![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
217 Cards in this Set
- Front
- Back
|
How much saliva is produced per day?
|
1.5 L
|
|
|
How much water is contained in the average day's food?
|
2 L
|
|
|
How much liquid does stomach secrete each day?
|
2 L
|
|
|
How much liquid does the pancreas secrete per day?
|
1.5 L
|
|
|
How much bile is secreted per day?
|
0.5 L
|
|
|
How much liquid does the small intestine secrete per day?
|
1 L
|
|
|
How much liquid is reabsorbed by the small intestine each day?
|
6.5 L
|
|
|
How much liquid is reabsorbed in the colon?
|
1.9 L
|
|
|
How much liquid enters or is secreted into the GIT each day (including food)?
How much of this remains in the faeces? |
8.5 L are ingested or secreted.
Of this, only 0.1 L remains in the faeces. |
|
|
What are the three basic types of GI secretion?
|
NaCl + water
NaCO3 + water HCl + water |
|
|
Which parts of the GIT secrete NaCl + water? (3)
|
Salivary glands
Pancreatic acinar cells Intestinal crypts (small and large intestine) |
|
|
Which parts of the GIT secrete NaCO3? (4)
|
Pancreatic ducts
Bile ducts Gastric surface mucosa Duodenal mucosa |
|
|
What is responsible for the overwhelming majority of water and electrolyte absorption in the gut?
What does it absorb exactly? |
The villous cell in the small and large intestine absorbs NaCl and water.
|
|
|
What is the basic mechanism by which GI epithelia secrete NaCl?
|
Na+/K+ ATPase generates a sodium gradient into the cell.
Na+K+Cl-2 triple transporter uses this gradient to move Cl- into the cell. This Cl- gradient flows through chloride channels into the lumen and pulls sodium with it via the paracellular route. |
|
|
T/F: Tight junctions can prevent the movement of cations
|
False
|
|
|
Why doesn't the concentration of K+ in the GI epithelium (due to the combined action of Na+/K+ ATPase and the NaK2Cl triple transporter) interfere with the electrochemical gradient into the cell?
|
Because K+ is free to diffuse back out of the cell through K+ channels.
|
|
|
How is saliva secretion regulated?
|
Muscarinic innervation via M1 receptors causes a rise in Ca++ levels, which in turn causes calcium-dependent chloride channels to open.
|
|
|
In which epithelia is [Ca++] responsible for the regulation of NaCl secretion?
|
Salivary glands
Pancreatic acinar cells |
|
|
What causes the obstructive GI symptoms seen in cystic fibrosis?
Where in the GI tract does this problem arise? |
NaCl can't be secreted (along with water) by the crypt cells of the small and large intestine because CFTR is the Cl- channel.
This causes obstruction due to the chyme being less hydrated. |
|
|
How does cholera toxin cause increased fluid secretion in the gut?
|
Cholera toxin binds irreversibly to a stimulatory G protein which causes constitutive cAMP production.
This leads to CFTR phosphorylation (activation) by PKA, leading to increased Cl- and hence fluid secretion. |
|
|
How does cholera toxin cause diarrhea? (2)
|
Increased secretion of fluid and electrolytes
Decreased absorption of the same. |
|
|
How does cholera toxin impair the absorptive ability of the gut epithelium?
|
Cholera toxin cause constitutive cAMP production.
cAMP prevents differentiation of secretory crypt cells into absorptive cells. |
|
|
Why does cholera last 5-7 days?
|
Because cholera toxin binds irreversibly to its cellular targets and it takes 5-7 days for new cells to be produced.
|
|
|
What causes fat malaborption in cystic fibrosis patients whose pancreas is still intact?
|
Lipase, even if produced in sufficient quantities, is destroyed because not enough neutralising bicarbonate can be secreted.
|
|
|
T/F: Supraphysiologic doses of lipase is enough to solve the fat malabsorption problem caused by cystic fibrosis
|
False - lipase will still be destroyed in the duodenum due to impaired bicarbonate secretion.
|
|
|
Why might you give misoprostol to someone with CF?
|
To treat malabsorption - this prostaglandin E2 analogue will suppress gastric acid secretion, leading to less destruction of lipase in the duodenum.
|
|
|
How does the secretion of HCl from parietal cells differ from the secretion of NaCl from other epithelia?
|
Instead of Na+ being pulled by chloride through tight junctions, K+ exits via channels and is then exchanged for H+ using the H+/K+ exchanger.
|
|
|
What is the tubulovesicular system?
What is its physiological importance? |
A structural system which allows parietal cell acid secretion to be dramatically increased in a short time (without the need for enzyme or pump induction).
