![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
286 Cards in this Set
- Front
- Back
|
Canadian C-Spine Rule Exclusion Criteria |
Non-trauma GCS < 15 Unstable vital signs Age < 16 Acute paralysis |
|
|
Canadian C-Spine Rules High Risk Factors |
Age > 65 Dangerous mechanism (fall from > 3 feet; Axial load; MVA > 100km) Paraethesia in extremities
IF YES TO ANY OF ABOVE - RADIOGRAPHY
|
|
|
Canadian C-Spine Rules Low Risk Factors |
Simple rear-ended MVA Sitting in ED Ambulatory at any time Delayed onset of neck pain Absence of midline tenderness
IF YES, & CAN ACTIVELY ROTATE NECK 45 deg LEFT & RIGHT - NO RADIOGRAPHY |
|
|
Causes of Damping |
Damping = The gradual reduction of excessive oscillation, vibration, or signal intensity, and therefore of instability in a mechanical or electrical device
Causes: - Air bubbles - Clotting - Kinking - Real BP |
|
|
Contraindications Nasal Intubation |
Absolute: Base of skull # Significant bleeding diathesis
Relative: Anti-platelet Reversed anti-coagulated Valvular or CHD Hereditary telangiectasia |
|
|
AFOI Innervation |
CNV: V2 (Greater & lesser palantine) - nasal turbinate & septum V1 (Ethmoid) - Rest of nasal passage Although there is variability CNIX: Posterior 2/3 tongue; pharyngeal epiglottis; soft palate; oropharynx SUPERIOR LARYNGEAL (CNX) Base of tongue; Posterior surface of epiglottis; arytenoids & aryepiglottic fold RLN (CNX) VC & trachea |
|
|
Anticonvulsant Meds Implications |
Enzyme induction: Phenytoin Carbemazepine Barb Will increase metabolim of vec & roc - so use cis or atracurium
Decreased Seizure Threshold: - Ketamine - Enflurane - abnormal EEG - esp w hyperventilation |
|
|
Epilepsy suitability for day surgery |
Well controlled: Seizure free >1 yr Nocturnal seizures only |
|
|
Anaphylactic vs Anaphylactoid |
End point for both - mast cell degranulation Anaphylactic - Type 1 IgE mediated Anaphylactoid - Dose related
|
|
|
Anaphylactic Testing |
TRYPTASE: - In vivo half life 3hrs (histamine 3min); Peak 1hr - 3 samples - 1hr; 4hrs & > 24hrs REFER for TESTING: - Skin testing - IgE - RAST (radio-allergosorbent test) - measuring specific IgE - CAP - fluoro-immunoassay - alternative to RAST - more sensitive than RAST |
|
|
Causes of Life-Threatening Reactions |
NMBDs (70%) Latex (12%) Colloids (5%) Induction agents (4%) Antibiotics (3%) BDZ (2%) Opioids (2%) Other (2.5%) e.g. Radiocontrast media |
|
|
Neuropathic Pain Def |
pain initiated or caused by a primary lesion or dysfunction of the nervous system |
|
|
Allodynia |
Painful response to a normally innocuous stimuli |
|
|
Hyperalgesia |
Increased response to painful stimulus |
|
|
Dysasthesias |
Abnormal sensation |
|
|
Warming Modalities |
Forced air warming Insulating layer Warming OR Circulating water mattress IV fluid warming Humidification of gases Preop warming Radiant heaters |
|
|
Hazards of Prone Position |
AIRWAY CVS - increased afterload; decreased preload; compression of neck veins ETT tie; increased myocardial demand (afterload) NEUROLOGICAL - C spine; Spinal cord (vertebrobasilar); Neuropathies (BP; Peroneal; Ulnar; Sciatic stretch; Fem compression); CVA risk OCULAR - Corneal abrasian; Orbital compression; Venous drainage RESP - Decreased FRC; Abdo compression; Atelectasis M-SK - C spine; Pressure ulcers; Gonads/breast; Face; Lines/monitoring THROMBOEMB MANUAL HANDLING LINES
|
|
|
CI to Beach Chair |
1. Risk of cerebral hypoperfusion: - Severe carotid disease/Increased ICP/ Chronic HTN - Hypovolemia - Autonomic dysfunction 2. Spinal injury 3. Morbidly obese (relative/precaution) |
|
|
Hypothermia - Def & Effects |
Temp < 35 deg
EFFECTs: Shivering - Increased pain; Dystonias; Dicomfort; Inc pain Inc Infections - Resp/surgical wound healing Drugs - Impaired metab & elimin (anaesthetic agents; analgesia; NMBDs) Increased hosp stay & cost CVS - Arrythmias/ Inc HR; Inc SCR/BP; Peripheral perf; IV access; ECG artefact; SpO2 CNS - Delayed wake; Opioid sens; Inc ICP Resp - Central resp depression; L shift ODC (dec unloading) GIT - ischaemia; Imp gut motility Renal - cold diuresis HAem - Imp Plt/clotting factor; Thromboemb risk/stasis (NB Coag tested at 37 deg therefore normal) Endocrine - Stress response - catechol/ Na & H2O retention; Inc BGL |
|
|
Monitoring ANZCA |
Clinical - Circulation/Ventilation/Oxygenation
Equipment - Must be in use: - O2 Analyser - Breathing system disconnection or vent failure alarm - Pulse oximeter - tone & alarm - CO2 monitor - VA analysis
Must be available: - ECG - 5 lead option - BP - NIBP (must be) & invasive (should be) available - Temp - NMS - BIS/Entropy - Other indicated monitors e.g. TOE; CO; CVP; EEG
|
|
|
Risk of MACE in Stents for non-cardiac surgery |
MACE = Death; MI; Thrombosis or rpt revascularisation
BMS <30 days - 11% DES < 90 days 6.4%; < 365 days 5.9% |
|
|
RFs for Thrombosis of Stents |
CLINICAL: - Previous stent thrombosis - Age >80 - Prior brachytherapy - Low EF - ACS indication for stent - Renal failure - DM STENT/PROCEDURAL RELATED: - Left main - Long stents (>18mm) - Small vessels (<3mm) - Suboptimal angio results - Multiple stents/overlapping - Ostial or bifurcation lesions |
|
|
Bridging for Non-cardiac Surgery (stents) |
Consider if high risk for thrombosis: BMS - < 6/52 or > 6/52 w addit RFs DES - <1 yr or >1yr w addit RFs
High risk surgery - Intracranial/Spinal/Extraocular/TURP
Option for high risk thrombosis & surgery: Cont aspirin if possible Cease clopidogrel 5 days before Tirofiban & UFH 3 days pre-op - cease 8hrs D1 post-op - give 300mg clopidogrel Other - short acting ADP-RA e.g. Ticagrelor - in future
NB Should be done in centre w CCU & PCI capability
|
|
|
Awareness Causes & Risk |
Human factors - miscalculation; omission; programming; inattention Patient factors - Inability to tolerate adequate anaesthesia; Altered PD or PK (obesity; hypermetabolic; other drugs); DI Equipment factors - delivery or monitoring - calibration; malfunction; disconnection
Risk 0.1-0.2% Implicit (unconscious awareness) & Explicit |
|
|
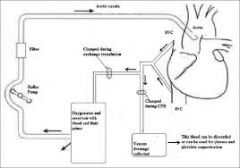
Pre-requisites for coming off CPB |
TRAVEL-CC
Temp - Normothermia (36-37deg) Rate/Rhythm - High-normal (80-90) & SR Acid/Base - Normal pH/pCO2/ HCO3 Ventilation - 100% O2 & expand lung bases Electrolytes - K (4.5-5); Mg; Ca Level table CO - Establish native cardiac output Coag - have protamine ready & do TEG
Main concerns - Inotropy; Coag; Temp |
|
|
Causes AS & natural Hx |
Calcific AS - age 70-90; progresses slowly Calcific Biscuspid (1-2% population); M>F; 40-60yrs RHD & congenital - rare
Pathophys - Sclerosis initally - ~16% progress to AS w/i 7yrs - Eventually LVH leading to diastolic dysfunction w onset of congestive symptoms OR angina (demand > supply) |
|
|
ECHO AS Features |
Qualitative: - Valve leaflets - AR - Post-stenotic root dilation - RWMA - TR/RV function
Quant: - EF - AVA - Pressures - gradients; RVSP - Velocity - Diastolic dysfunction |
|
|
Mortality AS |
Asymptomatic <1% / yr 50% mortality if symptomatic, or median survival: Angina 5 yrs Syncope 3 yrs Dyspnoea 1 yrs
Not linear, therefore exercise used to reveal occult symptoms in younger pts at low surgical risk |
