![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
90 Cards in this Set
- Front
- Back
|
Unintentional weight loss characteristics
|
Loss of 10 pounds or > 5% of baseline body weight in 6-12 months.
First establish if the weight loss is intentional Inquire if the patient's food intake is less, or the same/increased |
|
|
Differential of weight loss
|
DECREASED BODY MASS
Depression Endocrinopathy Cancer Renal Failure Enteric Access to Food Systemic inflammatory disease Eating difficulty Diabetes Mellitus Bulimia & Anorexia Opportunistic Infection Dementia Yucky food Medication side effects Aging Systemic chronic disease Schizophrenia/psychosis |
|
|
Lymphoma
|
malignancy of white blood cells arising in the lymph nodes.
|
|
|
Leukemia
|
Lymphoid neoplasms with widespread involvement of bone marrow. Tumor cells are usually found in the peripheral blood
|
|
|
Non-hodgkin Lymphoma
|
- Burkitt's: African pt w/ jaw mass
- Diffuse large B cell - Mantle Cell t(11:14) deactivation of cyclin D regulatory gene, CD5+, poor prognosis Follicular t(14;18) bcl-2 expression, which inhibits apoptosis, indolent course but difficult to cure Lymphoblastic T cell, children, mediastinal mass Cutaneous T cell, mycosis fungoides Adult T cell with HTLV-1 infection Marginal Cell MALToma H pylori associated |
|
|
Burkitt's Lymphoma
|
Highly aggressive B cell non-hodgkin lymphoma "starry sky" histology sheets of lymphocytes with interspersed macrophages
Occurs in children and young adults sporadic, or associated with HIV |
|
|
Burkitt's Lymphoma is associated with?
|
In Africa associated with Ebstein Barr Virus and presents as maxillary/mandibular mass
|
|
|
Genes of Burkitt's Lymphoma
|
c-MYC gene on chromosome 8 t(8;14) places c-MYC proto-oncogene adjustment to immunoglobulin heavy chain locus on 14w overexpression of the transcription factor c-MYC that leads to increased cell-growth CD20, CD10, and BCL-6.
|
|
|
Treatment of Burkitt's Lymphoma may lead to?
|
Treatment may lead to tumor lysis syndrome low phos, low calcium, increased uric acid, increased potassium and AKI, preventable w/ hydration and allopurinol.
|
|
|
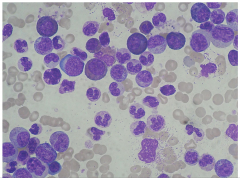
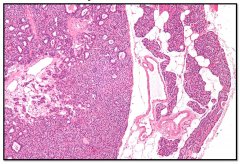
Burkitt's Lymphoma
|
|
|
B symptoms of Hodgkin's Lymphoma
|
Wt loss, fever, night swears - patients sometimes itch, node doesn't hurt
|
|
|
Cells of Hodgkin's Lymphoma
|
Reed-Sternberg cells - formed from germinal B cell centers CD15+ CD30+
|
|
|
Hodgkin's Lymphoma Treatment
|
Curable, excision +XRT or advanced ABVD chemo adriamycin, bleomycin, vinblastine, dacarbazine
|
|
|
Subtypes of Hodgkin's Lymphoma
|
- Nodular sclerosis
- lymphocyte predominance - lymphocyte rich - lymphocyte depleted (HIV) or mixed cellularity (25% older patients with EBV) - Prognosis better with more lymphocytes and less Reed Sternberg cells |
|
|
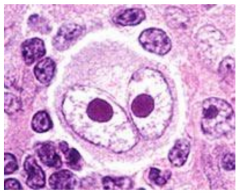
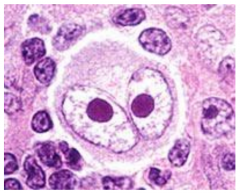
Hodgkin's Reed Sternberg Cell characterized by large size, bilobed nucleus, and nucleolar inclusion bodies "owl's eyes"
|
|
|
Vincristine: Mechanism
