![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
Who first described and used myofascial release?
|
A.T. Still.
|
|
|
What is MFR?
|
Myofascial release is a system of dx and tx which engages continual palpatory feedback to achieve release of myofascial tissues.
|
|
|
What are the subcategories of MFR?
|
Balanced ligamentous tension (BLT), ligamentous articular strain (LAS), integrated neuromusculoskeletal release (INR), fascial unwinding.
|
|
|
What is the basic concept of MFR?
|
Contact of the myofascial structures is made, tissues are returned to normal position and function to promote a positive change in a patient’s body. Improved: circulation of fluids- arterial, venous, lymphatic; neurologic function; ability of the person to heal himself/herself
|
|
|
What does MFR require?
|
Palpatory skills, dx ability, application of basic OMT principles.
|
|
|
What is fascia?
|
Band of fibrous tissue such as lies deep to the skin or forms an investment for muscles and various organs of the body.
|
|
|
What germ layer does fascia arise from?
|
Mesoderm
|
|
|
What are the functions of fascia?
|
Packaging, protection, posture, passageways, homeostasis.
|
|
|
List properties of fascia.
|
Elasticity, plasticity, viscosity, strain, stress, relaxation, creep, piezoelectricity, contractility, Newton's 3rd law, Wolf's law.
|
|
|
Describe a typical stress-strain curve for connective tissue.
|
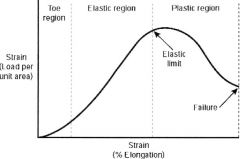
Toe region represents the region where little stress is required to lengthen the tissue; it probably represents straightening of wavy pattern of collagen fibers. Elastic region is that portion of the curve in which tissue returns to its original length when the stress is removed. Plastic region is that portion of the curve that results in permanent elongation when the stress is removed.
|
|
|
What is creep?
|

Tissue undergoes gradual elongation over time when subjected to constant stress.
|
|
|
What is the piezoelectricity?
|
Electric current generated in some materials in response to mechanical strain.
|
|
|
What is the piezoelectric phenomenon?
|

Mechanical stress produces piezoelectric effect in bones which leads to bone remodeling. The concave side {of a bone} (or side under compression) becomes electronegative. Electro-negativity signals osteoblasts to lay down bone on the concave side.
|
|
|
How does fascia have contractility?
|
Fibroblasts, chrondoblasts, osteobalsts have innate capacity to express the gene for alpha-smooth muscle actin. Human fibroblasts respond to acyclic strain by altering cell shape and alignment, undergoing hyperplasia… The increased secretion of IL-6 and nitric oxide may provide insight into the pathophysiology of fibrosis and tissue texture changes seen with injury and OMT.
|
|
|
What was the result of the experiment with human fibroblast under repetitive motion strain, with subsequent direct OMT?
|
The modeled injury (RMS) appropriately displayed enhanced apoptosis activity (consistent with pro-apoptotic BadS91 and DAPK2 signaling) and loss of intercellular integrity. Added DOMT to this group resulted in normalization in apoptotic rate and enhanced proliferative capacity, albeit in a BadS91 and DAPK2-independent fashion.
|
|
|
List and describe fascial mechanorecptors.
|
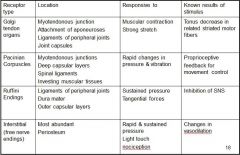
|
|
|
What mechanoreceptors does the physician use in his body in OMT treatment and what do they do?
|
Pacinian corpuscles (acceleration receptors) - uses to identify end range of motion of the patient's joints, to differentiate the restrictive barrier. Ruffini's endings (dermal stretch receptors) - use to determine skin drag. Interstitial [free nerve endings] (for light touch, temperature, nociception) - uses to identify temperature and tissue texture changes.
|
|
|
How does the patient use mechanoreceptors in treatment?
|
Pacinian corpuscles - sense of acceleration or deceleration causes change in muscle tension in response to differing forces being applied. Ruffini's endings - use to determine physiologic barrier and end range of motion. Intersitial - uses to identify nociceptive signals.
|
|
|
Describe tightness.
|
Restrictive barrier found, tethering (acute muscle spasm), bind, restriction of motion.
|
|
|
Describe looseness.
|
Ease of motion, neural inhibition (muscle weakness), pain, hypermobility.
|
|
|
What is indirect MFR?
|
Stack all myofascial tissues in the directions of ease.
|
|
|
What is direct MFR?
|
Stack all myofascial tissues in the directions of restriction.
|
|
|
List the palpable layers.
|
Skin, adipose tissue, superficial fascia, muscles, tendons/ligaments, deep fascia, bone.
|
|
|
What motion does the body undergo in inhalation?
|
Spinal curves flatten (decrease), extremities tend toward external rotation.
|
|
|
What motion does the body undergo in exhalation?
|
Spinal curves accentuated (increase), extremities tend toward internal rotation.
|
|
|
What is respiratory cooperation?
|
A physician directed inhalation and/or exhalation by the patient to assist the manipulative process.
|
|
|
List indications for MFR?
|
Acute painful situations, hospitalized pts, chronic disease states, peds pt, geriatric pts, anytime you wish to use OMT.
|
|
|
List contraindications for MFR?
|
Fractures, physicians inability, inability to position pt, inability of pt to respond to tx.
|
|
|
What are the steps of MFR technique?
|