|
|
AS Anaesthetic considerations |
Maintain SR Avoid brady or tachycardia Maintain SVR/avoid hypotension Optimise IV fluid volume to maintain VR & LV filling |
|
|
Day Surgery Criteria for DC |
Stable vital signs >1hr Correct orientation as appropriate No resp distress/stridor - 4hrs post extubation Pain controlled - with suitable analgesia for DC Minimal N&V, dizziness Adequate hydration & oral intake Minimal bleeding or wound drainage Responsible adult to take home Lines of contact established |
|
|
Day Surgery Suitability |
PROCEDURE SUITABILITY - Airway; Length; Inexperience; Post-op surgical or anaes complications (airway or bleeding); NOT cranial/Tx/Abdo; Pain; Return to diet
PT SUITABILITY - PGA >46weeks; Ability to follow instructions; Place of residence w/i 1hr; ASA 1/2 or medically stable 3/4
SOCIAL REQUIREMENT - Responsible adult to take home; Within 1hr of appropriate medical help; Access to telephone
|
|
|
WHO SS Checklist Objective |
Improved communication & culture of safety
- Correct site surgery - Provision of safe anaesthesia - Management of airway problems - Management of haemorrhage - Avoiding known allergies - Minimising risk of surgical site infection - Preventing retention of swabs - Accurate ID of specimens - Effective COMMUNICATION w/i surgical team - Routine surveillance of surgical outcomes |
|
|
WHO SS checklist Evidence |
Reduced overall mortality 1.5% to 0.8% Complication rate 11 to 7%
|
|
|
WHO Components |
SIGN IN (B4 induction) Pt; Site; Surgery; Consent; Marked; Anaes machine & meds; Allergy; Anaphy; SpO2
TIME OUT (B4 skin incision) Team intro; Pt; Site; Surgery; Incision; Abs; Anticipated critical events; Imaging
SIGN OUT (B4 pt leaves OT) Counts; Specimens; Equipment probs; Name of procedure |
|
|
Consent Steps |
ELEMENTS 1. Must be voluntary 2. Must be competent 3. Provision of information - info sheets not enough alone 4. Documentation 5. Qualified personell & interpreter if needed
WHY NECESSARY - Ethicial (Autonomy) & Medicolegal
|
|
|
Serotonin Syndrome Causative Drugs |
Anti-depressants - SSRIs; SNRIs; TCAs; *MAOIs Opioid & related - Tramadol; Peth; Fent Mood stabilisers - Lithium; Na Valproate Recreational - Ampheth; Ecstasy Herbal - St Johns Wort; Ginseng Anti-emetics - Ondansetron; Metoclopr ABs - Linezolid
|
|
|
Serotonin Syndrome - Clinical |
CAN: CNS - Confusion/Agitation; Seizures - Coma ANS - Labile BP & HR; Hyperthermia; Dysrhythmias; Mydriasis; Flushing Neuromuscular (NM) - Rigidity; Hyper-reflexia; Clonus
DIAGNOSIS - of exclusion; Need NM signs & exposure to drug w/i 5 wks Extensive DDx - Drugs; Encephalopathies; Psych; MH; TFT |
|
|
NMS vs Serotonin Syndrome |
NMS - Idiosyncratic reaction after prolonged exposure OR abrupt cessation NMS - Develops over days or wks NMS - Severe muscle rigidity & rhabdo (SS - mydriasis, diarrhoea, hyper-refl, myoclonus) NMS - Freq assoc w MOF |
|
|
Contraindications Sitting Position (Neuro) |
ABSOLUTE: - Patent AV shunt - PFO - RAP > LAP - Cerebral ischaemia when upright & awake RELATIVE: - Extremes of age - Uncontrolled HTN - COPD |
|
|
SITTING POSITION COMPLICATIONS |
VAE Pneumocephalus Macroglossia Quadriplegia PNS - particularly common peroneal; RLN (inc risk w TOE) Spinal injury/SC |
|
|
Ethical Principles |
Autonomy Beneficence Non-maleficence Fidelity - faithfulness to our duties Justice Utility - greater good Paternalism |
|
|
Block of Fibres with RA - Order |
1. Sympathetic 2. C - Cold (slow pain, T, touch) 3. A delta - Pinprick (fast pain & T) 4. A beta - Touch; Pressure 5. Motor
Usually highest to lowest: Cold - Pinprick - Touch |
|
|
Obstetric Blockade - Required levels & organs |
Incision - T12/L1 Peritoneum - T4 Uterus T10 |
|
|
Laryngeal Trauma Signs |
(HaNDSSS) MAJOR: Stridor Inability to lie Supine Subcut emphysema MINOR: Hoarseness Haemoptysis Dysphagia Neck tenderness/swelling
|
|
|
Sizes ETT to fit BB & FOB |
ETT >4.5; EBB 5; FOB <2.8 ETT >6.5; EBB 7; FOB <3.5 |
|
|
Sizes EBB |
French 5 7 9
|
|
|
DLT Sizes |
French (1 Fr = 1/3mm; 3 Fr = 1mm) 28/32/35/37/39/41 Calculating: - Diameter of trachea at clavicles - Ht of pt - Distance at lips NB Size 35F & below - need ped bronch <2.8mm >35F - fits 4.2mm FOB? |
|
|
Cerebral Monitoring |
Intraventricular Drain/Catheter Intraparenchyal Subdural pressure transducers Jugular bulb oximetry - shows effects of interventional therapy; Invasive; global O2 utilisation only Transcranial doppler - differentiate bn vasospasm & hyperaemia Near Infrared Cerebral Spectroscopy
NB ICP Monitoring - only evidence in TBI
|
|
|
DDx Stridor |
FB Infectious: - Epiglottitis - Croup (most common acute) - Bacterial tracheitis - Retropharyngeal or tonsillar abscess Laryngomalacia (most common chronic) Severe bronchospasm VC dysfunction Burns External compression |
|
|
ARDs Def & Diagnostic Criteria |
Def = Syndrome of inc pulm cap permeability & inflammation
Diag Criteria: PaO2 / FiO2 < 200 Bilat infiltrates on CXR PCWP < 18mmHg or no evidence of inc LAP |
|
|
ARDs Management |
1. Adequate Oxygenation (paO2 ~60) 2. Minimise Ventilator Trauma: - Volutrauma - Barotrauma - Biotrauma (infl) - Atelectotrauma PROTECTIVE LUNG STRATEGIES - TV 4-8ml/kg; Plateau P <30; High PEEP (5-24) 3. Prone - severe ARDS NNT = 11 4. Permissive Hypercarbia (deep sedation) 5. NO/PGI2 (no survival benefit); ECMO |
|
|
PCA Service |
Patient Selection Equipment Factors - Pump & lines Staff Factors Review
|
|
|
Contents Epidural Space |
Dural sac Fat Spinal nerves Connective tissue Blood vessels |
|
|
Tx vs Lx Epidural |
Tx VS Lx Distance from posterior epidural border to dural sac: Tx 1.5-3mm Lx ~6mm Ligament flav - thinner & softer Cardioaccel fibres T4 |
|
|
Decontamination |
Removal of micro-organisms from contaminated materials or living tissue |
|
|
Disinfection |
Inactivation of non-sporing organisms by thermal or chemical means Requires previous thorough decontamination eg 100deg water for 10min 70% EtOH 10min Doesn't kill a few bacterial spores |
|
|
Sterilisation |
Removes or destroys all forms of microbial life Must be decontaminated first Steam under pressure (autoclave) - most reliable |
|
|
Contraindications to Exercise Stress Test |
ABSOLUTE (pretty much acute cardiac conditions) Acute MI Unstable angina Uncontrolled arrhythmia Severe AS Uncontrolled HTN Severe pulm HTN Aortic dissection Acutely unwell Heart failure |
|
|
Types of Stents DES |
Paclitaxel - anti-proliferative Sirolimus - anti-metabolite |
|
|
PDPH Incidence & untreated % |
Touhy needle puncture - 70% PDPH Untreated - 72% resolve within 7 days - 85% within 6 wks
|
|
|
PDPH Clinical Features |
Typically within 24-48hrs (up to 7days) Bifronto-occipital Neck stiffness Worse on standing Assoc - Diplopia (14%); Tinnitus (10%)
|
|
|
PDPH Treatment |
Intrathecal Catheter: - PDPH 6% (Late removal) (Resite - 90%; 50% late removal) Simple analgesia & rest - may help PHARM: - Steroids - dec intensity - Caffeine - poor evidence - Sumatriptan - nil evidence - Epidural saline - typically transient Blood patch (separate slide) |
|
|
Blood patch - Evidence; Efficacy; Technique & CIs |
