![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
What are the main hormones involves in:
1. Pregnancy 2. Parturition 3. Lactation? |
1. Pregnancy
- hCG - Estrogens - Progesterone 2. Parturition - Oxytocin - Prostaglandins - Relaxin 3. Lactation - Oxytocin - Prolactin |
|
|
Describe the role of placental progesterone and oestrogens in pregnancy
|
Progesterone:
- Suppresses myometrial contractions throughout pregnancy - Promotes formation of mucous plug in cervical canal - Prepares mammary glands for lactation Oestrogen: - Proliferative effect on • Uterus • Breasts = Ductal structure - Preparation of uterus and cervix for labour - Induction of pro-labour genes? |
|
|
Define the stages of labour
|
1. First stage
- Starts with increased prostaglain synthesis and release stimulating more forceful contractions and increased sensitivity to oxytocin - Causes the initiation and increasing force of contractions to push the foetus into the birth canal - Ends when cervical dilation reaches 10 cm 2. Second stage of labour - 10cm dilation - Ends with the full birth of the foetus - Usually lasts up to 1 hour in the multiparous woman, or 2 hours in the prmi gravida 3. Third stage - Following birth of foetus - Powerful uterine contraction, separating the placenta from the uterine wall and expelling it - Normally within 10 minutes |
|
|
Describe the processes necessary to create a birth canal and its clinical assessment
|
The creation of a birth canal requires:
1. The release of the structures which normally retain the fetus in utero - At some time during the cervical dilation process the fetal membranes rupture, releasing amniotic fluid. 2. The enlargement and realignment of the cervix and vagina - The birth canal diameter cannot extend beyond the limits determined by the pelvis. • The true diameter of this inlet is normally about 11cm. • Softening of the pelvic ligaments may allow some expansion to occur. - To create a birth canal the cervix must dilate and be retracted anteriorly. - Cervical dilatation is facilitated by structural changes known as cervical ripening, but produced by forceful contractions of uterine smooth muscle. - These contractions first thin the cervix (‘effacement’) and then dilate it. |
|
|
Describe the functions and mechanisms of cervical ripening
|
- The cervix has a high connective tissue content made up of collagen fibres embedded
in a proteoglycan matrix. - Ripening involves a marked reduction in collagen and marked increase in glycosaminoglycans (GAG’s) which decrease the aggregation of collagen fibres. - Keratin sulphate increases at the expense of dermaton sulphate. - In consequence collagen bundles ‘loosen’. - There is also influx of inflammatory cells, and increase in nitric oxide output. - All of these changes are triggered by prostaglandins, namely E2 and F2x. - These aid the ability of the cervix to dilate |
|
|
Describe the properties of uterine smooth muscle that facilitate labour
|
- The myometrium is made up of bundles of smooth muscle cells.
- During pregnancy, the myometrium gets much thicker due primarily to increased cell size (10 fold) and glycogen deposition. - An intracellular apparatus containing actin and myosin, triggered by a rise in intracellular calcium concentration, generates force. - The rise in calcium concentration is produced by action potentials in the cell membrane. - Action potentials spread from cell to cell via specialised gap functions, allowing coordinated contractions to spread over the myometrium. - Some smooth muscle cells are capable of spontaneous depolarization and action potential generation, and so can act as ‘pacemakers’. - The myometrium is therefore always spontaneously motile. - In early pregnancy contractions may occur every 30 minutes or so, but are of low amplitude. - As pregnancy continues, the frequency falls, with some increase in amplitude, producing noticeable ‘Braxton-Hicks’ contractions. - None of these contractions are normally forceful enough to have any effect on the fetus. - Uterine smooth muscle has another crucial property = brachystasis. • At each contraction muscle fibres shorten, but do not relax fully. • The uterus, particularly the fundal region therefore shortens progressively. • This pushes the presenting part into the birth canal and stretches the cervix over it. |
|
|
Describe the normal physiological processes that initiate labour
|
- The onset of labour is a relatively sudden increase in the frequency and force of
contractions. - Two hormones are implicated in this change: 1. Prostaglandins: • These act by enhancing the release of calcium from intracellular stores • The endometrium is a major producer • The major factor influencing its release in the endometrium is the oestrogen/progesterone ratio • If progesterone is high relative to oestrogen, prostaglandin synthesis is low. • A fall in progesterone or rise in oestrogen increases prostaglandin synthesis. 2. Oxcytocin: • This peptide hormone is secreted from the posterior pituitary gland under the control of neurons in the hypothalamus. • It acts by lowering the threshold for triggering action potentials • Oxytocin acts by binding to receptors on uterine smooth muscle cells. • A fall in progesterone levels relative to oestrogen increases the receptor population making cells more sensitive to low circulating levels of the hormone. - The onset of labour is therefore associated with increased prostaglandin synthesis and release stimulating more forceful contractions, in conjunction with increased sensitivity to oxytocin. - All the evidence from animals suggests that labour is initiated by an increased in PG production and oxytocin sensitivity triggered by a fall in progesterone levels relative to oestrogen - However, this is less clear in the human = there is no clear evidence of pre-labour increases in plasma PGs or changes in oestrogen progesterone ratio. However, PGs will induce labour |
|
|
Describe the 1st stage of labour
|
- Contractions become stronger and more forceful, signalling the beginning of labour and causing the beginning of cervical dilatation and the descent of the foetal head
- As contractions increase, the ‘Ferguson Reflex’ increases oxytocin secretion massively: 1. Baby's head stretches the cervix 2. Cervical stretch stimulates oxytocin release and thus excites fundic contraction 3. Fundic contraction pushes baby down, stretching cervix further 4. Cycle repeats over and over again - This ‘positive feedback’ of oxytocin makes contractions more forceful and frequent. - This progressively allows the descent of the foetal head until it engages in the pelvis = 10cm dilatation |
|
|
Describe the 2nd stage of labour
|
- The first stage of labour ends when cervical dilatation reaches 10 cm.
