![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
141 Cards in this Set
- Front
- Back
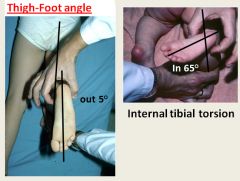
Used to determine whether a child has feet that are abnormally inverted.
|
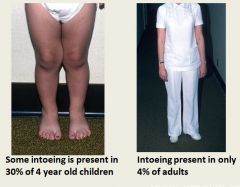
Intoeing is a common finding in children. Most often they grow out of it.
|
|
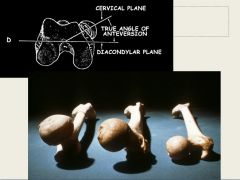
Normal is on the right; others have abnormal femoral angles - can be a cause of excess femoral torsion leading to intoeing.
|
|
|
|
What kind of sports are tibial and femoral torsion good for?
|
Tibial = sprinting
Femoral = swimming |
|
|
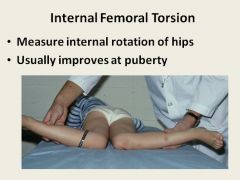
Increased Femoral Anteversion (Rotation):
|
Infants have a degree of torsion up to 40 degrees, which gradually reduces with growth - adult femurs have an angle of about 15 degrees.
In some children, the change is slow or incomplete leading to a relative increase in internal femoral rotation. The clinical manifestation is intoeing during walking and rotation of the entire femur (observed via the medial position of the patella). Usually, rotation gradually decreases, with improvement in intoeing, until 9 years of age. Persistant intoeing after this age means intoeing in the adult is more likely. This disorder requires no treatment except reassurance of the parents. |
|
|
What is the only circumstance in which surgery is used to fix intoeing?
|
Surgery to untwist the bones is only done in extreme cases after the age of 6 years.
|
|
|

|
|
|
Pes Planus (flatfoot):
|
Flat foot refers to the loss of the normal longitudinal arch of the medial foot. Many cases are inherited. The foot is usually flexible, so the arch appears when the foot is not bearing weight. Hindfoot eversion is often present.
Examination from behind should show a normal arch and varus heel when the patient stands on tiptoe. If these signs of a flexible flatfoot are not present, tarsal coalition should be considered. Will not go away with age. Should be helped with corrective shoes, arch supports and shoe inserts. |
|
|
|
|
|
|
|

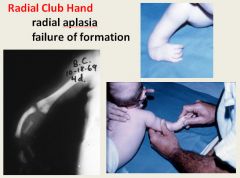
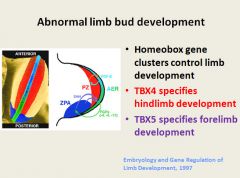
TBX5 controls the heart as well; that is why it’s called hand-heart syndrome.
|

|
|
|
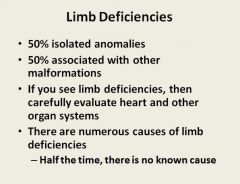
Amniotic Bands:
|
During gestation, protein-laden amniotic material can condense around limb segments. These amniotic bands may indent delicate embryonic tissues, causing constriction rings or even necrosis and resorption of the distal segment (congenital amputation).
|
|

|

Most common lower limb deficiency.
Though to be caused by an abnormality in vasculature during development or a placental emboli. |
|

Different parts of the skeleton grow at different rates.
|

|
|

|

From left to right: 2 years old (carpal bones grow in at about 1 per year), 10 years old, adult
|
|
|

Achondroplasia: Failure of cartilage formation = failure of bones to grow; doesn’t effect the spine, just the limbs
|
|
|
Achondroplasia:
|
The major cause of dwarfism.
The cause in a point mutation in the FGFR3 that results in its continuous activation. The production of FGFR3 suppresses chondrocyte proliferation; as a result, the normal epiphyseal growth plate expansion is suppressed and long bone growth is severely stunted. Typically an autosomal dominant disorder; four out of five cases represent new spontaneous mutations. The most obvious changes are shortening of the proximal extremities, bowing of the legs and a lordotic posture. |
|