EVIDENCE: - Symptomatic HA not relieved >24hrs post puncture (71% failure vs 4% if done >24hr) EFFICACY: - 75% pts - complete relief; 18% incomplete; 7% none TECHNIQUE - 15-25ml; Stop when pn; Lie still 2hrs post; no lifting 1/52 CI: - Normal epid CIs; ?Oncology COMPLICATIONS - Transient back pn (35%); Radicular pn; CN palsy; Meningitis; Seizure
|
|
|
PDPH DDx |
PIH/PET Meningitis Cerebral SOL Cerebral vein thrombosis - usually unilateral motor & sensory loss LLs Migraine ICH/SDH/SAH Muscle tension Caffeine withdrawal |
|
|
Causes of Visual Loss |
Rare - all surgery 0.0008%
CORNEAL ABRASIAN VASCULAR COMPROMISE/INAD O2 - Ischaemic optic neuropathy (most common) - Central Retinal Artery Occlusion (mostly embolic; Ext pressure) or BRAO - Central Retinal Vein Occ (External pressure) - Cortical Blindness (MCA/PCA occip/ICA chiasm)
OTHERS - Acute glaucoma |
|
|
Ischaemic Optic Neuropathy - Types, & prognosis |
Most common cause visual loss peri-op Causes not clearly determined ANTERIOR - to sclera foramen - Non-arteritic & arteritic; Vasculitis POSTERIOR - more often embolic than occlusion AION & POIN - different blood supplies & diff RFs Complete or partial loss Poor prognosis - 50% no improvement
|
|
|
Risks of Intra-op Visual Loss |
PATIENT: - Elderly - Vasc disease - Cardiac RFs SURGERY/ANAES: - Spinal/prone/cardiac - Prolonged - Large blood loss - Fluid administration
|
|
|
Reducing risk of Visual Loss |
PRE-OP - Identifying those at risk INTRA-OP - Maintain IOPerfusion/O2 - Avoid hypotension - Dec transfusion threshold - Minimise IOP - Max venous outflow - Avoid direct pressure - DVT prophy - TEDs; SCDs POST-OP - Screen - As above + clexane |
|
|
Risk Resp Events Paed |
PT - Hx Airway reactivity; Recent URTI (4-6/52); Symptoms (cough/fever/recurrent); Age<1; Premature; Parental smoking; Un-fasted; GORD SURG - ENT; Pneumoperiton; Emerg ANAES - ETT (x10); LMA (x5); Light anaes |
|
|
Buprenorphine Patch PD & PK |
Mixed ag (mu) /antag (kappa) Ceiling effect for resp dep; not analgesia T max 60hrs High PPB High lipid solubility T1/2 5 days Metab - liver to bile (norbupren low activity) |
|
|
Regional General Answer |
CIMPLE-TED CONSENT - Include CIs & risks IV ACCESS MONITORING - O2/NIPB/ECG POSITION LA - dose & type EQUIPMENT - Needle (usually short bevel stimuplex); PNS; USS (linear probe 10-15MHz for most) TECHNIQUE - includes landmarks; anatomy; end point EVALUATION - time DOCUMENTATION |
|
|
Blocks to use Curved USS Probe |
Sciatic sub-gluteal block (3-7MHz) - probe in line with greater trochanter & ischial tuberosity Lumbar plexus block |
|
|
VTE RFs |
SLOMMM-COM-Throm SLOMM (major - RR 5-20): S - Surgery/trauma L - LL probs O - Obstetrics M - Malignancy; Mobility; Misc (previous)
COM (minor - RR 2-4) C - CVS (CHF/CHF) O - OCP/HRT M - Misc - travel/COPD/Neuro disab
Thrombophilias
|
|
|
VTE Prophylaxis (* = quality of evidence) |
GENERAL: **Mobilise; Hydration; High quality surgery MECHANICAL: (not demonstrated to dec death or PE) *TEDs (best w heparin); *SCUDs (method of choice - only if BMI <28) Need to be well sized/fitted; Can be worn intra-op NEURAXIAL - low quality data PHARM: **UFH - Inc risk minor bleeding & HITTS cf LMWH **LMWH - Better than UFH for high risk NEWER - Fondaparinux (synthetic) - same as LMWH - Rivaroxaban (Direct Thr I) - Possibly better but inc bleeding risk |
|
|
PONV Risk Score |
RFs - Female; Non-smoker; Previous PONV; Opioids in PACU Risk: 0 RF - 10% 1 RF - 20% 2 RF - 40% 3 RF - 60% 4 RF - 80% |
|
|
Disproven PONV risks |
BMI Anxiety Migraine NG tube Peri-op fasting
UNCERTAIN: - Neostigmine - ASA - Menstrual cycle |
|
|
Strategies reduce PONV w Evidence |
Level A: - RA - TIVA - induction & main - Avoidance N2O - Avoid post-op opioids (multimodal) - Hydration |
|
|
PONV treatment NNT |
5HT3 = 5 Drop = 5 (prevention) Dex = 4 (prevention & nausea); 7 (vomit) Anti-chol = 6 Propofol = 5 (temp) Midaz - 2mg 30 b4 end better than premed (as effective as ondans)
|
|
|
PONV Risk Children |
RFs: Surgery > 30min Age > 3yrs Strabismus Hx PONV or PONV in relatives
Risk: 1 RF = 10% 2 = 30% 3 = 50% 4 = 70%
|
|
|
Obstetric Palsies |
~1% Incidence SPINAL - Rare; Traumatic; Chemical; Ischaemic; Infective LUMBOSACRAL TRUNK - w/i pelvis by foetal head - Foot drop (unilat 75%); 76% recover completely PERIPHERAL: LFCN - most common; Self-limiting; RFs - DM; Hip F/Abd/ER; Obesity FN - Compression ing lig; RFs - Hip F/ER/Abd ON - 25% B/L; Usually w FN; Compress fetal head - pelvis or forceps CP - Disting from LS injury w nerve conduction; Knee hyperflex |
|
|
Differentiation Obstetric Palsy vs Central Lesion |
CENTRAL - Commonly assoc w back or leg PAIN - Bilateral (unusual for periph but possible) - Deteriorating S&S or onset after symptom-free interval - Fever & WCC suggests infection
|
|
|
Red Flags Post Neuraxial |
Acute onset back pain Radicular leg pain Urinary & anal dysfunction LL numbness & weakness
Permanent injury b/n 6-12hrs post symptom onset |
|
|
VAE Detection Sn |
Most to least Sn: TOE Praecordial Doppler PAP - start to get minor clinical signs (HR; BP) EtCO2 Echo - Signif clinical signs (CVS collapse) Oesophageal stethoscope ("Millwheel")
|
|
|
Prevention VAE in Sitting |
1. Positive Venous Pressure - Positioning - Normovolemia - Venodilation - PEEP (controversial) - Jug vein compression (times of high risk) 2. SURGICAL TECHNIQUE - Bone wax; Saline gauzes - Communication high risk periods - Fastidious haemostasis - Dec time 3. EARLY RECOGNITION - Bubbling at site - EtCO2 |
|
|
Signs VAE |
CLINICAL: - Desat - Sudden drop EtCO2 - HR - inc or arrhythmia - Inc ETN2 - Inc CVP/neck vein distension Remember can also be from IV lines |
|
|
Anatomy Larynx (C spine levels) |
Hyoid C3 Superior horn of thryoid cartilage C4 Cricoid C6 |
|
|
C450 Inducers & Inhibitors |
INHIBITORS SSRIs/St Johns Wort* Buprenorphine* Cimetidine/Ranitidine* Metoclopramide*
INDUCERS Dexamethasone * Rifampicin* Anticonvulsants
* = 2D6 |
|
|
Autonomic Neuropathy Incidence, CVS S&S |
Incidence 1 in 10 DM (all types) (40% DM1)
- Resting tachy (90-130) - Exercise intolerance - Loss of HR variability (normal >15 w deep breathing - AN likely when <10; Abn Valsalva) - Orthostatic hypotension (SBP >30; DBP >10) - Silent MI - QT abnormalities 2 Abnormal tests for Dx (most Sn - HR response to standing/valsalva/deep breathing) - Assoc w greater haem changes intra-op
|
|
|
Autonomic Neuropathy S&S GIT & Other |
- Gastroparesis (GORD; Early satiety; Nausea) - Constipation, alternating w diarrhoea (often nocturnal)
OTHER - Absence of sweating/perfuse gustatory sweating; Dec recognition of hypo; Urinary retention; Poor temp regulation; Impotence |
|
|
Effects of Hypothermia |
CVS - Vasoconstrict/SNS; <28 arrhythmias; AMI RESP - L shift ODC CNS - Confusion <34; LOC <32; Slow wake; Dec O2 5%/degree NM - Shivering - O2 demand & monitoring artefact; Dec metab NMBDs IMMUN - Impaired wound healing; Neutr HAEM - Plt & factor dysfunction BEHAVIOURAL
|
|
|
SC Blood Supply |
ASA - Anterior 2/3 of cord - Arises foramen M junction of vert @ 2 x PSA - From PICA Anastamoses b/n ASA & PSA.