Preexisting H+/K+ ATPase pumps line 'tubulovesicles' within the cell. Upon activation, these fuse with the apical membrane, instantly expanding the secretory activity of the cell. |
|
|
How is NaCl absorbed "electroneutrally" throughout the gut? (describe apical and basolateral membrane mechanisms)
|
Apical membrane:
Na+ is swapped for H+ (Na+/H+ exchanger) Cl- is swapped for HCO3- (Cl-/HCO3- exchanger. Basolateral: Na+ is then transported via Na+/K+ ATPase Cl- is cotransported with K+. |
|
|
What transporter defect can cause sodium-rich diarrhea?
|
A defect in the Na+/H+ exchanger.
|
|
|
What transporter defect can cause chloride-rich diarrhea?
|
A defect in the Cl-/HCO3- exchanger
|
|
|
What is SGLT-1?
Is it active or passive? |
A sodium-glucose cotransporter that can absorb glucose or galactose by coupling it a sodium gradient.
It is active. |
|
|
T/F: SGLT-1 is specific for glucose
|
False - it can also transport galactose
|
|
|
T/F: SGLT-1 is ATP-dependent
|
False - it is dependent on a sodium gradient, so is energy-dependent, but does not use ATP directly.
|
|
|
How is fructose absorbed in the gut?
|
By facilitated diffusion through GLUT-5 channels.
|
|
|
T/F: High-dose fructose causes osmotic diarrhea in around 15% of the population because there is no active transporter for it
|
False - 50g or more of fructose causes osmotic diarrhea in up to 60% of the population.
Also, there is probably an active transporter for fructose but this, and the passive carrier GLUT-5, are saturated at low doses. |
|
|
What does GLUT-2 do?
|
It passively transports fructose and glucose across the basolateral membrane.
|
|
|
T/F: Neithr SGLT-1 nor GLUT-5 are inducible
|
False - SGLT-1 is not induced by high glucose in the diet, but GLUT-5 does get upregulated by high fructose diets
|
|
|
What is Hartnup disease?
|
A disease of defective amino acid transport - esp. tryptophan - which leads to deficiency and a range of skin and neurological symptoms.
|
|
|
What does PepT1 do?
Why is it clinically important? |
It transports di- and tripeptides into the gut.
It is clinically important because: - it provides a way around Hartnup disease (amino acid deficiency can be fixed with specific peptide replacement) - it transports certain drugs, such as cephalosporins |
|
|
What is the most common cause of diarrhea in children?
|
Rotavirus
|
|
|
What is the most common cause of diarrhea in adults?
|
Norovirus
|
|
|
Name six bacteria associated with diarrhea.
Are they gram-positive or -negative? |
Campylobacter
Salmonella Shigella Yersinia Vibrio E. coli All are gram negative |
|
|
Name the two most common protozoans to cause diarrhea.
Which* occurs frequently in the child-care setting? |
Giardia lamblia*
Cryptosporidium ss, |
|
|
What is the difference between kwashiorkor and marasmus?
|
Marasmus is malnutrition due primarily to caloric insuffiency.
In kwashiorkor , caloric intake may be sufficient but protein and various micronutrients are deficient. |
|
|
T/F: Microcephaly is only present in severe, long-standing malnutrition
|
True - head circumference is the last growth parameter to be affected by malnutrition
|
|
|
Which type of malnutrition is characterised by oedema?
What is the mechanism? |
Kwashiorkor - protein deficiency causes low plasma albumin
|
|
|
T/F: Marasmus typically causes skin changes such as pigmentation, scaling and peeling
|
False - these are characteristic of kwashiorkor
|
|
|
What nutrient deficiency is follicular hyperkeratosis a sign of?
|
Vitamin A
|
|
|
Name three signs or symptoms of vitamin A deficiency?
|
Night blindness
Xerophthalmia Follicular hyperkeratosis |
|
|
What are Bitot's spots?
|
Deposits of keratin on the conjunctiva due to vitamin A deficiency
|
|
|
T/F: Iron deficiency is the most common nutritional disorder worldwide
|
True
|
|
|
T/F: Iron deficiency causes preterm birth, low birth weight and higher rates of infection.
|
True
|
|
|
Which nutrient deficiency is associated with haemolytic anaemia?
|
Vitamin E
|
|
|
What are the two types of irritable bowel syndrome seen in children?
