![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
-Algia
|
Pain
|
|
|
Arthralgia
|
Pain without objective joint finding (thousand of causes)
|
|
|
Arthritis
|
Diagnosis of arthritis demands an objective finding.
Most commonly a physical finding. Sometimes a radiographical finding. Sometime it's a joint fluid abnormality |
|
|
Exam for arthritis
|
Look for:
Swelling (tumor) Warmth Erythema Tenderness accentuated over joint Decreased range of motion |
|
|
Eliciting Tenderness
|
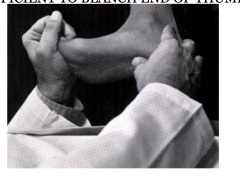
Sufficient to blanch end of thumbnail
|
|
|
Feeling for warmth with joints
|
Use back of hand. Compare to adjacent and contralateral structures.
|
|
|
Physical exam hints for joint pain
|
- A normal control might be the opposite side or adjacent similar joint
- Another normal control is you - intra-articular problems often restrict passive and active ROM (use joint during any ROM) - extra- articular problems restrict active or resisted and relative spare passive ROM (use muscles and tendons) |
|
|
Non-Inflammatory arthritis (osteoarthritis)
|
Tender, swelling often bony rather than soft
Joint fluid WBC > 200 but < 2000 Usually normal acute phase reactants sclerosis, narrowing, or normal on x-ray |
|
|
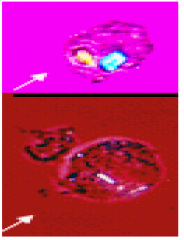
Inflammatory (rheumatoid arthritis)
|
Prominent inflammation
Soft tissue swelling Joint fluid WBC > 2000/MM3 Usually elevated acute phase reactants Porosis, narrowing, and/or erosions on x-ray |
|
|
Symptoms suggesting an "inflammatory arthritis"
|
Pain is similar in severity to "non-inflammatory"
Pain improves with activity, better late in day (non-inflammatory worsens) Morning stiffness > 30 min Subjective swelling usually more prominent in inflammatory |
|
|
2 Common Arthritis Presentations
|
Acute Monoarthritis (one joint)
Chronic polyarthritis |
|
|
Acute inflammatory monoarthritis
|
Three common causes:
- Inflammatory causes: .. crystal induced ( gout or pseudogout) .. septic ... acute non-inflammatory cause (trauma) |
|
|
Crystals associated with gout
|
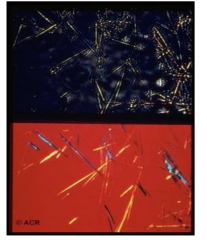
Monosodium urate crystals
|
|

|
Calcium pyrophosphate dihydrate crystals
- pseudogout |
|
|
Aspirate Joint Fluid
|
- Categorizes inflammatory vs. Non-inflammatory (WBC 2,000)
- Only way to confidently diagnose crystal-induced arthritis - Can't afford to miss a septic joint due to potential for rapid destruction w/o early intervention |
|
|
Chronic Inflammatory polyarthritis
|
- Rheumatoid Arthritis
-- mostly peripheral joints -- some systemic features (fatigue, anemia) - Connective Tissue Disease -- prominent extra-articular features (skin, renal, lung, etc.) e.g. - lupus, scleroderma - Spondyloarthropathies -- often spine and attachment structures inflamed (ligament, tendon, capsule, periosteum) as well as joint |
|

|

|
|
|
Arthritis
|
An objective finding by physical exam, direct visualization (surgery or arthroscopy), or by radiographic demonstration of joint damage
- Not merely subjective joint pain - Not an abnormal blood test - Is suggested by some typical symptoms, especially prolonged morning stiffness, history of swelling, loss of motion |
|
|
Acute Monoarthritis
|
Think crystals (inflammatory), infection (inflammatory), or trauma
Aspirate fluid if suspect inflammatory |
|
|
Chronic Inflammatory Polyarthritis
|
Think RA, Connective Tissue Disease, Enthesopathy
- Consider if primarily joints (RA), joints + other organs (CTD), joints + entheses or spine findings (enthesopathy, spondyloarthritis) Many clues in extra-articular symptoms and signs, clues in lab, and clues in x-ray indicate specific diagnosis |
|