Reinforced by radicular @, branches from: * ascending cervical artery* deep cervical artery * intercostal arteries * lumbar arteries * sacral arteries * |
|
|
SC RFs ischaemia & Prevention |
SCPP = MAP - CSFP Autoreg 45-180 Time >30-45min RFs - Distal aortic hypoperfusion - Peri-op hypotension - Hypoxemia PREVENTION 1. MAP/O2/Time 2. CSF drain - best w option 3 (set overflow 10 & cont post-op) 3. Distal aortic perfusion - only works if @ Adam below clamp 4. Surgical implantation critical intercostal @ 5. Hypothermia - local (epidural) or systemic |
|
|
Reasons not to do AFOI/Possible Probs/CIs |
|
|
|
Paediatric Dehydration Estimation (RCH) |
MODERATE DEHYDRATION (4-6%) - Delayed Central CRT (>2sec) - Inc RR - Mild Dec turgor SEVERE (>7%) - CRT >3sec; Mottled skin - Other signs of shock - Inc HR; irritable or Dec LOC - Deep, acidotic breathing - Dec turgor
UO (Mild/mod/sev) <2/<1/<0.5 |
|
|
Indications OLV |
ABSOLUTE: 2. Control of ventilation - BP fistula - Giant cyst or bullae - Major bronchial disruption or trauma - Unilat Tx 3. Surgical Access - VAT
RELATIVE: - Surgical access - Lobectomy/pneum - Other thoracic surgery - Oesoph; Vertebral |
|
|
Relative CIs OLV |
Paediatric - won't tolerate Tumour in lower trachea Critically O2 dependent |
|
|
Differential Blood flow - normal lung & OLV |
NORMAL: (R) 55% (L) 45%
OLV: Non-dependent 77.5% Dependent 22.5% |
|
|
Hypoxia on OLV Steps |
1. Check oximetry/trace/scan monitors 2. Increase FiO2 3. Check circuit/ventilator 4. Auscultate 5. Suction dependent lung & tube patency 6. Check tube position 7. Apply CPAP or entrain O2 to NVL 8. Perform recruitment man. or PEEP 9. Revert 2 lung 10. Clamp PA to NVL
(OO Circuit Listen Scan Suction Tube CPAP PEEP 2lung Clamp) |
|
|
General Approach to Any Complication |
ABC - Immediate medical care RV notes/event Sorry - open communication Debrief Consults Documentation Medical indemnity & hospital medico-legal authority Audit M&M
|
|
|
P COPE PRIME TIME RAW |
P - Pt; Procedure; PMHx C - Consults (inc Hx/Ex/Ix) O - Optimisation P - Premed E - Explain & consent P - Position; Prep; Plan; Pt safety R - Resusc I - IV access & fluids M - Monitoring E - Equipment T - TF (MADE) I - Induction - plan, drugs, airway M - Maintenance E - Emergence
PACU R - Recovery handover A - Analgesia W - Ward
|
|
|
CEA: 1. Indications? 2. Peri-op Mortality & Stroke risk? |
INDICATIONS: - Symptomatic pts with moderate to severe stenosis - Definite benefit in high grade (70-99% st) - NNT = 6 - Less marked benefit in sten 50-69% - Recommendation - with 2/52 of symptoms; <48hr is best (NICE guidelines)
PERI-OP MORT & STROKE RISK 2-5% Peri-op MI 2% (IHD common) |
|
|
Perceived Advantages of LA for CEA |
- Gold standard cerebral Fx - Lower shunt insertion - Improved haemodynamic stability - Earlier detection & Rx of complications - Intact cerebral autoregulation - Lower re-exploration rate - Less post-op anxiety for surgeon & anaes - Less post-op pain - Useful for pts whom GA is undesirable (a/w CABG) - Shorter stay
DISAD: - Conversion rate 1-3% - Airway & ventilation control - VA - cerebral protection - Claustrophobia - Phrenic nerve |
|
|
GALA Trial |
GA vs LA for CEA: - No difference (non-significant trend towards fewer operative deaths) - LA assoc with less shunts |
|
|
Monitoring Cerebral Function during CEA |
ICA stump pressure (want mean >50-60) EEG - cortical only not deep SSEP - Can detect subcortical ischaemia Transcranial Doppler - MCA flow - can detect emboli Jugular VO2 Near infrared spectroscopy |
|
|
Tourniquet Complications |
LOCAL EFFECTS: MUSCLE - Inflation - anaerobic metab (necrosis >2hr) - Deflation - 'Post-tourn syndrome' - swollen, pale, stiff limb - 1-6/52 NERVE 1. Physiological block - ischaemia 2. Direct compression - large nerves more susceptible - up to 6/12 CVS - Plaque rupture w exanguination - Inc CVP & SVR (CCF) - 400ml/leg - Deflation - hypotension TOURNIQUET PN - Unmyelinated slow C fibres |
|
|
Tourniquet Times, Size & Pressure |
PRESSURE (mmHg): - Fixed - 250 for UL & 300 LL - OR SBP + 100 (UL) & 150 (LL) SIZE: - >40% diameter of thigh TIMES: 1.5-2hr (muscle ATP depleted) Temp deflation - at least 10 min (ATP restored) |
|
|
CI Tourniquet |
DVT Severe crush injury Severe OP Sickle cell disease PVD Coagulopathy Cellulitis |
|
|
Obesity Systems Effects |
RESP - Dec FRC - Possible DI (correlates with OSA & neck circ) - Pulm HTN - Obesity hypoventilation syndrome CVS - HTN - systemic & pulm - Inc risk arrhythmias due to hypertrophy; hypoxemia; inc catechol & fatty conductive - DVT risk ASSOC DISEASES: - GORD - DM OTHER - PK; IV access & monitoring |
|
|
What is Obesity Hypoventilation syndrome? |
Diurnal variation in ventilation & inc PaCO2 CO2 sens & resp drive - partly under control of leptin (satiety hormone) Relative leptin insens in obesity - Dec vent response to inc PaCO2 THEREFORE - Avoid premeds w resp depressants; Opioid sparing techniques |
|
|
What is Metabolic Syndrome |
Cluster of RFs comprising: - Excess abdominal weight - Lipid abnormalities - HTN - Elevated glucose levels |
|
|
Anaemia Effects |
CVS: - Dec viscosity -> dec resistance -> Inc preload & dec -> Inc CO - Inc HR & /or contractility - minor role - Inc O2 ER - Redistribution of blood flow to areas of high demand (myocardium & brain) - Inc 2,3-DPG -> (R) shift ODC (chronic) RESP - Tachypnoea to Inc O2 - Dyspnoea ENDO - Inc EPO IMMUN - Impaired wound healing
|
|
|
Anaemia Classificaition |
NORMOCYTIC (MCV 80-100) - Anaemia of chronic disease (absent reticulocytes; low transferrin, iron & %sat) - Haemolysis (reticulocytes; high LDH; mildly inc bilirubin)
MICROCYTIC (MCV <80) - Iron def (hypochromic; high transferrin) - Chronic disease - Thalassemia
MACROCYTIC (MCV >100) - Acute blood loss - Haemolysis - Megaloblastic - Drugs (alcohol; MTXl Azathioprine; phenytoin)
|
|
|
SAH - WFNS Grades
|
GCS & Motor Deficit (+/-) Grades I - V I - 15 (-) II - 13-14 (-) III - 13-14 (+) IV - 7-12 (+/-) V - 3-6 (+/-) So basically only care about motor deficit to differentiate b/n grades II & III |
|
|
SAH - HUNT & HESS Grades |
Based on clinical presentation - more detail than WFNS (i.e asymptomatic; HA; nuchal rigidity; CN palsy; Drowsy; Hemiparesis; rigidity & coma)
Gives mortality: Ranges from 0-2%; 5-10% (Grades II & III) to 50% (V) |
|
|
Complications SAH |
1. RE-BLEED: - Untreated - 15% 1st 24/24; 30% 1/12; ~3%/yr 2. DCI (VASOSPASM) - Major cause delayed M&M - Peaks 4-14 days 3. HYDROCEPHALUS (15-20%) 4. CARDIAC DYSFUNCTION (b/c catechol release) 5. Dec Na & Mg 6. Epilepsy/Seizures 7. Neurogenic Pulm Oedema |
|
|
Remote Anaesthesia |
- Remote location - Risks of unfamiliarity w location - drugs / equipment; Unstocked - Unfamiliar staff - Access to DI trolley - Other colleagues further away if emergency - Poor lighting - Difficult access to pt |
|
|
Factors affecting IOP |
- Tone extraocular muscles (sux ?signif) - Venous drainage - head position; neck ties - MAP & CVP - pressor response; induction - LA volumes in orbit (transient) - External compression - Drugs - Mannitol (vitreous fluid); Azetazolamide (dec ciliary body aqueous production) - Hypocapnia - vasoconstriction choroidal vessels (26-30) |
|
|
Pre-op Ophthalmic Surgery |
Most day cases; LA; on elderly pts with > 1 serious systemic disease - Axial length (<25mm) - INR/APTT - BGL if DM - Ability to lie flat 1hr (cough; OSA; arthritis; CCF) - Hearing/comprehension |
|
|
Innervation Eye |
Muscles - All CN3 EXCEPT SO (IV) & LR (VI
Sensation (inc ciliary gang) - CNV (V1 & V2)
