![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
64 Cards in this Set
- Front
- Back
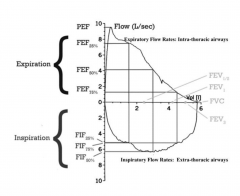
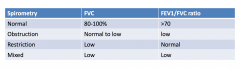
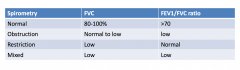
Flow volume Loop
|
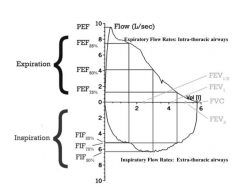
Shape of the loop tells us whether the person has normal breathing or not. Look at expiratory limb first. Look at the PEF and then the forced vital capacity (total amount of air that is blown out)
For dyspnea, pay attention to the inspiratory limb as well if you think there's an obstruction. |
|
|
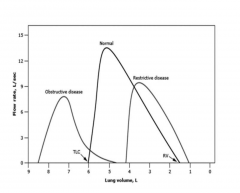
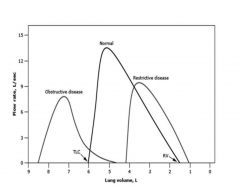
Restrictive Pattern - blowing out is normal, but the amount that they can blow out is smaller, because the amount they can hold in their lung is smaller due to fibrosis
|
|
|
RV
|
Tells us about air trapping. Tells us - if high - that the person has a barrel shaped chest with a huge amount of volume that is trapped.
|
|
|
|
|
|
Obstructive Ventilatory Pattern
|

Large conducting airways: tumors, foreign bodies
Peripheral airways: asthma, chronic bronchitis, cystic fibrosis Pulmonary parenchymal disease: emphysematous change from cigarette smoking |
|
|
Restrictive Ventilatory Defect
|
Interstitial lung disease: sarcoidosis, collagen vascular diseases, pulmonary fibrosis
Pneumonectomy Pleural disease: pleural effusion Chest wall disease: kyphosis, neuromuscular disorders Extrathoracic conditions: obesity |
|
|
Processes that result in decreased compliance of the lungs/chest wall will cause?
|
Restrictive pattern.
Compliance is a combination of lung and chest wall compliance |
|
|
|
|
|
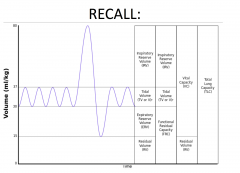
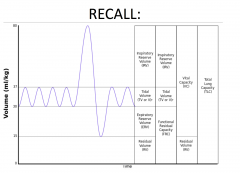
What is functional residual capacity?
|
The amount of volume left in the lungs at the end exhalation from tidal breathing
|
|
|
Diffusion: Key determinants
|
1. Surface area of the lung with contact to diffusing alveoli (VA - Alveolar Volume)
2. The thickness of the alveolar capillary membrane (Dm - Membrane Diffusion) 3. The volume of blood available in the capillary bed of the lung (Vc- Capillary Blood Volume) |
|
|
What's not associated with a low diffusing capacity?
|
Asthma
|
|
|
Causes of low diffusing capacity?
|
- Significant anemia
- Loss of parenchyma (like in emphysema) - Diseases that scar the lung such as pulmonary fibrosis or sarcoidosis - Swelling of lung tissue (pulmonary edema) due to heart failure or due to an acute inflammatory response to allergens (acute interstitial pneumonitis) - Diseases of the circulation in the lung, such as pulmonary vasculitis or pulmonary hypertension |
|
|
What elevates diffusing capacity?
|
Asthma
Alveolar hemorrhage (acute) Intracardiac shunt (left to right) Erthyrocytosis |
|
|
Chronic Obstructive Pulmonary Disease
|
Emphysema
Chronic Bronchitis Bronchiectasis Chronic persistent asthma (FEV1 remains abnormal after therapy) |
|
|
Emphysema
|

Irritants active macrophages and epithelial cells to release chemotactic factors that lead to recruitment to the area with more macrophages and neutrophils
Proteases are released that destroy structural elements in the lungs Highly reactive oxygen species (superoxide, hydroxyl free radical, and hydrogen peroxide) contribute to destructive power of the proteases leading to breakdown of alveolar units and emphysema develops |
|
|
Centriacinar Emphysema
|
Proximal part of acinus, respiratory bronchiole affected
Proximal airways = anthracosis (smoking) + lympho-plasmacytic inflammatory infiltrate Upper lobes of smokers may also see chronic bronchitis and bronchiolitis |
|
|
Panacinar Emphysema
|
Destruction involving the entire respiratory unit (respiratory bronchiole - alveoli)
Lower lobes of those with alpha-1 antitrypsin deficiency Associated with hepatitis + cirrhosis |
|
|
Paraseptal Emphysema
|
Distal destruction/ enlargement of the alveoli
Upper lobe, subpleural location (bullous change) Predisposes to spontaneous pneumothorax Patchy distribution of parenchymal injury and +/- pulmonary scarring |
|
|
What does emphysema lead to?
