![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
N2O is stored as a liquid under about ____ PSI.
|
750
|
|
|
|
Gases are regulated to a typical operating pressure of ___ PSI.
Some machines further reduce operating pressure to ≈ ___ PSI. |
50
16 |
|
|
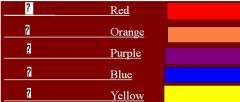
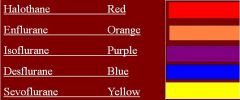
Label
|
|
|
|
label
|
|
|
|
|
|
|
|
|
Infrared analyzers can detect _______ gas.
Ionizing leak detectors identify __________________---require frequent calibration. Mass spectrometers, gas chromatography and photo-spectrometers can also be used. |
nitrous oxide
halogenated hydrocarbons |
|
|
|
The circle system advantages
|
This is the most widely used circuit in use today.
Low flow rates are needed from the fresh gas outlet (economy). Warming and humidification are achieved from the reactions in the CO2 absorber Reduced chance of overflow and therefore reduced pollution of theatre |
|
|
|
Low flow technique
The operator can allow _____ LPM of fresh gas into the circuit to produce minimal re-breathing. This is fine as long as a minimum of ___% O2 is maintained in the circuit |
2 to 3
25 |
|
|
|
Flows of _____mL/min of pure oxygen, are all that is needed to maintain metabolism. This low a flow will require that agent concentration is monitored very carefully (under target concentrations are possible).
|
200 to 300
|
|
|
|
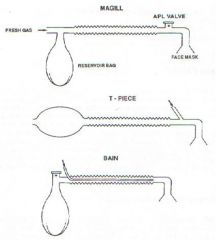
No CO2 absorber in the circuit therefore flow must be high enough to meet pts. minute ventilation. (100mL/kg)
Not practical for controlled ventilation |
Magill Circuit
|
|
|
|
No CO2 absorber in the circuit therefore flow must be high enough to meet pts. minute ventilation.
Plastic version is used in some head and neck surgery. Somewhat better in PPV than Magill. |
Bain Circuit
|
|
|
|
Very simple in design
Low resistance Was once popular for pediatrics Fresh gas flow of 2 to 3 times the normal minute ventilation is required to eliminate re-breathing. To and Fro: Has CO2 absorber near Pt. therefore limited resistance---cumbersome---not popular. Non-rebreathing circuit: Reservoir bag should be nearly full before inspiration and not quite empty after |
Jackson Reese (modified T-Piece)
|
|
|
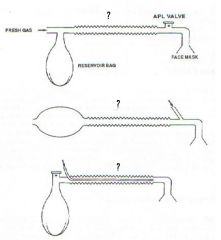
Which circuit is which
|
|
|
|
|
_____ is a coaxial circle system, with the inspiratory limb contained within the expiratory. Like a Bain, it is less bulky, and may offer more heat and humidification of the inspired gases. Like the Bain, disconnection or kinking of the inner limb causes a huge increase in dead space and respiratory acidosis dioxide from the patient's exhalations
|
King Circuit
|
|
|
|
EtC02 Mainstream:
|
Inline with subject’s exhaled gas via ETT
Can pull on the airway (heavy) Slight increase in deadspace |
|
|
|
EtC02 Sidestream:
|
Sample rate ~150mL/min
Slight lag in response time Slight increase in deadspace Sample line can occlude with condensation, some units have heaters to reduce condensation |
|
|
|
|
|
|
|
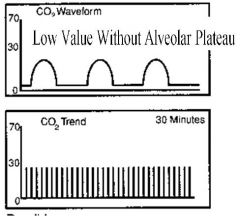
Shallow and Rapid breathing
PeT02 |
Partially mixed alveolar CO2 with dead-space gas
Very small Vt may cause ↑ PACO2 but a ↓PETCO2. This may hinder usefulness during weaning etc. |
|
|
|
Leak around ETT
|
unchanged PACO2 but ↓PETCO2
|
|
|
|
Leak in sampling system
|
unchanged PACO2 but ↓PETCO2
|
|
|
|
Increase in V/Q -Ventilation in excess of Perfusion
Decreased PACO2 Examples |
Pulmonary Embolism
Decreased C.O. Hypovolemia Severe Hypotension Cardiac Arrest |
|
|
|
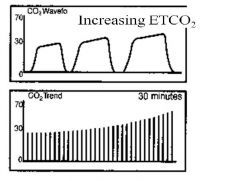
Increased PETCO2
|
Decreased Alveolar Ventilation (VA)
Hypoventilation Decreased minute ventilation (VE) Increased CO2 production: shivering, pain, fever etc VA=VE-VD |
|
|
|
Decreased PETCO2
|
↑ VA ----well above metabolic need
Very low Vt, approaching dead-space volume Low perfusion / emboli / ↓ cardiac output |
|
|
|
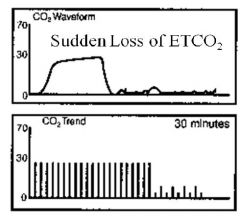
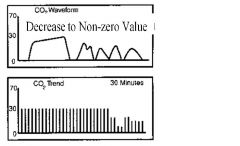
Disconnected circuit or apnea.