CILIARY GANGLION: PNS - CN III SNS - Carotid plexus
|
|
|
Peribulbar block complications |
- Globe perf (0.01%) - Inc IOP (Use Honan balloon) - Retrobulbar injection (upper eyelid should not fall) - Muscular injection - Retrobulbar haemorrhage (0.07%) - Systemic - oculocardiac R; neurogenic syncope (monitoring essential) - Infection - Dural injection (use short needle 25mm) |
|
|
Subtenon's Space - anaesthesia, akinesia & visual blockade mechanism |
OR Episcleral space = Potential space ANAES - from blockade of short ciliary nerves (V1) as they traverse the space VISUAL BLOCKADE - direct flow of LA into dura invaginating CNII posteriorly AKINESIA - Direct flow of LA into muscle sheaths |
|
|
PROS & CONS Subtenon Block |
- Greater akinesia than topical or subconj LA - Rapid onset - Good & reliable akinesia (?5-15min) - Less pn (cf retro & peribulbar) - No sharp needle (globe perf; SA injection; Intraneural) - Don't need to cease anticoag (bleeding pts can be cauterised directly) - Can use in myopic pts (>26mm) - Can perform block in any of 4 quadrants
CONS - Special equipment; Skill; More invasive than topical; Chemosis; Subconjunctival harm (30%) - Relatively CI inferonasal pterygium -> red eye & poor cosmetic result - CI Scleral disease & previous vitrectomy (spread) |
|
|
WHY INFERONASAL QUADRANT FOR SUBTENONS? |
- Lack of insertion of extra ocular muscles - Surgeons tend not to use this approach (can't get into coronial plane b/c of nose) |
|
|
Equipment Classification for Cleaning |
CRITICAL - will penetrate skin or MM - require sterilisation SEMI-CRITICAL - will be in contact with intact MM or may become contaminated with readily transmissible organisms - high level disinfection or sterilisation NON-CRITICAL - Contacts intact skin or doesn't contact pt directly - low level disinfection or cleaning
NB Everything should be decontaminated 1st |
|
|
Levels of Checks |
LEVEL I - after servicing or new machine LEVEL II - Before list - High pressure (pipeline) & low pressure (flow & anti-hypoxia) - Breathing systems (leaks/valves) - Automatic Ventilator - VA (level/scavenging/leak/back bar) - Other (suction/Emergency/O2 cylinder/Laryng blades) - IV & LA delivery systems END - Documentation LEVEL III - If circuit change - leak test - Suction/Intub/Humid/Filters/Gas analysis/ Monitors |
|
|
MH DDx & Supporting factors |
- Awareness - Rebreathing - Sepsis - NMS - Ecstasy - Thyroid storm
Supporting MH - Sustained jaw rigidity; Generalised rigidity; Core T Inc of 2 deg/hr |
|
|
Dantrolene Dose |
2.5mg/kg Boluses Q10-15 min Up to 10mg/kg or more
NB Each vial is 20mg |
|
|
Draw Cross section of arm at axilla |
arm_cross_section_large_004.tif |
|
|
Axillary block - Subcutaneous Nerves |
Medial Brachial Cutaneous Medial Antebrachial Cutaneous Intercostobrachial |
|
|
Effects Pneumoperitoneum 1. IAP 2. CO2 |
CVS - 10-20 - initally auto transfusion of splanchnic circa -> Inc VR & CO - Then -> Dec VR & CO; Inc SVR; HR Inc or same (SNS - CO2 & Pain) - Inc myocardial work, may ......-> Ischaemia - IAP >20 -> Dec VR & CO +++ (If Vagal w rapid insuffl -> brady) RESP - Dec lung volumes & compliance - Inc V/Q mismatch - Inc risk barotrauma RENAL >15 -> Oliguria >20 -> Anuria
2. CO2 Load (Resp/CVS/CNS/ODC) |
|
|
Trauma Induced Coagulopathy Definition & Characteristics |
Def - Imbalance of the dynamic equilibrium b/n procoagulant factors, anticoag factors, plts, endothelium & fibrinolysus CHARACTERISTICS: - Factor V Inhibition - Systemic Anticoagulation (APC -> breaks down Va & Viiia; Antirepression of fibrinolysis) - Hyperfibrinolysis (Rx TXA) - Plt dysfunction
|
|
|
Trauma Coag Abnormalities Lab Results |
- Anaemia - Thrombocytopenia (Plt dysfunction difficult to test) - Inc aPTT & PT ( APC breaks down fa & 8a - essential cofactors in both pathways) - Low fibrinogen (aPC -> dec plasminogen activator inhibitor -> Inc plasmin -> fibrinolysis) - Inc D-dimers - TEG & ROTEM changes - may take 30-60min |
|
|
Mx Trauma Coagulopathy |
PRE-HOSP: - TXA (<3hrs) - Crystalloids <3L - Prepare products (ring ahead) HOSPITAL: - Early activation MTP 1:1:1 - Prevent & treat hypothermia & pH (33 & 7.2) - TEG to guide - Level 3 evidence - Optimal CO - Ca2+ if hypocalcemic - Factor VII - non-surgical bleeding & all correctables corrected
|
|
|
TEG result & Products |
Inc R time -> FFP (>10) Dec alpha angle -> cryo (<53 - rate of clot formation) Dec MA -> Plts (consider ddAVP) (<50) Inc LY30 = fibrinolysis -> TXA (%Dec in amplitude after 30 min)
|
|
|
AFE Risk Factors |
- Inc maternal age (>25) - Multiparity - IUFD - Maternal Hx of atopy/allergy - Chorio - Polyhydramnios - Microsomia - Strong or tetanic uterine contractions - Placenta accreta - Augmented labour |
|
|
AFE Clinical Features |
1. MATERNAL COLLAPSE (Consider other DDx) 2. RESP - APO (>90%); Dyspnoea; Cough; Bspasm 3. CVS - Arrest (>90%); HypoBP; Arrhythmia; RV ->LV failure; Cyanosis; CP 4. NEURO - HA; Seizures 5. OTHER - Foetal distress (100%); DIC; Uterine atonyA |
|
|
Anatomy Bronch - Levels of cricoid & carina (i.e. length of trachea) - Length & angles of main bronchi - Directions of lobar bronchi |
Tracheal Length (10-15cm): Cricoid C6 Carina T5 RMB - 25 deg; 2.5cm to RUL bronchus LMB - 45 deg; 5cm to LUL bronchus RIGHT ULB - 0300 MLB - 1200 LLB - 0600 LEFT ULB - 0900 LLB - 0600
|
|
|
Lung Segments (Bronchopulmonary) |
Right lung = 10 Left lung = 8 |
|
|
Obstruction post thyroidectomy - DDx |
SURGICAL: - Haematoma - RLNP - Tracheomalacia - Hypocalcemia (unlikely early) - PTX - Oedema ANAES: - Residual NMBD - Drug error - Over-sedation/opioids PT: - Anaphylaxis - Pre-existing CVS or resp disease - Developing resp disease (atelectasis; aspiration) - MI - Anxiety |
|
|
Opioid Oral Morphine Equivalents (OME) |
IV morphine 1mg = 3mg OME Fentanyl (transdermal or IV) 12mcg = 30mg Tramadol 5mg = 1mg OME Oxycodone 1mg = 1.5mg OME Codeine 10mg = 1mg OME |
|
|
Variable Bypass Vaporiser Safety |
1. AGENT SPECIFIC (Colour; Key indexed fill) 2. Interlock device 3. Pressure resistance/anti-pumping 4. Locking spindle (& o-rings to prevent gas leakage from back bar) 5. Anti-tilt measures, visible agent level 6. Automatically compensate for changes in ambientpressure 7. One-way check valve b/n vaporiser & O2 flush valve |
|
|
TAP Spinal nerve Levels |
T6-L1 |
|
|
Pre-Eclampsia - Definition & Criteria |
= HTN occurring after 20/40 & resolving within 3/12 of delivery w:
SBP >140 or DBP >90 PLUS at least 1 of: - Proteinuria (0.3g/day) - Renal impairment (inc pr & cr) - Liver disease - pn; inc transam - Neuro probs - seizures; visual disturbance; papilloedema - Haem disturbance - Plt; Haemolysis; DIC - Foetal growth restriction |
|
|
PET Risk Factors |
- PET Hx - Inc maternal age - Multiple pregnancy - High BMI - CT disorders - Protein C & S Deficiencies - Factor V Leiden - Hyperhomocysteine
|
|
|
Peribulbar Insertion Point |
Inferior orbital rim - junction of zygoma & maxilla - Insertion point is 1mm above rim & just lateral to this |
|
|
Peribulbar Block Complications |
- Globe perforation (<0.01%) - Inc IOP (Honan balloon) - Retrobulbar injection (stop if upper eyelid falls) - Muscular injection - Retrobulbar haem (0.07%) - Systemic complications (OG reflex; Syncope) - Endophthalmitis - Dural injection (use short needle) Don't insert >15mm |
|
|
Vasospasm Mx |
- GENERAL MEASURES (airway; T; O2; CO2) - SURGICAL - Optimise CPP - Triple H - no evidence; ?HTN alone - Nimodipine - Level 1 evidence 60mg Q4H - No evidence - Mg; Statins - Clazosentan - small RCT (endothelia antag) - RADIOLOGICAL (angioplasty; papaverine - refractory; |