|

|
|

|

|
|
|
Juvenile Idiopathic Arthritis
|
Systemic:
- 1-2x daily fever spike - ecanescent rash Psoriatic |
|
|
Polyarticular
|
- more than 4 joints at presentation
- RF+ - RF- |
|
|
Oligoarticular
|
4 or fewer joints at presentation
|
|
|
Juvenile Idiopathic Arthritis - Enthesitis-related arthritis
|
Inflammation at tendinous inertions "enthesitis" or tendon sheaths
- axial involvement (spine, SI joints) - larger peripheral joints - acute anterior uveitis |
|
|
NSAIDs
|
Inhibit Cox1/2
Cox1- housekeeping Cox2- inflammation |
|
|
COX1
|
"housekeeping"
GI protection (gastritis) Renal blood flow (renal insufficiency) Platelet aggregation Vasoconstriction |
|
|
COX2
|
Inflammatory
Central mediation of pain/fever Vasodilation |
|
|
NASIDS and CV Risk
|
ASA irreversibly inhibits COX
- platelets cannot regenerate - other nucleated cells (including endothelial cells and vascular smooth muscle can) - Net effects, platelets permanently inhibited, endothelium transiently inhibited COX2 Inhibitors - COX2 more active in endothelial cells but not as much as in platelets |
|
|
Glucocorticoids
|
Effects on gene transcription - hours
- binds to steroid receptor allowing translocation to nucleus to either activate or repress transcription of genes "nongenomic effects" - direct effects on -- signaling molecules -- ion channels -- can happen in minutes |
|
|
Immunosuppressive Effects of Glucocorticoiuds
|
Decreases expression of COX2
Decreases circulating lymphocytes by 70% -- especially CD4's but also CD8's and B cells -- likely by sequestration in bone marrow -- decreased proliferative responses 90% decrease in circulating monocytes Reduces chemotaxis of neutrophils to inflammatory sites -- may raise blood neutrophil count ("demargination") --paradoxical increase in neutrophils |
|
|
Side Effects of Steroids
|
- Immune suppression
- HTN (steroids increase absorption of salt) - Osteoporosis, poor growth - Increased hunger, centripetal obesity, buffalo hump, moon facies - Striae - Psychiatric (mania, depression, psychosis, sleep disturbance) - Reversible adrenal insufficiency (need to wean steroids gradually) |
|
|
Methotrexate
|
Inhibition of DNA Synthesis
-- inhibits recycling of dihydrofolate reductase which is necessary for recycling of DHF to THF -- THF is necessary for purine and pyrimidine synthesis -- This is major action in high dose uses for cancer Increases levels of immunomodulatory adenosine -- this is likely the major action for low dose uses for autoimmune diseases |
|
|
Methotrexate Effects
|
Effects are dependent on polyglutamation
- prevents efflux of MTX from cells |
|
|
Indications for Methotrexate
|
- Leukemia/lymphoma
- Rheumatoid arthritis - Inflammatory bowel disease - Psoriasis |
|
|
Side Effects of Methotrexate
|
GI mucosa- nausea, mucositis
Bone marrow - anemia, other cytopenias Liver - hepatitis Lungs - hypersenstivity pneumonitis Renal - 90% renal clearance, high dose can cause renal insufficiency |
|
|
Tumor Necrosis Factor
|
Initially synthesized as membrane bound trimer
Released in soluble form by TNF-alpha converting enzyme Important role in control of granulomatous infections |
|
|
TNF sites of action
|
Produced largely by macrophages and CD4 T cells
Important role in control of granulomatous infections |
|
|
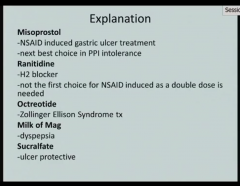
Patient complains of abdominal pain when using naproxen. What mediation do you use instead?
|
Celecoxib. It is a selective Cox-2 inhibitor.
|
|
|
Anti-TNF : Mechanism
|
Inhibits signaling through TNF-receptor
Antibody dependent cell cytotoxicity of tmTNF expressing cells (less so with etanercept) Potentially reverse signaling through thTNF itself |
|
|
Anti-TNF: Indications
|
Inflammatory bowel disease
RA/JIA Psoriasis |
|
|
Anti-TNF : Side Effects
|
- Infection - particularly infections controlled by granulomas (TB, histoplasma)
- Controversial increase in malignancies - Can develop antibodies to mouse portions of drug -- infusion reactions -- reduced efficacy - Neuropathies - Autoantibodies/autoimmunity |
|
|
NSAIDs block?
|
Cox1/Cox2
Includes: aspirin, ibuprofen and naproxen (acetaminophen) is not considered an NSAID because it has little anti-inflammatory activity selective cox-2 inhibitor is celecoxib |
|

|

|
|
|

|
|

|

|
|

|

|
|

|

|