|
M phase specific that blocks polymerization of microtubules so mitotic spindle cannot form
|
|
|
Vincrisitne : Uses
|
Acute leukemia, Hodkin's, WIlms tumor, choriocarcinoma
|
|
|
Side Effects of Vinblastine
|
Neuropathy peripheral neuritis, areflexia, paralytic ileus
|
|
|
Part of MOPP regimen for Hodgkin Lymphoma
|
Mustargen, oncovin, procarbazine, prednisone
|
|
|
Signs and Symptoms for Leukemia
|
Leukemia is unregulated growth of leukocytes in bone marrow so in addition to bone pain many symptoms are related to problems of production
There is decreased working WBCs (infections, esp cellulitis) Decreased Hgb & HCT (fatigue, dyspnea on exertion, pallor on exams) Decreased platelets (Bleeding gums, epistaxis, petechiae) Leukemic infiltrates can occur in liver, spleen, and lymph nodes. Hepatosplenomegaly on exam |
|
|
CML Chronic Myelogenous Leukemia: Cytogenic analysis
|
t(9;22) Philadelphia chromosome results BCR-ABL fusion gene, translocation of ABL proto-oncogene to BCR
Bcr-Abl fusion protein results in constitutively active Abl tyrosine kinase in the Ras/Raf/MEK/MAPK pathway which leads to inhibition of apoptosis and unregulated cell division. |
|
|
Age of onset of CML
|
35-55
|
|
|
Associated symptoms of CML
|
Splenomegaly, hepatomegaly, lymphadenopathy
|
|
|
Blood characteristics of CML
|
Leukocytosis, normocytic to macrocytic anemia
Bone marrow is hypercellular |
|
|
Effect of CML on platelets
|
Platelet derangement either thrombocytosis during active phase or thromobocytopenia in spent phase
|
|
|
Histology of CML
|
Promyelocytes, big cell and nuclei, coarse grains in cytoplasm, basophilic
|
|
|
Hydroxyurea
|
S phase specific agent binds ribonucleotide reductase and inhibits the formation of DNA
Used in melanoma, CML, and sickles cell disease |
|
|
Hydroxyurea : side effects
|
nausea, vomiting, bone marrow supression
|
|
|
Busulfan
|
Cell cycle nonspecific agent - alkylating agent
Cross links DNA and RNA stranfs Used in CML |
|
|
Side effects Busulfan
|
Pulmonary fibrosis and hyperpigmentation
|
|
|
Imantinib
|
Highly specific Bcr-Abl tyrosine kinase competitive inhibitor
Blocks proliferation, induces apoptosis in BCR-ABL positive cell lines and fresh leukemic cells Gleevec is well tolerated: side effect is fluid retnention 90% cytologic remission rate Dasatinib is second line |
|
|
CML to Blast Crisis
|
Progresses in 3-5 years to accelerated phase and then blast crisis, additional genetic abnormalities accumulate and lead to AML
Peripheral smear shows >20% blast cells |
|
|
Symptoms of AML
|
- low platelets lead to epistaxis and petechiae
- bone pain - anemia with dyspnea - gingivial hyperplasia (leukemic invasion) - leukemia cutis (skin infiltrates) - cellulitis is common presentation due to neutropenia bc of replacement of mature WBCs with leukemic cells leading to infections - Neurologic defects - DIC (more often in AML) |
|
|
DIC
|
Thrombohemorrhagic process with microthrombi throughout the body. Widespread activation of clotting leads to deficiency of clotting factors and leads to bleeding.