What is the typical age group for each? What are the presumed mechanisms? How are they treated? |
Diarrhea-predominant IBS:
Presents in children < 3 ? Motility problem Treated by observation and reassurance Pain-predominant IBS: Children > 5 Distension sensitivity of the bowel Treated with fibre, bowel training and buscopan |
|
|
What is buscopan?
What is it used for? How does it work? |
Buscopan (butylscopolamine) is an anti-muscarinic anti-cholinergic.
It is used to treat pain-predominant IBS (and dysmenorrhea) by reducing smooth muscle spasm. |
|
|
Name two hepato-biliary causes of chronic diarrhea
|
Cirrhosis
Extrahepatic biliary atresia |
|
|
What is acrodermatitis enteropathica?
Name 3 symptoms |
Dermatitis (esp. perioral and -anal, acral)
Alopecia |
|
|
T/F: Cow's milk protein intolerance is associated with atopic disease
|
True
|
|
|
T/F: Zollinger-Ellison syndrome typically causes diarrhea
|
True
|
|
|
Name 4 pancreatic causes of chronic diarrhea
|
Cystic fibrosis
Schwachman syndrome (exocrine pancreas hypoplasia) Malnutrition causing pancreatic dysfunction Specific enzyme deficiency |
|
|
T/F: Screening for coeliac disease is recommended for all type 2 diabetics
|
False - it is recommended for type 1
|
|
|
T/F: Osteoporosis is an indication to screen for Crohn's disease
|
False - you should screen for coeliac disease.
|
|
|
Name three syndromes which should raise the index of suspicion for coeliac disease?
|
Down
Turner Williams |
|
|
What serological abnormalities should lead to routine screening for coeliac disease? (2)
|
Unexplained iron deficiency
IgA deficiency |
|
|
What is the standard screening test for coeliac disease?
|
anti-tTG antibody
|
|
|
What are the three weight-based definitions of absolute failure to thrive?
|
Weight < 3rd percentile
Weight for height < 5th percentile Weight > 20% below ideal weight for height |
|
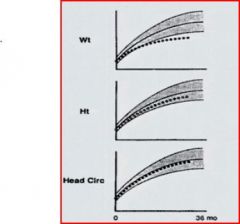
What general problem would cause these growth patterns?
Name three possible causes. |
In general, caloric insufficiency, e.g.:
- inadequate intake - malabsorption - hypermetabolic state |
|

Name three pathological and one non-pathological causes of the growth patterns depicted
|
Pathological:
- endocrine growth failure - stuctural dystrophies - constitutional growth failure Non-pathological: - genetic short stature |
|

Name this growth pattern and two causes of it
|
Absolute symmetrical failure to thrive.
It can be caused by: - intrauterine insults - genetic, esp. chromosomal abnormality (e.g. Down syndrome) |
|
|
Name three causes of excessive renal nutrient loss
|
Nephrotic syndrome
Diabetes mellitus Renal tubular acidosis |
|
|
What pathology is characterised by absent or abnormal peristalsis in the oesophagus and a failure of the lower sphincter to relax?
|
Achalasia
|
|
|
T/F:Food poisoning generally produces less pronounced dehydration and a faster recovery than gastroenteritis.
|
True
|
|
|
T/F: Food-poisoning is not an infectious disease
|
True - food-poisoning occurs due to ingestion of preformed toxins in food. In most cases, the pathogen cannot be cultured from a patient, and the illness cannot be spread from person to person.
|
|
|
What GI disease is characterised by a long incubation period, prolonged fever and a late onset diarrhea
|
Enteric (typhoid) fever
|
|
|
T/F: Enterococci are kinds of streptococci
|
True
|
|
|
Match the following to their food vehicle:
S. aureus C. perfringens B. cereus C. botulinum Rice, preserved vegetables, egg or milk dishes, meat or gravy |
S.aureus - egg or milk
C. perfringens - meat or gravy B. cereus - rice C. botulinum - preserved vegetables |
|
|
How do the enterotoxins produced by S. aureus cause nausea and vomiting?
|
By stimulating the vomiting centre (area postrema)
|
|
|
T/F: Food poisoning caused by B. cereus has an incubation period of 6-8 hours
|
False - it has two incubation periods of 1-6 hours or 8-16 hours, depending on whether growth occurs in the food or in the bowel.
|
|
|
What is the lower limit for acceptable weight gain for a boy at 6 weeks who is on the 3rd centile? the 97th?