|

|
|

|

|
|
|
Osteogenesis Imperfecta:
|
Caused by defective type I collagen sythesis (alpha1 and 2 chains).
The fundamental abnormality in OI is too little bone, resulting in extreme skeletal fragility. There are four major subtypes; type II is fatal in utero or immediately post-partum due to multiple fractures. Type I patients may have normal lifespans. Classic findings are blue sclera, hearing loss and small misshapen teeth. |
|
|
Osteopetrosis:
|
Characterized by reduced osteoclast-mediated bone resorption and defective bone remodelling.
The bone is grossly dense and stone like, but architecturally unsound and fractures easily. Bone resorption by osteoclasts depends on acidification of lysosomes by proton pumps. One variant of OP is associated with carbonic anhydrase II deficiency - lack of acidification in the lysosomes. The nature of pathogenesis in other variants is unknown. Besides fracture, patients frequently have cranial nerve problems due to compression of surrounding bone, and infections due to reduced marrow space. Hepatosplenomegaly is common due to increased extramedullary hematopoiesis. |
|
|
Where do bipeds have thier center of gravity?
|
In front of the second part of the sacrum.
|
|

|

|
|

|

|
|
|
What is the most common reason for toddlers' to not walk or bear weight?
|
Trauma: commonest fractures are 1st metatarsal, tibial shaft (spiral, known as a ‘toddler ‘fracture.) Toddlers will weight bear with a metatarsal fracture but not with a tibia fracture until it starts to heal (about a week)
* |
|

|

|
|

|

|
|

|

|
|
|
Cerebral Palsy:
|
A static encephalopathy in a growing child. Although it is often birth related, the term also includes childhood head injury, stroke, metabolic brain conditions and degenerative neurological conditions.
The hallmark of most cases of CP is alteration in motor tone (spasticity or dystonia). Diagnosis of spasticity can be direct (increased tone, increased tendon reflexes and clonus) or inferred (shortening of muscles, contractures of joints, scoliosis). |
|
|
What neurological disorder is an increasing cause of limping in children/toddlers
|
Cerebral palsy
|
|

|

|
|
|
Developmental Dysplasia of the Hip:
|
The neonatal hip is an unstable joint because the muscle is underdeveloped, the cartilage is soft and easily deformed and the ligaments are lax.
Positioning in utero and breech birth causes excess stretching of the posterior hip capsule, which renders the joint unstable after delivery. Because normal joint motion is needed for proper development, the hip joint may become dysplastic if not repaired. |
|
|
|
|

|

|
|
|
Slipped Capital Femoral Epiphysis:
|
An adolescent disorder characterized by displacement of the femoral head on the femoral neck.
Affects males and females 11-13 years of age. The typical patient is overweight and is in puberty. This disorder occurs when the cartilage is thickening under the influence of growth hormone, but the secretion of sex hormone that stabilizes the growth plate is absent. Lack of sexual maturity and mechanical stress combine to render the plate susceptible to slippage. |
|

|

|
|

|

Slipped capital femoral epiphysis
|
|

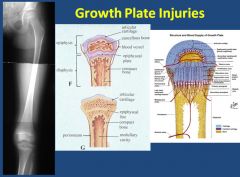
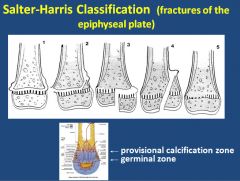
Types 4 and 5 are the worst; there is a possibility that the growth plate will be arrested.
|

X-ray of the growth plate on the back of the calcaneus; damage can lead to Sever's disease
|
|
|
Sever's Disease (calcaneal apophysitis):
|
Heel pain, unlike the heel spurs that occur in adults, is very uncommon in children. Of those children who do get heel pain, by far the most common cause is a disturbance to the growing area at the back of the heel bone (calcaneus) where the strong achilles tendon attaches to it. This is known as Sever's disease or calcaneal apophysitis (inflammation of the growth plate). It is most common between the ages of 10 to 14 years of age.
Pain is usually felt at the back and side of the heel bone. Sometimes there may be pain at the bottom of the heel. The pain is usually relieved when the child is not active and becomes painful with sport. Squeezing the sides of the heel bone is often painful. Running and jumping make the symptoms worse. One or both heels can be affected. In more severe cases, the child may be limping. |
|
|
Osgood-Schlatter disease:
|
In preadolescent children, the anterior tibial tubercle can be fragmented by chronic tensile stress from the muscle attachment (apophysitis). As the tibial tubercle becomes more prominant due to damage, a painful bursa can form over it.
Symptoms vary from mild aching at the tubercle to severe pain with patellar function and exaggerated bursal tenderness. |
|

A normal meniscus is C shaped. Discoid meniscus are abnormally shaped and thickened; can lead to the problems listed on the slide.
|

|
|

X-ray of child with Osgood-Schlotters disease; fracture of the tibial tubercle. Caused by tightness and shortening of the quadriceps.
|

