, and CNS. Treatment: local (thrush-nystatin), systemic (ketoconazole, fluconazole, amphotericin B, or capsofungin).
|
|
|
Cryptococcosis
|

Found in pigeon feces worldwide. Initial pulmonary infection may spread to CNS. Often asymptomatic or with an influenza-like illness during primary infection. Meningoencephalitis may be chronic. Treatment: amphotericin B +/- flucytosine and fluconazole prophylaxis to follow.
|
|
|
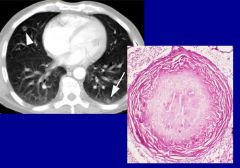
Aspergillosis
|

Common naturally occurring fungus. Hypersensitivity reactions common, pulmonary invasion followed by invasive hyphae. Invasion of vessels results in localized thrombosis and subsequent tissue infarction. Tendency to invade bronchial airspaces leads to allergic bronchopulmonary aspergillosis, notably for recurrent asthma, CXR infiltrates, peripheral eosinophilia. Treatment is often with steroids for allergic controls. Treatment with local ocontrol (excision of aspergilloma) and itraconazole and/or amphotericin B. Invasive infetions require amphotericin B, voriconazole, or posaconazole.
|
|
|
Mucormycosis
|

Highly invasive local tissue infections, starting in the nose, spreading through the face, with potential direct extension to the CNS, causing thrombosis and infarction. Increased risk from diabetes mellitus, leukemia, lymphoma, corticosteroid treatment, severe burns, immunodeficiency, and dialysis with iron chelating using deferoxamine. Requires surgical management, recurrent debridement, and amphotericin B therapy.
|
|
|
Pneumocystosis
|
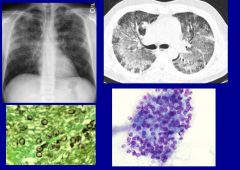
Caused by Pneumocystis carinii resides in the pulmonary tree, causing infection to the immunocompromised, notably premature or malnourished infants and in HIV/AIDS. Treatment with trimethoprim-sulfamethoxazole or pentamidine isethionate. Prophylaxis can be achieved with intermittent TMP-SMZ or monthly aerosolized pentamidine.
|
|
|
What are some virulence factors for fungi?
|
• Alpha(1,2) glucans
o Help resist macrophage phagocytosis, antigen masking, conceals β-glucans from becoming immuno-stimulatory • Adhesion to epithelia and ECM o Frequently observed in C. albicans, P. brasiliensis, B. dermatitidis, H. capsulatum, and C. neoformans. For example, P. brasiliensis produces gp43, which promotes laminin adherence • Hydrolytic Exoenzymes o Proteases, lipases, phospholipaseses o May damage barriers and host cells Liberate nutrients Destruction of immunoglobulins Penetration through mucous membranes o C. immitis produces collagenase and elastase. Pathogenic Cryptococcus produces DNase and various proteases • Aflatoxin o Highly carcinogenic o Liver injury/failure o DNA injury • Ureases and ammonia o Contribute to pulmonary tissue injury |
|
|
Which two fungal conditions could be lethal due to CNS injury (e.g., meningitis)?
|
Cryptococcosis and Mucormycosis
|