|
|
Metabolic Syndrome Diagnostic Criteria |
Elevated waist circumference (population specific) Elevated triglyceride levels Reduced HDL-C Elevated BP (>130/85) - Elevated fasting glucose (>5.5) |
|
|
Dabigatran & Rivaroxaban MOA & Indications |
Dabigatran = Oral direct thrombin inhibitor (Pradaxa)
TGA Approved Indications: - Prevention of VTE post major ortho surgery LL (PBS) - Non-valvular AF & at least one additional RF for CVA (Non-PBS)
Rivaroxaban = oral factor Xa inhibitor Indications - as above + treatment & prevention of recurrent VTE
|
|
|
Dabigatran Guidelines if bleeding |
- Optimise renal function - Check for drug interactions - Check FBC, U&E, Ca, APTT, TT & fibrinogen MOD BLEEDING: - Fluids to maintain UO - If Plt <80 or on anti-plt - consider Plts - Charcoal if <2hrs SEVERE BLEEDING: - As above PLUS - consider TXA - If critical - consider Recombinant FVIIa (50mcg/kg) - note short T1/2 - Dialysis - may remove 60% |
|
|
Dabigatran pre-op cessation & RA |
High bleeding risk (cardiac; spinal; neuro; abdo) - stop for 5 days
Low bleeding risk - eGFR > 50 - 2 days - eGFR > 30 - at least 3 days - <30 - 5 days & don't restart
Neauraxial - CI unless normal TT; & 24hrs post removal of catheter |
|
|
Fat Embolism Clinical Features |
Either fulminant or gradual Typically - 1F2-36hr post injury RESP - Inc PA pressures - Hypoxia.... Resp failure CUTANEOUS - Petechial rash (50-60%) - Upper half body/MMs/conjunct NEURO - Drowsiness/Coma/Seizures - Global dysfunction
MINOR SIGNS - HTN; Fever; Tachy; Oliguria; Jaundice; Retinal petechiae |
|
|
Fat Embolism Prognosis & RFs |
10-44% require ventilation Pulm - resolves 3-7 days Mortality 1-20% RFs: - Delayed ORIF (LLs > ULs) - Intramedullary fixation - Bone marrow necrosis; Sickle cell crisis; Acute pancreatitis
|
|
|
Hyponatraemia Causes |
HYPOVOLEMIC: - Renal H2O loss - CSW; Salt-losing nephro; Addisons - 3rd space - pancreatitis; burns; cirrhosis - Sweating/D&V - normal H2O intake EUVOLEMIC: - SIADH (drugs; malignancy; CNS) - Polydipsia; Amphet HYPERVOLEMIA: - Cirrhosis; CCF - Hypothyroidism - Renal failureH - Nephrotic syndrome PSEUDO: - When there is an osmolar gap (BGL; Glycine; proteins; lipids) |
|
|
Hyponatraemia Ix |
For hypo or hypervolemia: - Urinary Na to differentiate causes For Euvolemia: - Urine vs serum osm (SIADH Urine>Serum; all other causes opposite) |
|
|
Placenta Praevia: - Chance of Accreta - Risk of caesar-hysterectomy if accreta/percreta |
PP w: 1 previous LSCS - 30% 2 previous LSCS - 50% Risk hysterectomy: Accreta - 66% Percreta - 95% |
|
|
APGAR |
Out of 10 (0/1/2) APPEARANCE - Blue / Blue extremities / Pink PULSE - None / <100 / >100 GRIMACE - None / Feeble / Cry, pulls away ACTIVITY - Floppy / Some flexion / Flex & ext RESP - Apnoiec / Weak, irreg / Strong cry
Normal >7 Fairly low 4-6 Critical <4 |
|
|
NEONATAL RESUSC |
1. Ax - APGAR; Estimate gestation & ?meconium
2. If HR <100 / not breathing or crying -> ventilate (5 inflation breaths; then RR 40-60; 30cmH2O)
3. If HR < 60 OR not improving after ventilating for 30 seconds -> start CPR 3:1 every 2 sec & consider intubation
4. VENOUS ACCESS - adrenaline & fluid bolus 5. CHECK BGL 6. VT/VF - 4J/kg shock/2 min - Consider amiodarone; Atropine
Possible causes - PTX; Congenital heart or lung prob; APH |
|
|
Hazards of Laser |
1. Airway fire (Ignition) 2. Hypoxia (inadequate ventilation or distal debris/smoke/secretions) 3. Laser plume (PVR/ciliary/aerosolisation) 4. Soft tissue burns - pt or staff - cutaneous or adjacent to surgery 5. Eye damage (retina) - patient & staff 6. Gas embolism (gas coolant in Nd:YAG)
|
|
|
Laser - Minimising Hazards |
PATIENT: - Eye protection - Protect surrounding tissue - Laser compatible airway (tube or tubeless) - Minimise combustible gas (FiO2<0.4; N2O) - Flame resistant surgical drapes - Matte surgical instruments - Scavenge plume - Avoid plastic tape (combustible) STAFF: - Education/accreditation - Laser officer/protocol/signs & light on OT door - PPE - goggle/masks - Availability of non-water extinguisher |
|
|
Problems with Laser Tubes |
- Narrow ID as have thick outer walls -> difficult SV & higher airway pressures |
|
|
Airway Fire |
1. Disconnect O2 source Switch off LASER & flood site with saline If feasible remove tube Ventilate with air (BMV) w filter (smoke) Ensure keep anaesthetic going (TIVA) - if using VA CO2 extinguisher After fire extinguished - look with rigid bronch Arrange HDU/ICU If fire continues- follow local hospital protocol |
|
|
What does LASER stand for? |
Light Amplified Stimulated Emission of REadiation |
|
|
Effect of Magnet on PMs & AICDs |
PMs - Asynchronous (fixed rate) AICD - Disables anti-tachycardia function ICD+PM - Only disables AICD |
|
|
Peri-op plan PMs/AICDs & EMI |
EMI likely? - Switch of anti-tachycardia fx - Use bipolar - If mono polar - short bursts or low energy - Plate placed so current not within 15cm of heart - Does PM need programming to asynchronous mode (PM dependent & EMI close to PM) or disabling of special algorithms? - Disable AICD fx |
|
|
SAH Grading |
|
|
|
Rate of re-bleed SAH (untreated) |
24/24 15% 1 month 30% 3%/yr thereafterS |
|
|
SAH Complications |
|
|
|
ECG changes SAH |
ST changes Inc QT TWI U waves |
|
|
Nimodipine dose, duration, SEs & mortality benefit |
|
|
|
Vasospasm & DCI Definition, RFs & incidence |
Incidence 60% SAH (leading cause of M&M) DCI = Neuro deterioration related to ischaemia. Lasts >1hr & has no other cause Vasospasm = Arterial narrowing demonstrated angiographically on doppler US, w corresponding S&S RFs:
|
|
|
Classification TBI |
Mild / Mod / Severe (GCS) 13-15 / 9-13 / <9 |
|
|
Normal ICP? |
5-15mmHg |
|
|
Hyperosmolar therapy for ICP? Limits |
Mannitol 0.25-1g/kg (5ml/kg of 20%) (Osm < ?320) - renal damage
3% saline 5ml/kg (Na <155)
OR 20ml of 20% |
|
|
DI Diagnosis |
UO >50ml/kg/day OR >3L/day
High serum osm (>305) & Na (>145)
With abnormally low urine ism (paired)
ADH level
Desmopressin test - will work for neurogenic (= >50% increase in urine osm) MRI - for cause |
|
|
Risks of SC damage intra-op & Risk minimisation |
Minimising:
|
|
|
Monitoring SC function |
'Wake-up' test SEPs
MEPs
|
|
|
VAE Monitor Order of Sensitivity |
1. TOE 2. Praecordial doppler 3. PAP/Minor HR & BP 4. ETCO2 5. ETN2 6. RAP - Significant haemodynamic 7. Echo - CVS collapse |
|
|
Cushings Anaesthetic Implications |
CVS - HTN ......-> LVH ; ECG (TWI; high voltage) - reverts once corrected RESP - OSA/obesity; Myopathies (weaning) AIRWAY - OSA; GORD METABOLIC - Electrolytes & DM OTHER - Often obese w difficult access
|
|
|
Types of Adrenal Insufficiency |
PRIMARY (Addisons) -> Dec glucocorticoids; mineral; androgen Causes - Auto-immune; Infection; AIDS; Mets SECONDARY - Failure of CRH (hypoth) or ACTH (pit) or suppression ->glucocorticoid deficiency only Causes - Iatrogenic (pit surgery; glucocorticoids) S&S - Cut & mucosal pigmentation - primary only - Weakness/fatigue/anorexia/N&V/abdo pn - Myalgia/jt pn - Hypovolemia - Dec Na & BGL; Inc K
|
|
|
What is synacten |
Synthetic ACTH Tests whole HPA axis |
|
|
Treatment Addisons |
Hydrocort 20mg mane, 10mg nocte Fludrocortisone 0.1mg (replace aldosterone) |
|
|
Addison's Crisis |
Causes - Stress in chronic insufficiency w/o replacement S&S - Hypovolemia; Dec Na & BGL; Inc K & Ca Mx - 100% O2 - IV fluids - colloids; NS & glucose - Hydrocort 200mg stat; 100mg tds - Inotropes & vasopressors |
|
|
Steroid Replacement |