X-ray of an Osteochondritis Dissicans lesion.
|
|
|
Osteochondritis Dissecans:
|
A disorder of the distal femoral condyle ossification center. A portion of the joint softens, shears or separates through the articular cartilage and underlying bone. Common in children 8-14 years of age.
The disease is caused by a combination of injury from activity and femoral condyle fragility resulting from immature ossification of the femoral condyle. |
|
|
What is "Little league elbow"?
|
Medial epicondyle epiphysitis
|
|

|
Was born breech; her hip was dislocated
|
|

The hip pops back in when the leg is abducted and you can feel it. This checks for DDH. It does not hurt the baby.
|

This test check for a dislocatable hip. As the leg moves, the hip pops out of the socket.
|
|

|
Was discovered during a sports physical
|
|

|

|
|

|

|
|

|
Requires cast treatment; serial casting followed by heel cord cut at 6 weeks of age. Treatment is 90% sucessful by 9 weeks of age.
|
|
|
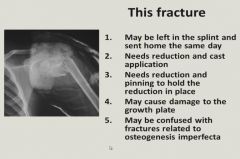
May be left in the splint and sent home the same day; in young children, the periosteum of rapidly growing areas can remodel and heal fractures quickly.
|
|

|
May be confused with fractures related to osteogenesis imperfecta; multiple healing fractures are present - although the bone density looks good on this child...the actual cause is child abuse.
|
|
|
Child Abuse:
|

|
|
|
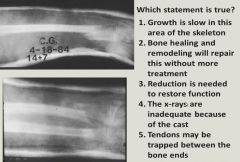
Bone healing and remodeling will repair this without further treatment.
|
|

Occurs in a rapidly growing area that does not include the epiphyseal growth plate.
|

This type of fracture can only occur in children. Wrist still works.
|
|

Distal radius fractures are increasing due to these factors.
|

|
|

|
X-rays of hips; this child is an overweight adolescent and he has a slipped capital femoral epiphysis.
The referred knee pain is due to the small branch of the obturator nerve that goes to the knee splitting off and going to thier hip. Any child who complains of knee pain should have thier hips examined. |
|

Then do a neurovascular exam and x-ray; check sensation motor function and pulses and check the skin.
|
|
|
|

|
|

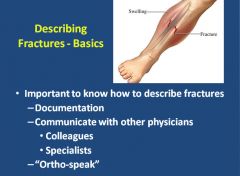
Any laceration around the area of a fracture is treated as open and sent to the ER.
|

|
|

|

|
|

|
|
|
|

|
|

Intrinsic bone quality; a pathological bone fracture means there is something wrong with the bone itself and broke doing something normal (can be caused by cancer)
|

|
|

|
|
|
|

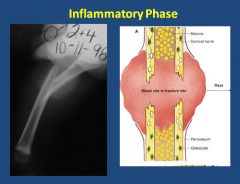
How do fractures heal? Primary and secondary. Secondary is the most common type: is where you heal with a substance called callus – heals this way when there is some motion allowed in the break. Common way to heal in casts.
Smoking can prolong fracture healing time. |
|
|

Early soft callus but no bleeding, doesn’t hurt as much any more.
|
|

|

|
|
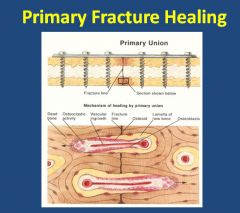
Primary fracture healing; much slower. Happens when the fracture is compressed and plated together and not allowed movement. Bone is gradually remodelled by osteoclasts instead of callus.
|

|
|

|
|
|

|

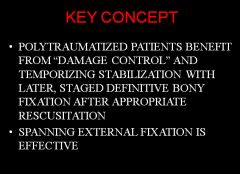
When the pelvis splits it stretches/breaks major vessels and you can get major life threatening internal bleeding
|
|

|

Think about soft tissue injuries when fractures happen; more likely to occur the more traumatic the accident was.
|
|

This is a comminuted intra-articular fracture of the distal femur.
|

|
|

|

|
|

|

|
|

This is what "nailing" a femur is; the insertion of a rod into the marrow cavity of the femur in order to stabilize a fracture.
|

|
|

|

|
|
|
What is the most common primary malignant bone tumor?
|
Osteosarcoma
|
|
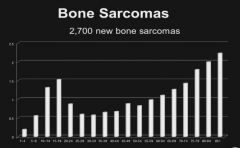
Osteosarcoma and Ewing's Sarcoma are the tumors that occur most in childhood.
|
|
|

The most common soft tissue sarcoma is pleomorphic high grade undifferentiated sarcoma.
The most common in children is rhabdomyosarcoma in the head, neck and retroperitoneum. |