(What about girls?) |
3rd centile: 170g/week (145g/week)
97th centile: 130g/week (103g/week) |
|
|
T/F: A child on the 50th percentile for weight will be approximately average
|
False - the 50th percentile reflects the median weight. As paediatrics weights show an upward skew, a child on the 50th percentile will be a bit below average - but right in the middle of their cohort.
|
|
|
What weight percentile is equivalent to 1.85 standard deviations below the mean weight for a given age?
|
The 3rd percentile is 1.85 SDs below the mean (approx)
|
|
|
What three anthropometric indices are recommended for the assessment of under-nutrition in children?
|
Weight-for-age
Height-for-age Weight-for-height |
|
|
What is the definition of 'wasting' in anthropometric terms?
Is the process usually acute or chronic? |
Weight-for-height < 3rd percentile.
The process is usually acute - either severe disease or starvation - because height is normally affected by chronic problems. |
|
|
What is the definition of 'stunted growth'?
|
Height-for-age < 3rd percentile
|
|
|
How does prematurity affect the interpretation of growth charts?
How do you compensate for this? At what age is this compensation no longer useful? |
Premature babies will usually be short and/or wasted if their actual birthdate is used to calculate their age.
To allow for this, their expected birthdate should be used instead. This allowance should be made for weight until 24 months and for height until 40 months. |
|
|
How much weight and length do babies gain per day in the first three months of life (on average)?
|
Weight: 25-30g
Height: 0.9 mm |
|
|
T/F: Failure to thrive can be used to describe a child with just wasting or stunting, or both together.
|
True - FTT can be used to describe all three situations.
|
|
|
What weight percentile is equivalent to 1.85 standard deviations below the mean weight for a given age?
|
The 3rd percentile is 1.85 SDs below the mean (approx)
|
|
|
T/F: A child on the 10th percentile for weight and height cannot be said to be 'failing to thrive'
|
False - if the child has fallen to the 10 percentile from a significantly higher one, this is referred to as relative FTT.
|
|
|
What three anthropometric indices are recommended for the assessment of under-nutrition in children?
|
Weight-for-age
Height-for-age Weight-for-height |
|
|
What is the definition of 'wasting' in anthropometric terms?
Is the process usually acute or chronic? |
Weight-for-height < 3rd percentile.
The process is usually acute - either severe disease or starvation - because height is normally affected by chronic problems. |
|
|
What is the difference between undernutrition and malnutrition?
|
Undernutrition - not enough food
Malnutrition - caloric intake may be sufficient but essential components are deficient, e.g. vitamins |
|
|
What is the definition of 'stunted growth'?
|
Height-for-age < 3rd percentile
|
|
|
T/F: Starvation (energy malnutrition) will generally be accompanied by protein malnutrition, but protein malnutrition does not lead to energy malnutrition.
|
False - protein malnutrition causes a loss of appetite which is often severe enough to cause actual caloric malnutrition.
|
|
|
How does prematurity affect the interpretation of growth charts?
How do you compensate for this? At what age is this compensation no longer useful? |
Premature babies will usually be short and/or wasted if their actual birthdate is used to calculate their age.
To allow for this, their expected birthdate should be used instead. This allowance should be made for weight until 24 months and for height until 40 months. |
|
|
How much weight and length do babies gain per day in the first three months of life (on average)?
|
Weight: 25-30g
Height: 0.9 mm |
|
|
T/F: Failure to thrive can be used to describe a child with just wasting or stunting, or both together.
|
True - FTT can be used to describe all three situations.
|
|
|
T/F: A child on the 10th percentile for weight and height cannot be said to be 'failing to thrive'
|
False - if the child has fallen to the 10 percentile from a significantly higher one, this is referred to as relative FTT.
|
|
|
What is the difference between undernutrition and malnutrition?
|
Undernutrition - not enough food
Malnutrition - caloric intake may be sufficient but essential components are deficient, e.g. vitamins |
|
|
T/F: Starvation (energy malnutrition) will generally be accompanied by protein malnutrition, but protein malnutrition does not lead to energy malnutrition.
|
False - protein malnutrition causes a loss of appetite which is often severe enough to cause actual caloric undernutrition.
|
|
|
T/F: Children and the elderly have higher daily protein requirements than the average
|
True - children need it for growth, older people need more to offset less efficient utilisation.
|
|
|
T/F: Children and the elderly have higher daily energy requirements than the average
|
False - children do but the elderly have reduced requirements due to a reduced BMR and decreased lean body mass.
|
|
|
How does the pattern of protein loss differ between marasmus and kwashiorkor?
|
In marasmus, the protein loss is predominantly from skeletal muscle.
In kwashiorkor, the liver and gut are depleted of protein. |
|
|
How does rotavirus cause diarrhea? (2)
|
Impaired absorption due to death of differentiated enterocytes and replacement with non-absorptive crypt cells.