Consumes platelets so thrombocytopenia occur Decreased fibrinogen as converted to fibrin Increased D dimers (fibrin split products) - this is the most specific lab test due to activation of protein C and plasmin leading to fibrinolysis Prolonged coagulation labs with increased bleeding time, increased PT and increased PTT Occurs in the better prognosis AML t(15;17) which is FAB M3 acute promyelocytic leukemia because All-trans retinoic acid is effective treatment by inducing differentiation |
|
|
AML Characteristics
|
60-65 years
Poor prognosis in contrast to ALL Defect in maturation beyond myeloblast or promyelocyte state which appear on peripheral smear |
|
|
Stain for AML
|
Periodic acid-Schidd stain PAS - (negative) which distinguished from ALL which occurs most often in children
|
|
|
AML: microscopy
|
Auer rods: peroxidase positive cytoplasmic inclusions in granulocytes and myeloblasts
|
|
|
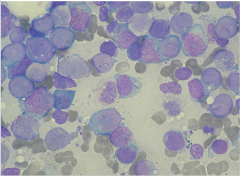
Auer rods
|
|
|
Genetics of Acute Promyelocytic Leukemia
|
t(15;17) translocation is a feature of acute promyelocytic leukemia
All-trans retinoic acid for treatment, vitamin A induces differentiation Release of Auer rods leads to DIC disseminated intravascular coagulation |
|
|
Methotrexate
|
S phase specific antimetabolite - folic acid analog- decreases dTMP, decreases DNA and protein synthesis; immunosupressant
|
|
|
Indication for Methotrexate
|
AML, bone marrow transplant for abortion, ectopic pregnancy, rheumatoid arthritis and psoriasis
|
|
|
Side effects of Methotrexate
|
Oral and GI ulceration, megaloblastic anemia immunosuppression, thrombocytopenia, leukopenia, fibrotic lung disease, mucositis, hepatotoxicity
|
|
|
Leucovorin "rescue"
|
Given as adjuvant after treatment to reverse myelosuppression
|
|
|
Cytarabine (ara-C)
|
S phase specific antimetabolite, pyrimidine analog that inhibits DNA polymerase
Used in AML |
|
|
Side effects of cytarabine
|
Leukopenia, thrombocytopenia, megaloblastic anemia
|
|
|
Granulocyte Colony Stimulating Factor
|
Aldesleukin human recombinant interleukin-2 can be used in AML
Filgramstim or Sargramostim granulocyte-macrophage stimulating factor for recovery of bone marrow during chemo induced neutropenia |
|
|
Graft vs. Host Disease
|
- Caused by donor lymphocytes attacking recipient cells
- Seen in non-autologous bone marrow transplants - Most common sites liver (elevated LFTS), skin (severe rash), and GI (watery diarrhea) |
|
|
ALL
|
Acute Lymphoblastic Leukemia
<15 can spread to CNS and testes t(12;21) better prognosis but in general all variants very responsive to therapy PAS periodic acid-Schiff stain +positive |
|
|
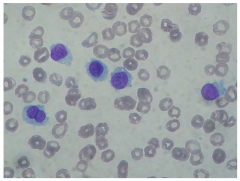
CLL
|
Chronic Lymphocytic Leukemia/Small lymphocytic lymphoma
age >60 smudge cells hepatosplenomegaly |
|
|
Hair cell leukemia
|
Stains TRAP positive
mature B cell tumor in elderly |
|
|
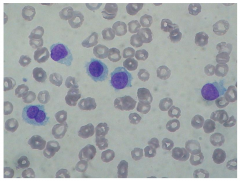
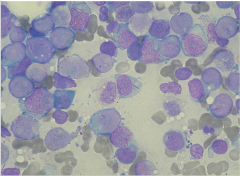
Hairy cell leukemia
|
|

|
|
|
|
|
|
|
Symptoms of Hyperthyroidism
|
1. Alertness, emotional lability, nervousness, irritability
2. Poor concentration 3.* muscular weakness, fatigability 4. palpitation 5. voracious appetite, weight loss* 6. increased frequency of bowel movements 7. heat intolerance |
|
|
Signs of hyperthyroidism
|
1. Hyperkinesia, rapid speech
2. Proximal muscle weakness, fine tremor 3. Fine, moist skin; fine, abundant air; onycholysis (separation of nail from its bed); pretibial skin thickening 4. Lid lag, stare, chemoisis, periorbital edema, proptosis 5. Accentuated first heart sound, tachycardia, afib, widened pulse pressure, dyspnea |
|
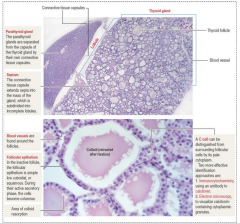
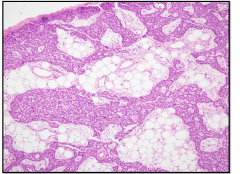
Normal Thyroid Histology
|

|
|
|
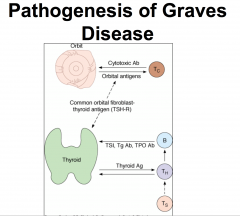
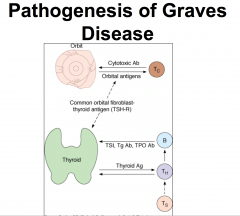
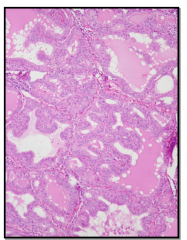
Graves Disease
|
Autoimmune
- diffuse involvement - microscopic appearance -- irregular follicles -- scalloped colloid |
|
|
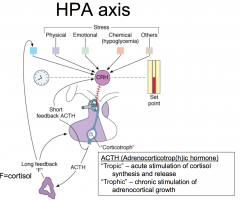
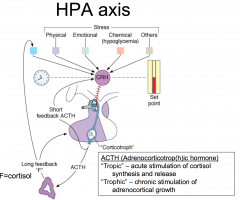
CRH stimulates ACTH - stimulate adrenal gland to produce cortisol... stress axis can by physical stress, chemical stress, or many other stresses .