|
|
|
|
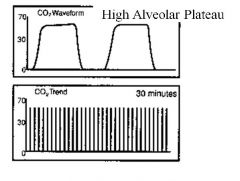
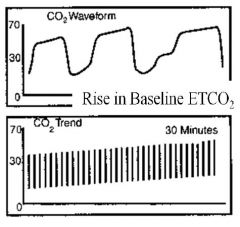
Hypoventilation
--high plateau |
May also see rising slow speed baseline
|
|
|
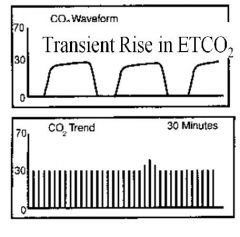
Increased CO2 production, (exercise, stress), decreased removal, perhaps improving CO, if increasing to near normal.
|
|
|
|
Early airway closing
Small airway disease Eg. COPD |
|
|
|
Erratic exhalation
Post op ? |
|
|
|
|
Opening of previously closed lobe/lobule. ?
|
|
|
|
Opening of previously closed lobe/lobule. ?
|
|
|
|
Re-breathing CO2
|
|
|
|
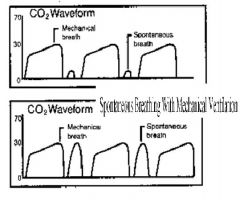
Very small Vt. Didn’t trigger vent.
Good sized Vt interspersed with Vent breaths. R Rate? Mode ? |
|
|
|
Why is PetCO2 possibly erroneous during a SBT?
|
Weaning pts seldom hyper-ventilate if pain/fear/anxiety is under control.
|
|
|
|
Anesthesia is ________
|
“A state of reversible loss of sensation and unconsciousness”.
|
|
|
|
Stages of anesthesia
Stage1. Stage2. Stage3. Stage4. |
Stage 1--Analgesia: Beginning of drowsiness to the loss of the eyelash-flick response.
Stage 2--Excitement: Agitation, irregular resps, delirium, salivation, dilated pupils, leading to regular (or brain stem) resps. Stage 3: Surgical Anesthesia: Four Planes Stage 4: Impending Death: Circulatory collapse signifies medullary dysfunction. |
|
|
|
Planes of Surgical Anesthesia
Plane 1. Plane 2. Plane3. Plane 4. |
Plane 1: Regular resps, REM
Plane 2: Cessation of REM to partial paralysis of the intercostal muscles. Plane 3: From partial intercostal to full intercostal paralysis. Plane 4: From full intercostal paralysis to full diaphragmatic paralysis, and therefore apnea. |
|
|
|
3 Main Components of Anesthesia
|
1)Unconsciousness
Patient may well be oblivious to all sensation but autonomic reflex to pain can still occur. 2) Analgesia ‘Areflexia’---reaction to pain, tachycardia, diaphoresis, etc are reduced or absent. 3)Muscle relaxation Surgery on extremities requires minimal relaxation where thoracic/abdominal requires profound relaxation of all muscle groups. |
|
|
|
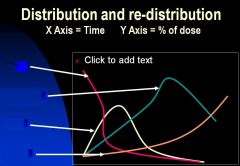
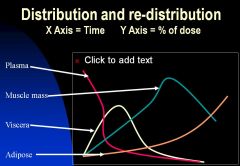
Regional Blood Flow
|
Vessel rich viscera; 70%
Brain, heart, liver, kidney Muscle; 25% Adipose tissue; 4% Vessel poor tissue; 1% Skin, cartilage, bone |
|
|
|
|
|
|
|
Ketamine (Ketalar)
|
Produces a dissociative mental state:
Catalepsy---trance-like state with muscle rigidity Sedation Amnesia Analgesia |
Given IV or IM in 1-2 mg/Kg dose over 1 minute.