All meds up to morning of surgery Hydrocortisone 25mg IV at induction, then: - Minor surgery - nothing required (e.g. hernia) - Intermediate - 25mg Q6H IV for 24/24 - Major - 25mg Q6H for 48-72/24
|
|
|
Brain Death Definition & 3 essential findings |
Def = Irreversible loss of all function of brain 3 essential findings:
|
|
|
Brain death Preconditions |
|
|
|
Brain death Testing |
Independent examination by 2 suitable trained & experienced doctors (can't be transplant team)
Test (CN)
|
|
|
Bypass Circuit |
|
|
|
ICP trace |
|
|
|
Hypothermia effect on metabolic rate |
Decrease 7% for every degree drop |
|
|
ASA & mortality |
Originally used to Ax pre-op status of pts Studies have shown a correlation between ASA & post-op adverse outcomes
Mortality Data 1 - 0.05% 2 - 0.4% 3. 4.5% 4. 25% 5. 50% |
|
|
What affects thermodilution accuracy from PAC? |
|
|
|
PAC waveform |
|
|
|
Cardiac Index Formula & Normal Values |
= SV x HR / BSA
Normal range 2.5-4.2L/min/m2 |
|
|
CEA Indications & Timing |
>70% stenosis (NNT = 6) Maybe - >50% w low surgical risk (M&M <3%)
TIMING NICE guidelines - Within 2 weeks of TIA/CVA, & <48hrs if possible
|
|
|
Rheumatoid Arthritis - Who to Xray C spine |
Flexion/extension views in: - Pts with neurological symptoms or signs - Those with persistent neck pain - role of X-ray is controversial & interpretation is difficult MRI/CT to assess cord compression
Unless certain that C-spine is stable - treat all RA pts as if they might have an unstable spine |
|
|
Atlanto-axial subluxation - Types & incidence |
Order from most common to least: Anterior - 80% (significant if gap >3mm b/n odontoid & atlas) - neck F worsens Vertical - odontoid moves up foramen magnum Lateral - uncommon (>2mm significant) - spinal n & vert @ compression Posterior - rare - neck E worsens
Subaxial (below C2 >2mm significant (suspect if fusion at higher level) |
|
|
CEA LA vs GA & points for LA |
GALA trial LA vs GA: - No signif difference for CVA & mortality rates - Possibly long term benefit for LA - lower cognitive impairment
LA
|
|
|
Hyperperfusion Syndrome post CEA RFs |
Rx - Aggressive Rx of HTN |
|
|
Renal Protection Strategies AAA |
PRE-OP
INTRA-OP
POST-OP
|
|
|
Non-Surgical Mx AAA |
Aspirin (level 1) Stop smoking (slows growth) Statins Consider B-B & ACE-i in high risk |
|
|
Define Anaesthesia Dolorosa |
Pain in an area of numbness |
|
|
Neuropathic Pain Def |
Pain caused by a lesion or disease of the somatosensory nervous system
More up to date version |
|
|
Consent - BRAN |
Benefits Risks Alternatives Nothing |
|
|
Cardiac Ablation Complications |
ABLATION Cx:
ANAESTHESIA Cx: Hypotension Suppression of arrhythmia (partic VA) Airway complications; Positioning
Overall Mortality 1:1000 Age > 75 & CCF - assoc w complications
NB Rate of long term arrhythmia control or cure ~70% |
|
|
CM5 ECG configuration - where are electrodes placed? |
C = Clavicle - neutral lead (left leg) - can be placed anywhere, but usually placed over clavicle M = Manubrium - RA lead 5 = LA on V5 Select lead one - gives vector pretty much straight down direction of conduction |
|
|
CS5 Configuration |
Central Subclavicular Lead RA on (R) clavicle (C) LL - ground (anywhere) LA on V5 Lead I - anterior ischaemia Lead II - inferiorSen
Best & easiest alternative to a true V5 lead for monitoring ischaemia |
|
|
Sensitivity of ECG leads |
5 lead: II, V4 & V5 - 96% (however can't select 2 chest leads with our monitors) II & V5 - 80%
When only one praecordial lead can be chosen - Choose most isoelectric |
|
|
MPS - Info provided - PPV & NPV |
INFO: 1. Perfusion 2. Structure - wall thickness 3. Function - EF NPV 99% PPV 10-20% |
|
|
MPS - Not indicated |
|
|
|
MPS Indications |
AS PART OF AHA/ACC NON_INVASIVE TESTING
|
|
|
Benefits MPS |
|
|
|
MP Score Sn & Sp |
~60% alone |
|
|
LASER = |
Light Amplification by Stimulated Emission Radiation |
|
|
Ax RLN nerve Post-operatively |
1. R/V NOTES - intubation difficulty; VC pre-intubation 2. VOICE CHANGES (Sn 33%; Sp 75%) 3. LARYNGOSCOPY - direct & indirect (nasendoscopy/video) 4. USS - Established validity 5. LARYNGEAL EMG - prognosis & distinguish paralysis vs cricoarytenoid jt damage (ETT)
NB Innervates all muscles of larynx except cricothyroid (superior laryng) B/L incomplete more dangerous than complete |
|
|
Atlanto-axial Instability Conditions |
RA Downs AS Trauma Osteogenesis imperfecta |
|
|
Cocaine Toxicity |
MOA - SNDRI Biphasic response - low concentration -> brady; high ->HTN; tachy; coronary spasm Cx & Mx:
|
|
|
OSA Associated Conditions (that cause) |
|
|
|
Conditions Assoc with Difficult Intubation |
|
|
|
Difficult Intubation Definition |
ASA (1993) Proper insertion of ETT with conventional laryngoscopy that requires more than 3 attempts &/or >10 minutes Incidence - 1-2% (Failed 0.3%)
Difficult Laryngoscopy = C&L Grade 3-4 view |
|
|
Examination Findings to Predict Difficult Intubation |
1. MP Score - Visibility of soft palate & uvula
2. Mouth opening - <2.5cm = difficulty 3. Mandibular mvt - trismus; Protrusion A/B/C (B = Teeth edge to edge) 4. Incisors & oral cavity - high arched palate; oral tumours 5. Neck & TMD - <6cm - v. difficult (PPV 75%) 6. Body Habitus - OSA; Neck circ >40cm; Large breasts; ability to BURP; Pregnancy |
|
|
Failed Intubation - CICO |
1. Call for help Consider:
2. Cease further intub attempts (trauma) 3. BMV manoeuvres & adjunts
4. Insert SGA - LMA 5. Emergency Airway Access - perc or surgical trache.
NB if Successful ventilation/O2 steps 3-4 - move to non-emergency pathway |
|
|
Failed Intubation - Can Ventilate/Oxygenate |
Non-Emergency Pathway:
Alternative approaches to intubation
If failure - wake pt or proceed to emergency airway if can't wake (i.e. emergency surgery) |
|
|
Emergency Case - CICO |
Same as elective pathway except:
Aspiration risk - Cricoid pressure maintained t/out unless think that releasing will improve view - Possible use of sux (i.e. rapid wake up with sugammadex not an option)
Basically same except risk of aspiration & ability to wake up not as clear an optioni |
|
|
iLMA Sizes of ETT to fit |
LMA 3/4 - ETT 6.0 LMA 5 - ETT 7.0 |
|
|
Smoke Inhalation - Ax of Damage |
Upper Airway Thermal
Lower Airway Thermal
Noxious Gases
NB 100% O2 - reduces T1/2 CO 4 hrs -> 45min |
|
|
Smoke Inhalation - Intubation |
|
|
|
CI to Cricoid |
|
|
|
Obesity Classes |
From BMI: Pre-Obese 25-30 (overweight) Class I - 30-35 Class II - 36-40 Class III - 41-49 (extreme obesity) Super morbidly obese >45P
|
|
|
Predictors of DI in Obese |
|
|
|
RFs for Aspiration |
Greatest risk - Emergency surgery; Light Anaesthesia; Abdominal pathology; Obesity
OTHER PATIENT - Increased gastric content (fasting; opioids; obstruction); LOS (pregnancy; GORD); Laryngeal reflexes (TBI; bulbar); Female; Elderly SURGICAL - Pneumperitoneum; Lithotomy ANAES - Difficult airway; BMV ->gastric; LightA |
|
|
Aspiration Mx |
1. Minimise further aspiration (suction; position; cricoid) 2. Secure airway 3. Suction - Trachea; Bronch 4. CXR (25% NAD initially)/HDU/ICU (if SpO2 <10% of pre-op; tachycard or tachyp; CXR changes) 5. ABs only if develop pneumonia (targeted)
No steroids |
|
|
Eye Muscle Cone - Contents |
CN V - V1 (nasociliary branch only)
- Sensory fibres (V1) - PNS (CN III) - SNS (carotid plexus)
NB Formed by all muscles except inferior oblique NOT IN CONE - CNIV; Other V1 branches/V2 (frontal & lacrimal sensation to peripheral conjunctiva/lower lid) Apex of cone = annulus of Zinn |
|
|
Gabapentin - MOA & PK/PD |
MOA - Not completely understood - Effect on VG-Ca channels - Postulated - enhanced inhibitory input of GABA-mediated pathway; NMDA antagonism Oral prep only!
