![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
Stage 1 CKD
|
GFR > 90 with renal damage as evident by proteinuria
|
|
|
Stage 2 CKD
|
GFR 60-89
|
|
|
Stage 3 CKD
|
GFR 30-59 (A and B)
|
|
|
Stage 4 CKD
|
GFR 15-29
|
|
|
Stage 5 CKD
|
GFR < 15
|
|
|
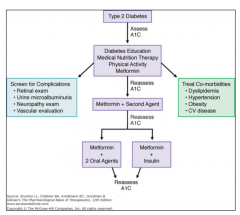
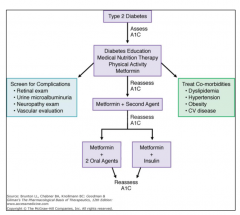
Pt was diagnosed with type 2 Diabetes
Mellitus 10 years ago. At that point he was on oral hypoglycemic drugs. Now he presents with main complaint of leg swelling and polyuria. On Exam he is 5’11”, 278 lbs, temp 37, RR 17, pulse 98, BP 167/102. Lungs are clear on auscultation. He has 3+ LE edema bilateral and symmetrical. Most likely cause of LE edema? |
Kidney disease complications of DM
Although DVT is plausible, it is unlikely because the edema is bilateral. |
|
|
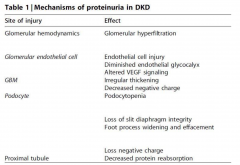
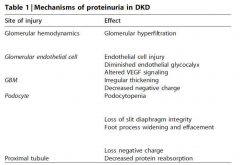
Diabetic Nephropathy
|
Among the leading cause of nephrotic syndrome which have a constellation of features: Proteinuria (>3/5g/24hr), hypoalbuinemia, hyperlipidemia and edema. The edema is caused by volume retention (salt retaining nephrons) and low oncotic pressure caused by hypoalbuminemia.
|
|
|
|
|
|
|
|
|
On further interview he said that he is get tired and
wants to lay down during the day especially after he takes his meds in the morning. His current medications are metformin, clonidine, glyburide, and Lasix. What are the possible cause(s) of his fatigue? A. Hypoglycemia B. Obstructive sleep apnea C. Hypotension D. TIAs |
Hypoglycemia
Hypotension |
|
|
|
|
|
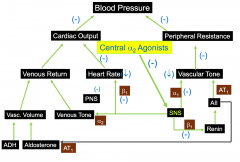
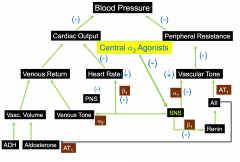
Central alpha 2 agonists
|
Clonidine
Guanabenz alpha-methyldopa Stimulate alpha2-adrenergic receptors in the brain - this reduces sympathetic outflow from the brains vasomotor center - increases vagal tone |
|

|

|
|
|
Central alpha 2 agonists: adverse effects
|
- sodium and water retention
- abrupt discontinuation may cause rebound htn - depression - orthostatic htn - dizziness clonidine can result in anticholinergic side effects methyldopa can cause hepatitis, hemolytic anemia (rare) |
|
|
With this patient what labs are necessary?
|
- Blood chemistry (BMP, HbA1C)
- Urine albumin/creatinine ratio - Lipids profile |
|
|
|
|
|
|
|
|
53 year old female with family history of
autosomal dominant polycystic kidney disease (ADPKD). She just moved from another state 10 month ago. She was told 14 years ago that she has polycystic kidney disease but nothing to be worried about yet. She was busy but now has to see someone because she noticed she has blood in the urine and she has right flank pain. Vitals: Temp 37°C, RR 16, Pulse 72, BP 176/105. Pt is only taking ibuprofen for headache. What is the most likely cause of her symptoms ? |
Kidney Stones
Ruptured Renal Cyst |
|
|
Renal Complications of Autosomal Dominant Polycystic Kidney Disease
|
Infection
Kidney Stones Hematuria Renal cell carcinoma is suspected when hematuria is recurrent or perisistent |
|
|
Diagnosis for PKD
|
1. Imaging technology of cysts in kidneys and other organs
2. Family medical history (genetic testing) |
|
|
|
|
|
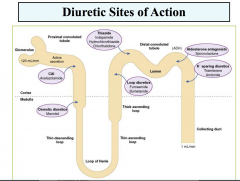
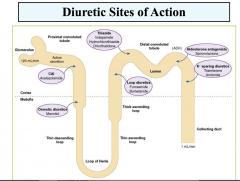
Ascending Limb Loop of Henle
|
- Sodium and chloride reabsorbed (20-30%): active chloride reabsorbed
- Impermeable to water: no water reabsorption - Can compensate for increased sodium delivery from proximal tubule by increasing reabsorption - Diuretic action on cortical and medullary segments differ in response |
|
|
Characteristics of Thiazide and Thiazide-like Diruectics
|
Orally active
Intermediate efficacy (8-10% of filtered sodium load excreted) Moderate onset of activity (60 min) Long duration of action |
|
|
Mechanism of action of thiazide diuretics
|
Filtered and secreted by the OAT