Duration of action is 5-10 minutes. Converted in liver and excreted by kidneys. Pt can maintain airway, used in burns, Peds Dx. BP (20-40mmHg), and HR, may ICP Pts need dark, quiet room to recover as can cause hallucinations/bad dreams (emergence delirium). |
|
|
Propofol (Diprivan)
|
Loading dose; 1.5 to 2.5 mg/kg
Rapid redistribution and elimination make it helpful in out-patient procedures. Anti-emetic, Lack of cumulative effect is helpful for total IV anesthesia. May cause transient apnea with reduced response to O2 and CO2 ---no bronchospasm (maybe broncho dilation). May cause vivid dreams and sexual fantasies during emergence. |
|
|
|
Thiopental (Sodium Pentothal®)
|
Short acting barbiturate used to induce unconsciousness. No analgesic action.
Slow injection to allow for ‘dose to action titration’. 3 to 5 mg/Kg used for initial induction, action only lasts 5-10 minutes or so as redistribution sends more agent to muscle mass. Thiopental causes a cerebral oxygen demand, myocardial function, and possibly vascular tone leading to hypo-tension. May be associated with airway reactiveness and therefore is not used with asthmatics etc. Has been used by shadowy Eastern European secret agents to get secrets etc. out of low level secretaries in Brussels. (Truth serum). |
|
|
|
Diazepam (Valium)
|
Widely used tranquilizer used primarily for pre-anesthetic sedation.
Is a mild muscle relaxant and anti-convulsant. Metabolized by the liver and excreted by the kidney (70%) & bile/feces (30%). Prolonged effect due to metabolites having nearly as strong an effect as the original drug. Causes pain at peripheral injection site. Better to infuse in a central line. |
|
|
|
Midazolam (Versed)
|
Stronger cousin of diazepam. (2 to 3 times)
0.1 to 0.3 mg/Kg dose. Has the same pharmacological action plus is an anterograde amnesiac. Pts may seem awake during procedure but have little or no memory of the event afterwards. Useful in cardio-versions, intubation, bronchoscopy etc. No pain at injection site. Duration of action is 15 minutes---longer than thiopental but less than valium. Metabolized by liver---excreted by kidneys Little effect on BP, RR, cerebral blood flow, ICP |
|
|
|
Etomidate
|
Loading dose: 0.2 to 0.3 mg/kg
Short duration of action: 3 to 8 minutes No analgesia, minimal cardio vascular effects. Some adrenal suppression, which may be advantageous in some pts.). Potent cerebral vasoconstrictor. Possible alternative to Propofol or thiopental |
|
|
|
MAC?
|
Definition: Minimum Alveolar Concentration. “The minimum concentration of an agent needed to prevent movement in 50% of patients when a standard incision is made”.
This obviously infers that 50% will move. If we increase a MAC by 30 %, 95% of patients will not move during a painful incision. MAC is the standard measure of an agents’ strength. The lower the MAC, the stronger the agent. |
|
|
|
MACs of Inhaled Anesthetics
|
Methoxyflurane 0.16%
Halothane 0.77% Isoflurane 1.15% Enflurane 1.70% Sevoflurane 2.00% Desflurane 6.00% Nitrous Oxide 104.00% |
|
|
|
Increases MAC
|
Hyperthermia
Drug use Chronic alcohol abuse Amphetamines CNS stimulants |
|
|
|
Decreases MAC
|
Advanced age
Hypothermia Severe hypotension Other agents; opiates,valium Acute drug or ETOH intox. Pregnancy Hypothyroidism High PCO2, Low PO2 |
|
|
|
Nitrous Oxide facts
|
Nitrous Oxide is 34x more soluble than nitrogen gas.
Second gas effect Diffusion hypoxia during emergence. Closed air spaces may double in 66% N2O |
|
|
|
|
|
|
|
Soluability of halogenated hydrocarbons
|
High: Halothane
Enflurane Isoflurane Sevoflurane Desflurane Low: Nitrous Oxide (HE IS Dumb N2O?) |
|
|
|
the enzyme _____ takes out most anesthetic agent
|
P450 cytochrome
|
|
|
|
Rocuronium reversed by
|
Neostygmine
|
|