|
It leads to loss of elastic recoil and dynamic airway collapse as a result of loss of structural support in the smaller noncartilaginous airways. As the lungs expand, they stretch the chest wall and place the diaphragm at mechanical disadvantage and the upper chest wall muscles must now assist in breathing.
These are the pink puffers - and they will eventually become hypoxic -- but that's in the later stages |
|
|
With emphysema, what happens as more alveoli are lost?
|
More mismatched ventilation perfusion and deadspace develop with eventual hypoxemia and hypercapnia
|
|
|
How is deadspace calculated?
|
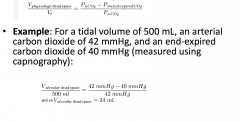
|
|
|
What is the genotype associated with Panacinar Emphysema?
|
ZZ
|
|
|
What are the genetics of emphysema
|
Alpha-1 antitrypsin deficiency
- autosomal recessive - MM is normal phenotype - ZZ homozygous (panacinar emphysema) - Should screen all patients with obstructive lung disease - Replacement therapy can stabilize function if no longer smoking |
|
|
Pathogenesis of Chronic Bronchitis
|
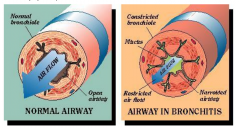
Inhaled smoke or other respiratory irritants or abnormal mucous due to or resulting in recurrent bacterial infection --> mucous hypersecretion in bronchi --> air flow obstruction in terminal bronchioles (more proximal than emphysema) --> irreversible fibrosis of terminal bronchioles
|
|
|
Chronic Bronchitis
|
Subtype of COPD
Productive cough for at least 3 months for 2 consecutive years Causes: - Smoking - Chronic exposure to respiratory irritants (pollution, work related) - Cystic fibrosis - Infection --- maintenance of disease --- acute exacerbations |
|
|
Clinical findings of bronchitis
|
Productive cough
Cyanosis "Blue bloater" Dyspnea Expiratory wheezing and rhonchi Cor pulmonale (strain on RT heart) Clubbin |
|
|
CXR of Bronchitis
|
Enlarged heart, horizontally oriented
Increased bronchial markings Increased mucous glands |
|
|
Pathogenesis of cystic fibrosis
|
Mutations affect the composition of the mucus layer lining the epithelial surfaces in the lungs and pancreas. The disruption of ion transport affects the salt conc in sweat.
Chloride ion transport is affected -- water does not come in with Cl- resulting in a very viscous mucuous |
|
|
Term used to describe microscopic changes in chronic bronchitis
|
Reid Index
|
|
|
Reid Index
|
Ratio of the thickness of the mucous gland layer to the thickness of the wall between the epithelium and cartilage (Normal is < 0.4).