- The fetus is normally then expelled relatively quickly. - The second stage of labour normally lasts up to 1 hour in the multiparous woman, and 2 hours or more in primi gravida. - The descended head flexes as it meets the pelvic floor, reducing the diameter of presentation. There is then internal rotation. - The sharply flexed head descends to the vulva, so stretching the vagina and perineum. - The head is then delivered (‘crowning’), and as it emerges it rotates back to its original position and extends. - The shoulders then rotate followed by the head, and the shoulders deliver followed rapidly by the rest of the fetus. -The second stage of labour ends with delivery of the fetus. - The risk of tearing to the perineum and vagina may be reduced by episiotomy. |
|
|
Describe the 3rd stage of labour - what processes normally limit maternal blood loss after birth?
|
- With the fetus removed there is a powerful uterine contraction, which separates the placenta, positioning it into the upper part of the vagina, or lower uterine segment.
- The placenta and membranes are then expelled, normally within about 10 minutes. - This completes the third stage of labour. - This contraction of the uterus also compresses blood vessels and reduces bleeding. - It is normally enhanced by administration of an oxytocic drug. |
|
|
Describe the immediate physiological changes in the neonate which enable independent life
|
- Within a short time of delivery the fetus takes its first breath triggered by multiple stimuli
= delivery trauma, temperature change and others. - This causes a dramatic fall in pulmonary vascular resistance, so reducing pulmonary arterial pressure and increasing left atrial pressure relative to right atrial pressure. - The atrial pressure change shuts the foramen ovale, and rising arterial pO2 causing the ductus arteriosus to constrict, so establishing the adult form of circulation. - The sphincter in the ductus venosus constricts, so that all blood entering the liver passes through the hepatic sinusoids. |
|
|
Describe the 5 most common foetal presentations
|
‘Presentation’ refers to the part of the fetus which lies at the pelvic brim or in the lower pole of the uterus.
1. Vertex - The most common foetal presentation approx. 96% of all term pregnancies - Usually occipito-anterior, but can be occipito-posterior - A cephalic presentation (but not only one) 2. Breech - The second most common presentation occurring in approx. 3% of all term pregnancies - Much more common in pre-term labour because it is a normal stage of transition and found much more commonly earlier in pregnancy when the fetus has more room for manoeuvre. 3. Shoulder presentation - When the fetal lie is transverse the shoulder is most likely to present. - Incidence is roughly 0.4% (1 in 250) pregnancies 4. Face presentation - Type of cephalic presentation roughly 0.2% (1 in 500) pregnancies - Mentoposterior - Complete extension = face - ?may deliver spontaneously = could be cord around neck, goitre or hydrocephaly causing head to be pushed back 5. Brow presentation - A cephalic presentation, roughly 0.1% (1 in 1000) pregnancies - If head is deflexed at the onset of labour, extension can occur. Partial extension (brow) will not deliver and must change to a face presentation |
|
|
Describe the main principles of inducing labour
|
- Induction of labour is an intervention designed to artificially initiate uterine contractions leading to progressive dilatation and effacement of the cervix and birth of the baby.
- Is to expedite the birth of the baby when it is agreed that the fetus and/or mother will benefit from a higher probability of a healthy outcome than if birth is delayed. - Should only be considered when vaginal delivery is considered appropriate and is very painful - Main methods: • Membrane sweep = stretch cervix and sweep aside membranes • Prostaglandins (PGE2) – given vaginally into posterior fornix • Oxytocin – given as IV infusion (preferably after rupture of membranes) |
|
|
Describe how the physiological state of the foetus may be monitored during labour
|
- Relies mostly on fetal heart rate
• Will naturally accelerate on contractions as foetal blood supply may be sporadically cut off. However, if fallen too low sign of foetal distress • Baseline 110-160 (bpm) • Variability (bpm) = >5 (if <5 foetus may be asleep but may be serious so repeat later) • Decelerations : none • Accelerations : present • May use intermittent foetal monitoring using Pinnard's stethescope • May use continuous electronic monitoring but restricts mobility - Meconium is an indicator too = first bowel movement of a neonate and should be passed in utero = only if foetus is distressed. Will stain liqua blackish-green - For a woman who is healthy and has had an otherwise uncomplicated pregnancy, intermittent auscultation should be offered and recommended in labour to monitor fetal wellbeing. - How often depends on stage of labour • Onset of regular contractions to full dilation = every 15 mins for 60 secs • Full dilatation to full expulsion of foetus = after each contraction for 60 seconds |
|
|
Describe how delivery may be facilitated by intervention
|
Social
1. Control 2. Support 3. Mobility 4. Position 5. Nutrition and hydration 6. Bladder and bowel empty 7. Dim lighting and music 8. Water bath Medical - Forceps - Ventouse - Episiotomy - Augmentation = oxytocin - Caesarean section - Pain relief |
|
|
Describe the constituents of human breast milk
|
- Milk is secreted in significant quantities from soon after birth.