Increased chloride secretion due to an increase in intracellular calcium caused by a capsid protein |
|
|
How do helminth infections cause diarrhea?
|
By inducing mast cell degranulation and profuse inflammatory secretion (intestinal anaphylaxis).
|
|
|
What is the equation for calculating the stool osmotic gap?
What results diagnose secretory and osmotic diarrhea respectively? |
Osmotic gap = stool osmolality (~290) - 2 x ([Na+] + [K+])
A normal gap is less than 50; this also corresponds to a secretory diarrhea. > 50 implies an osmotic diarrhea. |
|
|
What degree of fluid-related weight loss corresponds to severe dehydration?
|
10% or more
|
|
|
What is the immediate management of a severely dehydrated child? (3 parts)
|
If in shock: resuscitate with IV bolus.
If not, check acid-base, urea and electrolytes first. Rehydrate over 4-6h with regular clinical and biochemical review |
|
|
Why is glucose included in oral rehydration solutions?
|
It stimulates Na+ reabsorption via SGLT-1, thus encouraging more fluid uptake.
|
|
|
What causes the acidosis seen in dehydration? (3)
|
Increased bicarbonate loss in the stool
Decreased H+ excretion in the kidney due to low GFR Increased lactic acid production due to poor perfusion of tissues |
|
|
What makes diluted juice a poor rehydrating alternative? (3)
|
Low Na+ - doesn't stimulate SGLT-1
No potassium Sugar may act as an osmotic laxative |
|
|
Why is extra care (and ongoing monitoring) needed when rehydrating patients with hypernatraemic dehydration?
|
Because a sudden drop in their sodium will cause a fluid shift into the tissues, leading to life-threatening cerebral oedema.
|
|
|
T/F: Blood pressure monitoring is the most reliable and sensitive non-invasive means of assessing the effectiveness of rehydration.
|
False - BP drops late in dehydration and so will rise to normal early in rehydration. Heart rate is both more sensitive and reliable.
|
|
|
T/F: Food should be given to a child with gastroenteritis as soon as she is willing to eat.
|
True - caloric deficit will only worsen damage and prolong recovery.
|
|
|
T/F: The diet of a child recovering from gastroenteritis is frequently altered for the duration of the recovery phase.
|
True - in cases of secondary lactose intolerance, milk and other lactose-containing dairy foods are generally best avoided.
|
|
|
What medications are in routine use for the treatment of gastroenteritis in children?
|
None - treatment is replacement of fluid and electrolytes, and nutritional support.
|
|
|
Name four situations in which antibiotics would be used to treat a case of paediatric gastroenteritis.
|
Bacterial sepsis
Shigella infection Giardia infection Helminth infestation |
|
|
T/F: Rotavirus and Norwalk-like viruses are found to be causative in most cases of infectious diarrhea
|
False - they are probably the most common causative pathogens, but in most cases, no agent is identified.
|
|
|
What is the most common bacterial cause of diarrhea in Australia?
|
Campylobacter jejuni
|
|
|
T/F: Most cases of diarrhea are caused by infection
|
True
|
|
|
T/F: Most cases of infectious diarrhea are caused by viral pathogens
|
True
|
|
|
What diarrhea-causing pathogens are associated with poorly cooked chicken? (2)
|
Salmonella sp.
Campylobacter jejuni |
|
|
T/F: Diarrhea-causing viruses may be transmitted by faecal-oral, respiratory, food or drinking water routes.
|
True - though food and water are less common modes of transmission.
|
|
|
What are SR(S)Vs and SR(U)Vs?
What are they related to? |
Small Round Structured (or Unstructured) viruses which are related to the Norwalk virus.
|
|
|
What diarrheal pathogens (2) are neonates more prone to?
|
Enteropathic E. coli (EPEC)
Clostridium difficile |
|
|
What pathogens cause enteric (typhoid and paratyphoid) fevers?
|
Salmonella typhi and paratyphi (A+B)
|
|
|
What is EHEC?
Why is it clinically important? |
Enterohaemorrhagic E. coli.
It is important because it expresses verotoxin (Shiga-like toxin) which can cause haemolytic uraemic syndrome. |
|
|
What viral diarrheal agents can be tested for by immune assay? (2)
How are other viral pathogens identified? |
Rota viruses and adenoviruses can be identified by immunoassay.