|
|
|
Cortisol and Circadian Rhythm
|
|
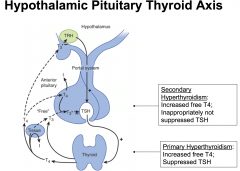
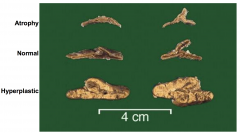
Adrenal Insufficiency: Primary adrenal insufficiency:
|
-destruction (usually irreversible) of the adrenal cortex (autoimmune; tuberculosis; adrenal hemorrhage)
Cortisol low; ACTH high (loss of negative feedback) Aldosterone low; renin high (loss of negative feedback) |
|

Secondary Adrenal Insufficiency
|

Chronically inadequate ACTH secretion resulting in loss of adrenocortical volume = adrenal atrophy
Cortisol low, ACTH inappropriately not increased Aldosterone and renin : usually unaffected |
|
|
Signs and symptoms of adrenal insufficiency
|
Fatigue, malaise, lack of energy
GI: nausea, vomiting, anorexia --> wt loss Hypotension ---> dizziness, orthostasis Increased skin pigmentation, salt craving (primary) WEAKNESS, FATIGUE, ANOREXIA, WEIGHT-LOSS |
|
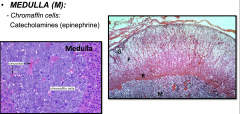
Histology and Physiology of the Adrenal Glands
|

- Zona glomerulosa : Mineralocorticoids = "salt"
- Zona fasciculata : Glucocorticoids = "sugar" - Zona reticularis : Estrogens and androgens = "Sex" |
|
|
|
|
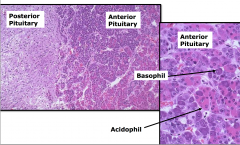
histology of pituitary gland
|
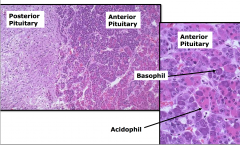
Anterior: secreting the horomones - acth, tsh etc.
made up of basophil and acidophil (primarily) |
|
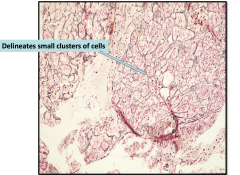
Anterior Pituitary Gland Architecture (reticulin stain)
|
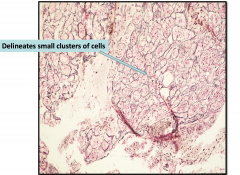
Reticulin network around lobules of normal glands - if it's gone means that you're having a proliferation of cells w/o normal architecture - pituitary adenoma
|
|
|
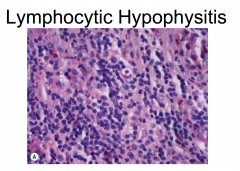
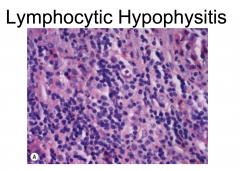
Autoimmune disorder classically affecting young women during late pregnancy or in the early postpartum period, mimics adenoma on neuroimaging and shows sheets of cytologically bland pure lymphocytic infiltrates.