|
|
|
Bode Index
|
Used for prognosis of COPD
|
|
|
COPD Treatment
|
Bronchodilators
- relax smooth muscle bronchoconstriction, increased cilia beat frequency Anticholinergics - blocks muscarinic receptors, preventing bronchoconstriction, decreased mucous production Inhaled Corticosteroids - may decrease exacerbation Oxygen Therapy - may decrease mortality in cor pulmonale |
|
|
Chest pain radiating to neck or arm. Diaphoresis. Nausea
|
Angina
|
|
|
Chronic cough, tobacco history
|
COPD
|
|
|
Orthopnea, Paroxysmal Nocturnal Dyspnea, Leg Swelling
|
CHF
|
|
|
Clinical history of COPD
|
Older age, tobacco exposure, diurnal variation not present
|
|
|
Clinical history of asthma
|
Younger age, allergens, family hx, worsen early morning and night time
|
|
|
Tests : Spirometry
Diffusing Capacity CXR COPD |
Obstruction not fully reversible
Reduced Hyperinflation, bullous changes |
|
|
Tests : Spirometry
Diffusing Capacity CXR Asthma |
Fully reversible obstruction
Normal or increased Normal to hyperinflated |
|
|
Pathology of COPD
|
Mucous gland metaplasia
Loss of alveolar tissue |
|
|
Pathology of Asthma
|
Mucous gland hyperplasia, intact alveolar structures
|
|
|
Inflammation of COPD
|
Macrophages and neutrophils ++
CD8+ lymphocytes |
|
|
Inflammation of Asthma
|
Mast cells and eosinophils ++
CD4+ lymphocytes |
|
|
Treatment COPD
|
Inhaled corticosteroids for moderate to severe disease
Leukotriene inhibitors not recommended Anticholinergics are for maintenance and exaccerbations |
|
|
Treatment of Asthma
|
Inhaled corticosteroids for mild to severe persistent disease
Leukotriene Inhibitor is used as a controller Anticholinergics may benefit in exacerbations |
|
|
What defines reversibility
|
Increase in FEV1 by 12% and 200 mL
|
|
|
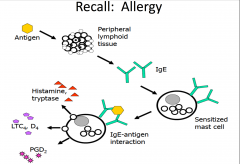
In allergy skin testing, what antibody are you detecting?
|
IgE
|
|
|
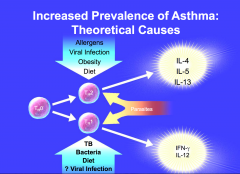
Asthma
|
Complex clinical syndrome characterized by variable airflow obstruction, airway inflammation, bronchial hyperresponsiveness
|
|
|
Why do asthmatics get nocturnal cough?
|
Cooling of airway
Lower levels of endogenous epinephrine and cortisol |
|
|
|
|
|
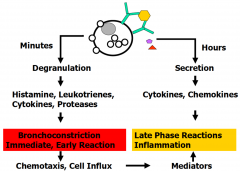
Pathophysiology of Asthma
|
Persistent inflammation
- Infiltration of airway by inflammatory cells - Hypertrophy of airway smooth muscle - Thickening of basement membrane - Hyperplasia and Hypertrophy of submucosal glands - Goblet cell hyperplasia and hypertrophy - Hyperplasia of microvascular dilation - Loss of epithelial cells |
|
|
Predominant and characteristic cell seen in airways of asthma inflammation
|
Eosinophil
|
|
|
Finding in sputum of asthma
|
Charcot-Leyden Crystals
|
|
|
Asthma Triggers
|
Allergic
-- pollen, mold, pet dander Viral Respiratory Infections -- RSV, rhinovirus Exercise Aspirin Irritants -- smoke, perfume, pollution Weather Changes -- cold air, humidity |
|
|
|
|
|
|
|
|
How does exercise trigger asthma?
|
Cooler, drier air causes release of bronchoconstrictor mediators from airway mast cells
- cysLTs (LTC4, LTD4) and histamine |
|
|
Aspiring and Asthma
|
Smooth muscle contraction
Bronchial constriction Increased vascular permeability Increased mucous production |
|
|
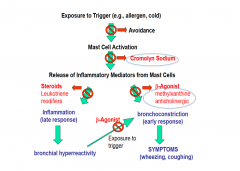
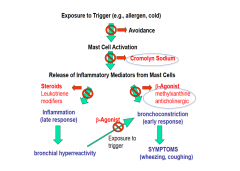
How do you treat asthma?
|
Avoidance of triggers
- Pollen : stay inside - Mold: repair water leaks - Pets: bathe frequently, keep out of bedroom - Cockroach : exterminate - Dust mites : encasing over bedding |
|
|
Asthma medication that leads to the synthesis of anti-inflammatory proteins
|
Beclomethasone
|
|
|
Which receptor does albuterol bind?
|
Beta 2
|
|
|
Beta Agonist for Asthma
|
Relaxes airway smooth muscle
Improves mucociliary function Short-acting: as needed Long-acting: use in combination with inhaled steroid |
|
|
Medication that is helpful in aspirin exacerbated asthma
|
Leukotriene modifier
|
|
|
|