Others are identified by electron microscopy. |
|
|
What is the antibiotic of choice for Campylobacter jejuni diarrhea (assuming antibiotics are needed)?
|
Erythromycin
|
|
|
How are parasites such as Giardia and Entamoeba identified from stool samples?
|
By microscopy
|
|
|
What is the purpose of adding selenite broth to growth medium when culturing a stool sample?
|
Selenite broth is used to isolate Salmonella and Shigella species.
|
|
|
T/F: Salmonella diarrhea should not be treated by antibiotics unless caused by Salmonella typhii.
|
True
|
|
|
What is "Montezuma's Revenge" also known as?
What causes it? |
Montezuma's Revenge, a.k.a. traveller's diarrhea, is cause by enterotoxigenic E. coli (ETEC).
|
|
|
Name five strains of diarrheal E. coli.
Which (*) cause bloody diarrhea? Which (#) causes haemolytic uraemic syndrome? Which (@) are known as 'childhood diarrhea'? |
Enteroaddherent (EAEC)@
Enterohaemolytic (EHEC)*# Enteroinvasive (EIEC)* Enteropathogenic (EPEC)@ Enterotoxigenic (ETEC) |
|
|
Which antibiotic has good efficacy against both Campylobacter and Enterobacteriaceae (E. coli, Salmonella, Shigella etc) species
|
Ciprofloxacin
|
|
|
What nutrient deficiencies tend to exacerbate diarrheal illnesses in the developing world? (2)
|
Zinc
Vitamin A |
|
|
tyvärr
dessvärre olyckligtvis |
δυστυχώς
|
|
|
T/F: Enterotoxins produced by ETEC work via the same mechanism as cholera toxin.
|
True - they raise cAMP levels in the enterocytes. They also act by increasing cGMP, which has a similar effect on fluid secretion.
|
|
|
How does steatorrhea cause a secretory diarrhea?
|
Dihidroxy fatty acids produced by colonic bacteria stimulate enterocyte secretion.
|
|
|
How does abetalipoproteinaemia cause diarrhea?
|
Abetalipoproteinaemia causes impaired fat absorption due to abnormal chylomicron formation.
The ensuing steatorrhea causes a secretory diarrhea. |
|
|
T/F: Steatorrhea does not occur in GIT infections or malnutrition
|
False - it is unusual for infections but can accompany severe malnutrition due to the impairment of pancreatic enzyme production.
|
|
|
T/F: Bloody diarrhea is always due to infection or IBD
|
False - it can be due to food allergy also.
|
|
|
What virus can cause bloody diarrhea in an immunocompromised individual?
|
CMV
|
|
|
What is the recommended treatment for ETEC (traveller's diarrhea)?
|
Bactrim
(trimethoprim + sulfonamide) |
|
|
How can S. aureus food poisoning be distinguished from that caused by Salmonella?
|
Onset and duration of symptoms - S. aureus causes symptoms within 6 hours and lasts for around 12.
Salmonella takes 6-72 hours to cause symptoms and lasts for 3-7 days. |
|
|
What is the first-line antibiotic for Giardia lamblia?
|
Metronidazole
|
|
|
What pumps/channels (2) are responsible for the absorption of NaCl in the colon?
|
Na+/H+ exchanger
ENaC |
|
|
What did love in the time of cholera lead to cystic fibrosis (according to one theory)?
|
Because heterzygotes for a CFTR defect were (hypothetically) resistant to the worst effects of cholera, and thus were more likely to produce more kids.
|
|
|
T/F: ENaC and CFTR are responsible for the electrogenic absorption of Na+ and Cl- respectively throughout the colon.
|
False - ENaC allows electrogenic Na+ absorption, but CFTR is responsible for electrogenic Cl- secretion.
|
|
|
What happens to the H+ and HCO3- ions which are exchanged for Na+ and Cl- throughout the colon?
What happens in diarrhea? |
H+ and HCO3- combine to form H2CO3, which dissociates to form water and carbon dioxide.
The carbon dioxide is reabsorbed and converted back to bicarbonate by carbonic anhydrase. In diarrhea, this reconversion is overwhelming, meaning bicarbonate cannot be replenished as fast as it is secreted, leading to acidosis. |
|
|
How does sodium absorption in the descending colon differ from that in the ascending colon?
|
Electroneutral in the proximal colon
Electrogenic in the descending. |
|
|
T/F: The rectum absorbs little or no sodium and water
|
True
|
|
|
How does aldosterone affect colonic absorption of salt and water?
|
It increases it by upregulating ENaC (amiloride-sensitive) channels in the apical membrane.
|
|

Name the mushroom shown.
Why shouldn't you eat it? |
Amanita phylloides, a.k.a. Death Cap.
It causes fatal hepatotoxicity. |
|
|
What is the toxin implicated in scrombroid fish poisoning?