|
|
|

|
|
|
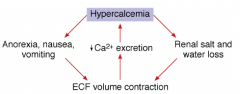
Symptoms of hypercalcemia
|
- Related to level and rate of change
- Fatigue, weakness - Nausea, vomiting, constipation - Anorexia - Polyuria, polydipsia - Dehydration - Memory impairment - Drowsiness, confusion, coma - Most ambulatory patients - no clear symptoms |
|
|

|
|
|
What causes hypercalcemia
|
Increase in PTH secretion
Primary hyperparathyroidism (usually a parathyroid adenoma) |
|
|
What does hypercalcemia result in?
|
Suppression of PTH secretion
Vit D intoxication, hypercalcemia of malignancy (caused by PTHrp) |
|
|
Primary hyperparathyroidism
|
Hypercalcemia; serum PTH inappropriately not suppresed (can have hypophosphatemia; high normal or increased calcium excreation)
- Sporadic (single and multiple gland disease, carcinoma) |
|
|
MENs associate with Primary hyperparathyroidism: MEN1
|
parathyroid, pituitary, pancreatic islet
|
|
|
MENs associate with Primary hyperparathyroidism: MEN2A
|
Parathyroid, pheochromocytoma, medullary carcinoma of the thyroid
|
|
|
MENs associate with Primary hyperparathyroidism: MEN2B
|
Medullary carcinoma, pheochromocytoma, neuromas/ganglioneuromas
|
|
|
PTH- Independent hypercalcemia : Malignancy
|
Bone metastases, PTH-related protein, osteoclast activating factors, unregulated calcitriol production, true ectopic PTH
Calcitriol-mediated (granulomatous, inflammatory) (calcitriol = 1,25(OH)2D) |
|
|
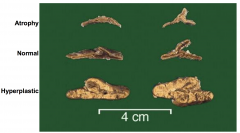
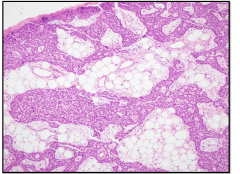
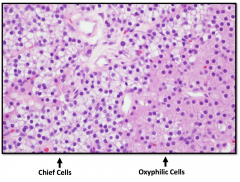
Characteristics of normal parathyroid
|
Yellow, brown ovoid nodule
30-45mg Composed primarily of chief cells and some oxyphil cells In adults there is a large amount of intervening stromal fat (30-70%) Chief cells secrete parathyroid hormone |
|
|
Normal Parathyroid Gland
|
|
|
|
|
|
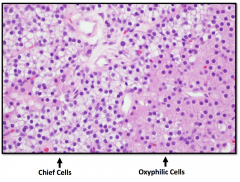
Parathyroid Adenoma
|
Solitary nodule arising in a single parathyroid gland
0.5 - 5.0 grams Other glands are either normal or atrophic Composed of sheets of chief cells with decrease in stromal fat Oxyphilic cells may also be present May show a rim of normal parathyroid at the periphery |
|
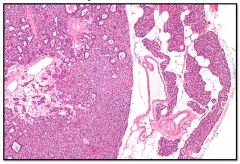
Parathyroid Adenoma
|
|
|
|
How is Graves disease best rules out?
|
By measuring a suppressed serum TSH (increase neg feedback inhibition of pituitary thyrotrophs)
|
|
|
Hashimoto shows?
|
Autoimmune condition
Show lymphocytic infiltration |
|
|
What does Graves show?
|
Autoimmune condition
Irregular follicular borders Scalloped colloid |
|
|
Adrenal Insufficiency
|
An ambulatory patient is best rules out with an ACTCH stimulation test (primary AI - adrenal destroyed; secondary AI - adrenal atrophied)
|
|
|
Adrenal cortical atrophy can be caused by
|
increased glucocorticoids, pituitary dysfunction (sheehan, panhypopituitarism), Addision disease (autoimmune destruction)
|
|
|
Mild hyperalcemia
|
Requires evaluation for possible primary hyperparathyroidism
|
|
|
Primary hyperparathyroidism
|
PTH is usually in the upper part of the reference range or increased
Hypercalciuria may be present because the filtered load of calcium has exceeded the Tm for calcium in the kidney |
|
|
Most common cause of primary hyperparathyroidism
|
Parathyroid adenoma
|