Ossification looks like "cumulus cloud like"
Calcification looks like "arcs and rings" Fibrous looks like "ground glass”, and the histology has a herringbone pattern. |
|
|
Osteoma:
|
Osteomas are benign lesions of bone that are commonly found in the head and neck and occur in middle age.
They are usually solitary and present as localized, slowly growing, hard masses on the bone surface. They may cause local mechanical problems or cosmetic deformaties, but do not undergo malignant transformation. |
|
|
Osteoid osteoma and osteoblastoma:
|
Are benign neoplasms with similar features. Both arise during the teenage years most often in males.
Osteoid osteomas arise most often in the proximal femur and tibia are are less than 2 cm - whereas osteoblastomas are much larger. Localized pain is common with osteoid osteomas and is relieved by aspirin. Osteoblastomas arise most often in the vertebral column; they also cause pain - not relieved by aspirin. Grossly, both lesions are round or oval masses with a rim of sclerotic bone (more conspicuous in osteoid osteomas). |
|

|

Interlacing trabecula of woven bone surrounded by osteoblasts. The intervening stroma is loose, vascular connective tissue containing variable numbers of giant cells.
|
|
|
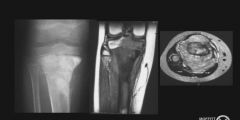
Osteosarcoma:
|
A bone producing malignant mesenchymal tumor. The most common primary malignant tumor of bone. 75% of cases are in patients younger than 20. Most arise in the metaphyseal region of the long bones of the extremeties.
Heriditary - RB gene mutations Sporadic - p53 mutations Typically present as painful enlarging masses. The tumor frequently breaks through the cortex and lifts the periosteum creating a "Codman triangle". Osteosarcomas spread hematogenously and frequently metastasizes to the lungs. |
|

Gritty gray white tumors that frequently produce soft tissue masses.
|

Cells vary in size and shape and have large hyperchromatic nuclei; bizarre giant cells and mitoses are common.
|
|
|
Enchondroma:
|
Chondromas are benign tumors of hyaline cartilage. When they arise within the medulla they are called enchondromas; when on the surface they are called juxtacortical chondromas.
Most endochondromas are detected as incidental findings. The calcified matrix looks like loops and rings. Most are benign and stable, and can recur if incompletely excised. |
|

|

|
|
|
Chondrosarcoma:
|
Malignant tumors of cartilage that commonly arise in the pelvis, shoulder and ribs; they rarely involve the distal extremities. They typically present as painful, progressively enlarging masses.
Chondrosarcomas metastasize hematogenously to the lungs and skeleton |
|

|

Somtimes two nuclei can be seen in 1 lacuna - this is indicative of chondrosarcoma
|
|
|
Fibrous Dysplasia:
|
A benign tumor that can involve single or multiple bones. However, fibrous dysplasia can cause marked enlargement and distortion of bone, so that if the face or skull is involved, disfigurement can occur.
Individuals with monostotic disease usually have minimal symptoms. By x-ray, lesions exhibit a ground glass appearance with well defined margins. Polyostotic disease is more progressive and has more severe skeletal complications, fractures, long bone deformities and craniofacial distortion. |
|

Note the "shepherds crook" deformity.
|

Note herringbone pattern with fibrous tissue.
|
|

Note the "bear bite" lesion
|

|
|
|
Giant Cell tumors:
|
Giant cell tumors are dominated by multinucleated osteoclast type giant cells. It is benign but locally aggressive.
The majority arise in the epiphysis of long bones around the knee, frequently causing arthritis-like symptoms. |
|
|
Fibrous Cortical Defect:
|
Fibrous cortical defects occur in 30-50% of all children older than 2; they are developmental defects rather than true neoplasms.
The majority are small and arise in the metaphysis of the distal femur or proximal tibia; almost 50% are bilateral or multiple. They are asymptomatic and most undergo spontaneous differentiation into normal cortical bone within a few years. Histology shows a characteristic "pinwheel" pattern. |
|
|

|
|
|

|
|

|

The technicium goes into osteoblasts. Detects areas of high turnover.
|
|

|
Note that the CT scan of the bone shows a calfication mass; enchodroma
|
|
|
Ewing's Sarcoma:
|
Malignant small round-cell tumors of bone and soft tissue. After osteosarcomas they are the second most common pediatric bone sarcoma.
The common chromosomal abnormality is fusion of the EWS gene on 22 with either FL1 on 11 or ERG on 21. The resulting protein acts as a transcription factor to stimulate cell proliferation. Typically present as painful enlarging masses in the diaphyses of long tubular bones and the pelvic flat bones. Some patients have systemic symptoms (fever, ESR, anemia and leukocytosis). There is a characteristic periostial reaction seen on x-ray as "onion skinning". |
|
What bone tumor is this?
|
Osteosarcoma
|
|