Where does it come from? |
Histamine - produced by bacterial breakdown of histidine.
|
|
|
What toxin do reef fish often accumulate which can cause food poisoning in humans?
Where does it come from? |
Ciguatoxin - accumulated due to the fish ingesting dinoflagellate species which produce it.
|
|
|
What are brevitoxin, saxitoxin and domoic acid?
What produces them? |
They are marine biotoxins found in shellfish which can cause food poisoning.
They are produced by algae. |
|
|
What toxin is found in the puffer fish?
|
Tetrodotoxin
|
|
|
T/F: Ciguatoxin, histamine, brevitoxin, saxitoxin, domoic acid and tetrodotoxin are not rendered inert by heat.
|
True - they are all heat stable toxins
|
|
|
T/F: Antacids and PPIs both increase a person's risk of food poisoning.
|
False - toxins associated with food poisoning are generally unaffected by stomach acid anyway.
|
|
|
What blood group is at greater risk of contracting a gastrointestinal infection due to cholera, EHEC or norovirus?
|
O
|
|
|
T/F: Rotavirus and norovirus infections peak during winter
|
True
|
|
|
T/F: Norovirus (nee Norwalk) causes vomiting in >50% of cases.
|
True
|
|
|
T/F: Oysters are a prominent source of rotavirus and norovirus outbreaks.
|
False - only norovirus (and hepatitis A) are commonly spread by oyster contamination.
|
|
|
What are the main clinical differences between enterotoxic and enteroinvasive bacterial enteritis in terms of:
- incubation period - fever - stool volume - duration of symptoms - faecal white cells? |
Entertoxic enteritis:
- has a shorter incubation and duration - causes less fever but greater stool volume - does not result in faecal white cells. |
|
|
What percentage of travellers who stay in a developing country for one moth will develop some kind of diarrhea?
What percentage are severe cases? |
40%
13% are severe |
|
|
What parts of the GI tract are most affected by toxigenic diarrhea?
|
Duodenum and ileum
|
|
|
What parts of the GI tract are most affected by invasive diarrhea?
|
Terminal ileum and colon
|
|
|
T/F: Campylobacter, Salmonella and Yersinia ss, all cause an invasive diarrhea
|
True
|
|
|
T/F: Giardia intestinalis (nee lamblia) causes steatorrhea
|
True
|
|
|
T/F: Giardia intestinalis (nee lamblia) has a slow onset, causes relapsing infection in IgA deficient people, and responds to metronidazole.
|
True
|
|
|
What age group is most commonly affected by protozoan (Giardia or Cryptosporidium) enteropathy?
|
Infants
|
|
|
T/F: AIDS patients with persistent cryptosporidium infection may be treated effectively with antibiotics but most people will not need such intervention
|
False - antibiotics are usually unnecessary in cryptosporidiosis, and are generally ineffective anyway. The only option for AIDS patients is to try to boost their defences.
|
|
|
What is the incubation period for enteric (typhoid) fever?
|
1-2 weeks
|
|
|
T/F: Enteric (typhoid) fever initially causes constipation rather than diarrhea
|
True
|
|
|
T/F: Enteric (typhoid) fever is characterised by a relapsing-remitting fever
|
False - the fever is continuous
|
|
|
Name four typical clinical findings in enteric (typhoid) fever,
|
Continuous fever
Weight loss Splenomegaly Constipation |
|
|
What is the relapse rate of enteric (typhoid) fever in the convalescent phase?
|
~10%
|
|
|
T/F: Enteric (typhoid) fever may be transmitted by someone in the convalescent phase
|
True - faecal excretion is prolonged and can be transmitted via food preparation.
|
|
|
T/F: Salmonella enterica shows tropism for Peyer's patches
|
True - this leads to ulceration and bacteraemia
|
|
|
T/F: Enterica (typhoid) fever can involve the lungs, causing a productive cough.
|
False - it can involve the lungs but causes a dry cough
|
|
|
T/F: Perforation and haemorrhage are major complications of enteric (typhoid) fever which happen in the early febrile phase.
|
False - these happen late in the course of the disease after ulceration and necrosis have weakened the ileal gut wall.
|
|
|
How is typhoid diagnosed?
|
Blood culture
|
|
|
What are the first line antibiotics against enteric (typhoid) fever?
|
3rd gen cephalosporins
(Ceftriaxone, cefotaxime) |
|
|
T/F: Fluoroquinolone resistance in Indian strains of enteric (typhoid) fever is currently low
|
False - 90% of such cases are resistant to ciprofloxacin
|
|
|
What is the only macrolide which is useful against enteric (typhoid) fever?