- The composition varies with time. - In the first week up to 40ml/day of colostrum is secreted. • Colostrum contains less water-soluble vitamins, fat and sugar than later milk, but much more protein, fat-soluble vitamins, and immunoglobulins. - Over the next 2-3 weeks, IgG and total protein declines, whilst, fat and sugar rises, to produce mature milk. - Composition of human mature milk: • Water 90% • Lactose 7% • Fat 2% • Proteins, including lactalbumin and lactoglobulin • Minerals Ca2+, Fe, Mg, K, Na, P, S • Vitamin A, B, B2, B2, C, D, E, K • Ph 7.0 • Energy Value 27MJ.l-1 |
|
|
Outline the mechanisms of production of milk in the lactating breast
|
- The alveoli are the site of milk synthesis.
- Myoepithelial cells, which are smooth muscle cells responsible for milk let down, surround alveoli. - Milk fat is synthesised in the smooth endoplasmic reticulum of the alveolar cells and passes in membrane bound droplets towards the lumen. - Milk protein passes through the golgi apparatus and is released by exocytosis |
|
|
Describe the hormonal growth and development of mammary tissues
|
- At birth only a few ducts are present, and the breast remains the same until puberty.
- At this time oestrogens cause the ducts to sprout and branch and the ends form masses of cells that later become alveoli. - In the non-pregnant woman there are cyclic changes in the breast under the influence of oestrogen and progesterone. - Most development of mammary tissue occurs during pregnancy. - Rising titres of oestrogen and progesterone in early pregnancy stimulate a considerable hypertrophy of the ductular-lobular-alveolar system. - Prominent lobules form and the lumina of alveoli become dilated. - The alveolar cells differentiate in mid-pregnancy. Cells are capable of secretion from this time, and contain substantial amounts of secretory material, but milk is not secreted in significant quantities. |
|
|
Describe the hormonal control of milk production and milk let down
|
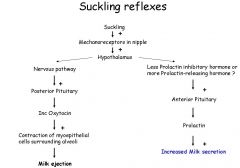
- During pregnancy a high progesterone/oestrogen ratio favours development of alveoli,
but not secretion. - At birth, progesterone levels fall precipitously, and oestrogen levels less so. - These changes lead to the alveolar cells becoming responsive to prolactin. - Prolactin is secreted from the anterior pituitary, under the control of the hypothalamus. - The infant stimulates receptors in the nipple mechanically. - Impulses pass up to the brain stem, and to the hypothalamus to reduce the secretion of dopamine and vasoactive intestinal peptide, so promoting prolactin secretion. - The amount of milk produced before the next feed depends upon the suckling stimulus. - Milk is produced continuously between feeds and accumulates in the ducts, increasing the turgor of the breast. - When the infant suckles a second reflex promotes milk ‘let down’. - This is a dramatic increase in the secretion of oxytocin from the posterior pituitary gland. - This contracts myoepithelial cells which eject the milk. |
|
|
Describe the mechanisms which produce cessation of lactation
|
- If the infant does not suckle prolactin levels fall after birth → as inhibitory levels remain high and therefore no milk is produced
- If suckling stops milk production will cease, in part through lower prolactin levels, in part due to turgor-induced damage to the breast. |
|
|
What are the 3 elements of labour that must be analysed for a normal birth?
|
1. The Powers:
- Delivery of the fetus is dependent on contraction of the myometrium, which has undergone considerable hypertrophy and hyperplasia during pregnancy. - Contraction and retraction of the multidirectional smooth muscle fibres causes progressive shortening, particularly in the fundus of the uterus. - Uterine contractions can be assessed in terms of frequency, amplitude and duration. 2. The Passage: - The passage is formed by the bony pelvis and soft tissues. - The pelvic inlet is shorter in the anterior - posterior plane (obstetric conjugate, 10.5cm). - Between the pelvic inlet and outlet, the mid-cavity is circular (12cm diameter). - The pelvic outlet is narrowest usually mediolaterally (11cm). - The fetus flexes, extends and rotates as it passes through the birth canal. - Resistance of the soft tissue can slow labour. 3. The Passenger: - The size and presentation of the fetus is critical in labour. - The orientation of the head of the fetus when entering the pelvis (in a cephalic delivery) is variable and as such the head diameter of the fetus is different in differing positions. - However, moulding of the fetal cranium may occur since cranial sutures have not yet fused. - Progress in labour is plotted graphically on a partogram. |