|
|
|
In performing direct MFR, what should you note about the tension?
|
There should be increased tension under your hands and less distally.
|
|
|
In performing indirect MFR, what should you note about the tension?
|
There should be decreased tension under your hands and more distally.
|
|
|
How is diagnosis made for MFR?
|
Visual inspeciton, TTA assessment, assess somatic dysfunction of area.
|
|
|
What are the indications for MFR on the knee?
|
Knee pain, ankle somatic dysfunction, late post-operative, patellofemoral syndrome, postural imbalance, knee swelling, etc.
|
|
|
Describe the MFR technique for the knee.
|
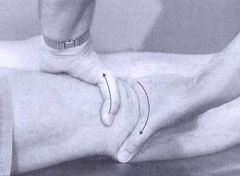
Patient supine. Stand beside affected knee. Place cephalad hand on the distal thigh, superior to the patella. Place caudad hand on the proximal tibia, inferior to the patella. Make firm and full contact with hands. Palpate for fascial layers. Evaluate rotatory motion – internal/external rotation of tibia/femur. Maintain rotatory tension. Evaluate abduction/adduction motion (induce valgus/varus). Hold the tissues at the restrictive barrier. Evaluate compression and traction. Hold in the position of tightness (restrictive barrier). Ask patient to breath in an out. Notice which breath cycle tightens the tissues (respiratory cooperation). Then ask patient to hold breath in the cycle which tightened the barrier further, until air hunger. Hold the tissues firmly in all planes until release is appreciated. Release and retest the TTA and motion in the knee joint looking for improvement in range and quality.
|
|
|
What are the indications for MFR on the ankle?
|
Ankle or foot pain, grade 1 ankle sprain (grades 2-3 when cleared orthopedically), plantar fasciitis, postural imbalance, etc.
|
|
|
Describe the MFR technique for the ankle.
|

The patient is supine. Stand at side of affected ankle . Place cephalad hand so that thumb is around the distal tibia and on lateral ankle ligaments, fingers grasping tibia. Place caudad hand so that web of thumb and fingers is on the hind foot (just distal to other hand). Palpate for fascial layer(s). Evaluate rotatory motion. Next evaluate inversion/ eversion motion . Next evaluate compression and distraction. Ask patient to breath in an out. Notice which breath cycle increases the ease in the tissues. Then ask patient to hold breath in the cycle which loosened the tissues further, until air hunger. Hold the tissues firmly in all planes until release is appreciated. Release and retest the TTA and motion in the ankle joint looking for improvement in range and quality.
|
|
|
What are the indications for MFR on the scapulothoracic joint?
|
Shoulder restrictions in motion, pain, cervical pain, postural imbalances, thoracic outlet syndrome, etc.
|
|
|
Describe the MFR technique for the scapulothoracic.
|
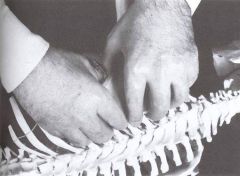
Partner is prone with arm hanging over table (or lateral recumbent). Stand on the side of the affected shoulder. Using caudad hand, place the thumbs on the lateral border and fingers along the medial border of the scapula, so angle of scapula is in palm. With cephalad hand, place fingers at medial border and thumb at lateral border. Motion test in the following 3 planes, assessing for ease and restriction: superior/inferior (red); lateral/medial (blue); clockwise/counterclockwise (yellow). Ask patient to breath in an out. Ask patient to hold breath in the cycle which tightened the barrier further, until air hunger, for direct technique. Hold tissues until release is palpated and patient takes a breath. Release tissues and reassess.
|
|
|
What are the indications for MFR on the wirst, forearm, and elbow?
|
Forearm/wrist/elbow pain, lateral and epicondylitis, carpal tunnely syndrome, etc.
|
|
|
Describe the MFR technique for the wirst, forearm, and elbow.
|
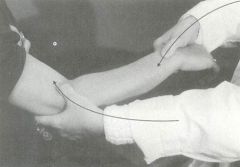
Partner is standing, seated, or supine. Grasp the thenar eminence with four fingers. The index and long fingers contact the area of the transverse carpal ligament. The grasping thumb contacts the extensor surface of the hand and wrist pointing proximally along the long axis of the forearm. The other hand grasps the patient’s forearm at the elbow (radial head). Palpate superficial and deep myofascial structures to determine which layer to work in. Next turn the wrist in pronation and supination until a restrictive (tight) barrier is noted at either side of the elbow or within the mechanics of the wrist and hand (Diagnosis= pronation or supination). Assess fascial motion of the wrist (Diagnosis= flexion/extension/abduction/adduction). Add compression or traction, whichever tightens the barrier (Diagnosis= compression or traction). Ask patient to breath in an out. Notice which breath cycle tightens the tissues. Then ask patient to hold breath in the cycle which tightened the barrier further, until air hunger. Hold the tissues firmly for a few seconds until release is appreciated. Release and retest the motion of the forearm looking for improvement in range and quality.
|