|
Azithromycin
|
|
|
T/F: Fever in cases of typhoid comes down slowly with IV antibiotics, even when non-resistant.
|
True - it often takes several days (cf. 24-28 hours with most infections)
|
|
|
What organism causes amoebiasis?
|
Entamoeba histolytica
|
|
|
What is verotoxic E. coli also known as?
|
Enterohaemorrhagic E. coli
|
|
|
What are the main causes of infective colitis in Australia? (5)
|
EHEC
Shigella ss. Entamoeba histolytica Campylobacter jejuni Clostridium difficile |
|
|
What is the typical incubation period and duration of infective colitis (non-typhoid)?
|
Incubation: 1-3 days
Duration: up to three weeks |
|
|
What two clinical features are most useful in distinguishing invasive enteritis from appendicitis?
|
Appendicitis causes diarrhea very rarely.
Invasive enteritis does not cause rebound tenderness. |
|
|
What enteritis-causing pathogen can also cause intravascular haemolysis?
|
Enterohaemorrhagic E. coli (EHEC)
|
|
|
What feature of vancomycin makes it useful for C. difficile colitis?
|
It is not absorbed into the blood when ingested and therefore not toxic.
|
|
|
What two drugs are used for C. difficile colitis?
|
Metronidazole (Flagyl)
Vancomycin |
|
|
Which antibiotics (2) most frequently cause C. difficile colitis?
|
Clindamycin
Beta-lactams |
|
|
Which antibiotic class (almost) never causes C. difficile colitis?
|
Aminoglycosides
|
|
|
Name four causes of diarrhea in hospitalised patients that do not relate to infective causes.
|
Hyperosmolar feeding
Sorbitol or mannitol elixirs Drugs Ischaemic colitis |
|
|
T/F: Colchicine use can cause diarrhea.
|
True
|
|
|
Name four pathogens (or genera of pathogen) which produce 'enteroinvasive' symptoms (bloody diarrhea + fever)?
|
Shigella
Salmonella EHEC Campylobacter |
|
|
What should oral rehydration solutions contain other than water?
Why? |
Electrolytes, esp. Na+ and K+ (to replace losses and prevent dilution)
Glucose or sucrose (to enhance Na+ absorption). |
|
|
What electrolytes should be included in oral rehydration solutions? (4)
|
Na
K HCO3 Cl |
|
|
Name two anti-emetics that work by antagonising dopamine receptors.
|
Metoclopramide (Maxolon)
Prochlorperazine (Stemetil) |
|
|
Name an anti-emetic that works by antagonising serotonin receptors.
|
Ondansetron
|
|
|
What does loperamide do?
How does it work? |
It is an anti-diarrheal drug.
It works by slowing peristalsis down by acting on opioid receptors in the myenteric plexuses. |
|
|
Name two opioid agonists used to treat diarrhea.
|
Diphenoxylate
Loperamide |
|
|
What drugs will tend to cause toxic megacolon in infective colitis due to shigella, EHEC or C. difficile?
|
Those which reduce motility, i.e. the opioid agonists:
Loperamide Diphenoxylate |
|
|
What antibiotics is protozoal infective colitis (entamoeba, giardia) usually treated with?
|
A nitroimidazole, such as metronidazole.
|
|
|
T/F: Apart from enteric (typhoid) fever, most cases of traveller's diarrhea are treatable with a fluoroquinolone such as ciprofloxacin.
|
True
|
|
|
T/F: The risk of reactive arthritis is over seven times higher following Yersinia enteritis than after Campylobacter enteritis
|
True
|
|
|
Which bacterial cause of enteritis is associated with Guillain-Barre syndrome?
|
Campylobacter jejuni
|
|
|
Which bacterial cause of enteritis is associated with Erythema nodosum?
|
Yersinia enterocolitica
|
|
|
T/F: Reactive arthritis can follow infective enteritis of any cause
|
True
|
|
|
T/F: CMV infection can cause profuse diarrhea in otherwise healthy adults
|
False - this will usually only occur in immunocompromised hosts.
|
|
|
Name three causes of enteritis which generally only cause disease in immunocompromised hosts.
|
CMV
Microsporidia ss. Mycobacterium avium |
|
|
Name five protozoan species which can cause persistent diarrhea.
Which* is so confined to HIV+ patients as to be almost diagnostic of HIV seropositivity? |
Giardia lamblia
Cryptosporidium parvum Entamoeba histolytica Cyclospora cayetanensis Isospora belli* |