PK: BAV high but varies w dose; TDS dosing; Nil metabolised (renal excreted)
PD: Sedation (20%); Dizziness (18%); Ataxia; Fatigue; Convulsions (1%)
|
|
|
Gabapentin in Acute Pain - the evidence |
Level 1 evidence - single pre-op dose:
|
|
|
Gabapentin in Chronic Pain - evidence |
Level 1 evidence:
Limited evidence for other chronic post-surgical pn states |
|
|
Pain History |
Nature Location Intensity Duration Onset/Offset Associated Symptoms Aggravating/Relieving Radiation Functional Impairment
|
|
|
Mx & Prevention of Phantom limb pn - evidence |
PREVENTION - Epidural reduces incidence; Ketamine reduces severity (cont for 3/7)
Rx - MDT & Multimodal:
|
|
|
Analgesia & Antiemetics Classification Pregnancy |
A - Paracetamol/Bupivacaine/Lignocaine/Codeine /Metoclopramide B1 - Ropivacaine/Gabapentin/Granisetron B2 - Domperidone/Hyoscine B3 - Clonidine/Ketamine C - Other Opioids/Aspirin/Promethazine D - Anticonvulsants/Paroxetine
NB Opioids - Short term treatment appears safe - at a minimal dose (concern - neonatal abstinence syndrome) |
|
|
Pregnancy Drug Classification |
A - Safe in large number of pregnant women B - Appears safe in humans - variable safety in animals: B1 - Safe in animals B2 - May be unsafe in animals B3 - Appears unsafe in animals C - Have caused, or suspected of causing harmful effects in foetus without causing malformation D - Have caused, or suspected of causing foetal malformations or irreversible damage X - Such high risk of foetal malformation that shouldn't be used if any chance of pregnancy |
|
|
Classes of drugs in persistent pain? |
Simple analgesics Anticonvulsants (Old - carbamazepine; valproate - level I; New agents - gaba; lamotrigina - Level III-IV) Antidepressants (TCAs - level I) Membrane stabilisers e.g. some anticonvulsants; lignocaine (level II) Opioids |
|
|
Assessing pain in dementia pt - methods |
Both understanding of scores & ability to communicate impaired
NB Vital signs are not accurate reflection |
|
|
Problems with naltrexone |
Naltrexone = opioid antagonist Long DOA (T 1/2 14hrs) May have up regulation of opioid Rs Opioid beneficial - Co-induction; Sole anaes agent ('CVS stable'); Balanced GA
Cease 24-48hrs if possible If not able to cease: Intra-op - consider lignocaine or esmolol; Increase induction agent dose; alternative analgesia; BIS; Remi Post-op - Regional; Multimodal; Adjuncts |
|
|
Mortality for lobectomy vs pneumonectomy ppo FEV1% for above + wedge resection |
Pneumonectomy 6-8% Lobectomy 2-4%
ppo FEV1%: Pneum 55% Lobectomy 40% Wedge resection 35% |
|
|
Checking DLT |
R vs L 1. CLINICAL
2. FOB
3. CXR
4. CAPNOGRAPHY/SPIROMETRY |
|
|
RFs RDS Thoracic Surgery |
|
|
|
Blood Loss Trauma Causes |
SCALPeR
S = Scalp (esp children) C = Chest A = Abdomen L = Long bones, esp femur P = Pelvis R = Retroperitoneal |
|
|
Pulse palpation & approximate BP |
Only carotid - SBP 60-70 Only carotid & femoral - 70-80 Carotid, radial & femoral - 80-90
Always disappear in that order - but values vary individually
|
|
|
Haemorrhage Adults - Estimating amt |
Grades I - IV based on % blood volumes: 15 - 30 - 40 - >40 (game over)
Don't really bear out in reality - age/comorbidities /Meds (e.g. BB) |
|
|
Final common pathway coagulation |
Prothrombin (2) -> Thrombin (2a) -> Fibrinogen -> Fibrin Fibrin + platelets = platelet-fibrin matrix = Haemostasis Extrinsic (7a) - converts 10 ->10a |
|
|
Recombinant Factor VIIa Pros & Cons |
PROS:
CONS:
|
|
|
Approach to using rFVIIa |
Use in life-threatening bleeding & MTx. Consider use in ICH Consider when pt has had:
Dose - 100mcg/kg - round up to nearest 1.2mg vial. Wait 20min - repeat |
|
|
TRAUMA - ATLS Approach |
Primary Survey - ABCDE + avoid secondary insult AMPLE / MIST A - Airway maintenance & C-spine B - Exposure & inspection - Chest surgical emphysema/Tension (may only become apparent after PPV) C - Permissive low BP (poor evidence) - but SBP <90 -> mortality increases x2; Find the bleeding & stop it (remove all bandages); IV & Ix D - GCS; AVPU - Severity of TBI; Is suspect spinal -> priaprism & anal sphincter tone; BGL E - T/Expose/log roll Adjuncts - FAST; XR; OGT; IDCT Secondary Survey - Top to Toe O/E |
|
|
Trauma - Deadly Dozen |
Lethal Six
Hidden Six:
|
|
|
Laryngeal Cartilages |
3 Unpaired:
3 Paired:
Membranes:
Thyroid gland:
|
|
|
TPN Complications |
Related to CVL:
Related to metabolic effects:
|
|
|
Classification of Shock |
|
|
|
ScvO2 Pros & Cons |
Normal O2 extraction 25-30% - corresponds to SvO2 >65% Intermittent or continuous Pros:
Cons:
|
|
|
Timing of Smoking Cessation & Changes |
One day -> Decreased COHb & nicotine (expect increased tissue O2 delivery) 3/52 -> Wound healing 6/52 -> Sputum volume & pulmonary function 6/12 -> Immune function
Ask Advise Refer
Following abdo surgery - 6x increase in resp complications |
|
|
Pneumothorax Causes |
1. Spontaneous - Primary - healthy, no lung disease; often tall smokers - Secondary - Underlying lung disease 2. Traumatic - High inflation pressures - Complication of surgery/Iatrogenic
Risk of recurrence of spontaneous PTX is 54% at 4 yrs |
|
|
Common Peri-op nerve injuries of UL |
Aetiology - Stretch; Compression; Ischaemia; Metabolic derangement; direct trauma (needle, diathermy); LA injection |
|
|
RFs for Peripheral Nerve Injury |
PATIENT
ANAESTHETIC
SURGERY
|
|
|
Failure to Emerge from GA - Causes |
4 S's
Sedatives/Drugs
Stroke/CNS
Seizures
Sudden metabolic/endocrine derangement
|
|
|
Anti-emetic Rx for PONV |
If prophylactic drug failed - use anti-emetic from a different class Re-administer if >6hrs in PACU Don't re-administer droperidol? |
|
|
Impaired Colleague |
DEF - Inability to safely & competently practice anaesthesia at a standard appropriate for a given environment
|
|
|
Decreasing risk of awareness |
1. BDZ pre-med 2. Dont titrate anaesthetic agents to CVS or resp depression 3. EtVA >0.8MAC 4. Only use when required NMBD 5. BIS/entropy - in high risk patients (B-aware trial) - LSCS; Emergency; Hx previous awareness OR clinical signs of awareness may be masked |
|
|
OHGs |
|
|
|
Peri-op Probs DM |
|
|
|
Required to cough? |
VC should be twice TV |
|
|
Rheumatoid Arthritis - Anaesthetic Implications |
C-Spine
Airway
Drugs
CVS
Resp
Haem
Hepatic & Renal
Vasc Access
RA
Other
|
|
|
Bone cement implantation syndrome - Grades |
Methyl methacylate
Grade 1 - Mod hypoxia or hypotension Grade 2 - Severe ditto OR unexpected LOC Grade 3 - CVS collapse |
|
|
DIC |
Disseminated Intravascular Coagulopathy Widespread activation of coagulation -> consumptive coagulopathy LAB:
Rx:
|
|
|
Pk of Dabigatran & Rivaroxaban |
Dabigatran: Prodrug - converted by plasma esterases T1/2 (hrs) - dependent on renal function & increases w chronic dosing - Normal = 14; Mild-Mod = 16-20; Severe = 30 Elim = 80% renal; 20% metab (active metab) Monitoring - aPTT or TCT Rivaroxaban: T1/2 (hrs) - 7.5 (with severe renal impairment = 9.5) Elim - 33% renal; 66% metab Monitoring - PT or anti-factor Xa assay |
|
|
Rivaroxaban vs Warfarin Effects |
R vs W:
CVA reduction w AF: 1.7 vs 2.1%/yr ICH bleeding - R < W GIT & bleeding requiring Tx - R > W
|
|
|
Dabigatran vs Warfarin Effects & SEs |
D vs W:
VTE/death post TKR - D = W CVA/emboli w AF: Lower dose - D = W effect; D < W bleeding Higher dose - D > W effect; D = W bleeding (although W - ICH more common & D - GIT more common)
NB DABIGATRAN - CI w prosthetic heart valves (trial terminated early as increased thromboembolic events - valve thrombosis, CVA, MI, & bleeding > W) |
|
|
Neuraxial Guidelines for Dabigatran & Rivaroxaban |
ASRA - Avoid European - 24hrs post dose for insertion & removal for R (D - CI); Dose after removal - 6hrs TGA - D - CI for insertion, but dose 2hrs post removal. R - 18hrs for insertion/removal post dose; and dose 6hrs post removal
|
|
|
Spinal USS - Steps |
|
|
|
Substance Abuse Management |
2. Initial response to suspected misuse
3. Follow-up
|
|
|
Specialist Referral for Burns |
|
|
|
Modified Parkland Formula |
%BSA x 4ml x weight = 24hr fluid
Give half in 1st 8hrs, half n next 16hrs
Burns oedema maximal in 1st 18-30hrs Re-assess fluid needs w CRT, mental state & UO
Don't forget to treat pain |
|
|
RSI Steps |
1. Equipment - machine, drugs, airway, suction, IV access 2. Assistance - cricoid + airway 3. Monitoring 4. Pre-oxygenate; Aspirate NG 5. Induction 6. Intubation |
|
|
Dose & drugs for caudal |
Bupivacaine 0.25% 1ml/kg - long DOA; Motor blockade short time may be helpful (levi & ropiv not licenced) Adrenaline 1: 200 000 - Slightly increases DOA; IV; decrease absorption (minor); Con - ?arachnoiditis Fentanyl - Aids quality; Cons - opioids SEs |
|
|
Apnoea RFs paediatrics |
|
|
|
Physiological anaemia of pregnancy - nadir
|
Birth 16-18g/dL Nadir 3 months - 9-10g/dL By 8 months - 12
|
|
|
Maximal allowable blood loss calculation Paediatric blood volumes |
pre-op Hb - trigger Hb/pre-op Hb x EBV
Estimated blood volume (EBV): Preterm 90-100ml/kg Term 85-90 Infants 80 School age 70 Adult 70 |
|
|
Risks of Epidural with numbers |
Reversible 1:500 Neuropraxia 1:1000 - 1:10000 Paralysis 1:200000 11. Abscess 1:25000 12. Haematoma 1:150000 |