What bone tumor is this?
|
A benign Fibrous cortical defect
|
|

What kind of tumor is this?
|
A benign osteoid osteoma.
|
|

What kind of tumor is this?
|
Benign Fibrous dysplasia; always shows up very hot on a bone scan.
|
|

What kind of tumor is this?
|
Ewings sarcoma
|
|

What kind of tumor is this?
|
Osteosarcoma; note the moth eaten appearance of the bone
|
|
|
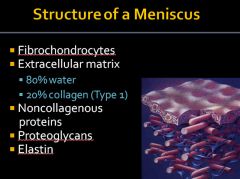
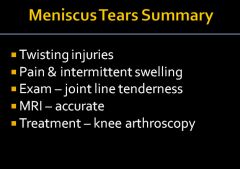
This type of knee injury causes the following symptoms/physical exam findings:
Intermittent knee swelling Pain with running Pain with squatting Full knee ROM Mild effusion Medial joint line tenderness Stable ligament exam |

|
|
|
|
|

|

|
|
|
What knee injury causes the following symptoms/physical exam findings?
Immediately after injury: Loud “pop” Pain & abundant swelling Difficulty walking Physical exam a few days later: Large effusion ROM 0-90 degrees Diffuse pain to palpation Positive Lachman test |

The Lachman test is the anterior drawer test with the knee flexed at 20-30 degrees.
|
|

|

|
|

|
|
|

|

|
|

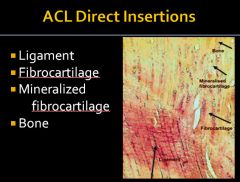
Tendons used as replacements are the middle third of the patellar tendon or a tendon from the hamstrings.
|

|
|
|

|
|

|

The anterior talofibular ligament is the most commonly injured.
|
|

Medial ankle sprains are less common because the ligament bands are so thick
|

Injury to these ligaments results in a “High” ankle sprain
|
|

When you see the dimple that means the talus is moving anteriorly.
Means the anterior talofibular ligament is sprained. |

Checks the ligament that run between the tibia and fibula. These ligament help hold the ankle together
|
|

Generally, if you hurt over bone – you might have a fracture
|

|
|
|

|
|

|

|
|

|
|
|
|

|
|

|

Neer and Hawkins tests are provocative tests that evaluate for impingement.
|
|

|

|
|
|
|
|

|

|
|

|

|
|

|

|
|

The lateral epicondyle is on the thumb side of the arm.
|

|
|

|

|
|
|
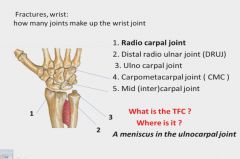
Distal radius and ulna fracture:
|
Colles fracture: A radius break at the distal metaphysis resulting in volar angulation of the hand.
Smith's fracture: A radius break at the distal metaphysis that results in dorsal angulation of the hand. Distal radial fractures are separated into three groups: extraarticular (A), partial articular (B) and complete articular (C) |
|
|
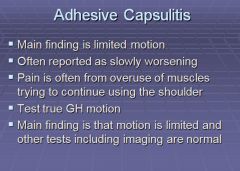
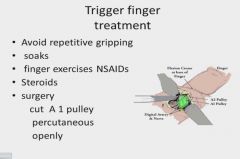
Trigger finger:
|
Also called flexor tenosynovitis; characterized by pain and tenderness in the palm. Patients frequently notice catching or triggering of the finger after forceful flexion.
|
|
|
Carpal Tunnel:
|
Compression of the median nerve within the carpal tunnel; patients complain of numbness in thumb and index and middle fingers. Pain may awaken the patient after a few hours of sleep.
Tinel sign: Elicited by percussing the skin over the median nerve; the patient complais of an electric or tingling sensation. Phalen maneuver: Patient flexes wrists while holding elbows in extension; onset of symptoms within 60 seconds = carpal tunnel syndrome |
|
|
Dupuytren Disease:
|
Characterized by a nodular thickening on the palmar surface of the hand affecting the palmar fascia. Flexion contractures occur at the MP joints; the little and ring fingers are the most involved.
Dupeytren disease is associated with family history, seizure medications, alcoholism, smoking and diabetes. (The little and ring fingers are contracted up against the palm) |
|

|

|
|
|

|
|

The scaphoid is supplied by a branch of the radial artery; the radial artery supplies the palm and the dorsum of the hand is where veins are located.
|

|
|

|

|
|

|

|
|

|

|
|
|

Dequervaines = extensor tendon swelling
|
|

|

|