Inhibits Na-Cl symporter Acts on cortical segment of distal tubule Increases the excretion of sodium, potassium, chloride and water Urine is hypertonic – unable to dilute Increases potassium secretion Enhances urate reabsorption |
|
|
Disadvantages of thiazide diuretics
|
Hypokalemia
Alkalosis Hyperuricemia Hyperglycemia Decrease in GFR with thiazies |
|
|
Uses of thiazide diuretics
|
Edema due to CHF
Hypertension Hyeprcalciuria/Ca salt - renal caliculi |
|
|
Loop Diuretics
|
Furosemide, Bumetanide, Ethacrynic Acid
|
|
|
Characteristics of Loop Diuretics
|
Orally and IV active
High efficacy (20-30% of filtered sodium load excreted) Rapid in onset (20-30min) Short duration of action |
|
|
Mechanism of Loop Diuretics
|
Filtered and secreted by OAT
Inhibits Na-K-2Cl symporter Acts on the cortical and medullary segments of the ascending limb of the loop of Henle Increase the excretion of sodium, potassium, chloride, and water |
|
|
Actions of Loop Diuretics?
|
Increases renal blood flow and GFR
Enhances calcium excretion Large urine volume |
|
|
Disadvantages and side effects of Loop Diuretics
|
Hypokalemia
Alkalosis Hypovolemia Hyperuricemia (urate reabsorption - PT) Hyperglycemia - furosemise Otoxicity |
|
|
Uses of Loop Diuretics
|
Edema of cardiac, hepatic or renal origin
Acute pulmonary edema HTN |
|
|
|
|
|
Patient has the following:
Blood chemistry come back showing – eGFR 18 – Ca 7.1 – Hemoglobin 8.5 – PO4 7.8 – PTH 328 What should you give them? |
Erythropoietin
Calcitriol Phosphate binders |
|
|
Tolvaptan
|
Vasopressin receptor 2 antagonism
Was designed to treat hyponatremia cAMP carry out the signal of V2 receptor In PKD cAMP also stimulates cystogensis and increase the size of cysts Drug gas been shown to reduce cyst growth |
|
|
Main complications of Tolvaptan
|
One of the main complications is volume loss
|
|
|
What is the likely chemical changes seen on BMP on first blood draw in ER with Tolvaptan
|
- Creatine
- Sodium - BUN |
|
|
Creatinine goes up when GFR goes down.
Why? |
Decreased kidney function leads to a decreased ability in creatinine clearance
|
|
|
Pt decided to withdraw from the clinical trial. eGFR is
stable. Two month later she calls your office and said she has the worst headache of her life. What should the advice be? |
Call 911 or go to nearest ER
|
|
|
Extra-renal complications of ADPKD?
|
Intracranial aneurysm: 5-7% of adults with ADPKD may
have brain aneurysm and up to 12-15% if another family member had an intracranial aneurysm. (5x higher than general population) • Liver cysts: >85 percent of patients will have liver cysts by age 30. • Heart valve disease: 25% of patients with ADPKD. Usually require no treatment but can become severe enough to require valve replacement. • Abdominal wall hernias: 45 % of patients with ADPKD. |
|
|
A 45-year-old morbidly obese Caucasian woman
comes to your office for the first time to establish care. She has not seen a doctor in years and complains only of wanting to lose weight. The patient takes no medications and has no significant past medical history. Her parents are both living and healthy. Her blood pressure is 145/88mm Hg and BMI is 40.5. The remainder of her exam is normal. You order a fasting lipid profile, basic serum chemistry panel, urinalysis, and electrocardiogram. Regarding her obesity and risk for kidney disease, what information will you give her? |
Obesity may cause proteinuria
|
|
|
Obesity-associated glomerulosclerosis
|
form of hyperfiltration nephropathy, in which hemodynamic changes associated with obesity lead to progressive renal scarring, decline in glomerular
filtration rate, and proteinuria. It is a known entity, whose incidence is rising with the epidemic of obesity in the United States |
|
|
Obesity leads to hypertension via
|
increased peripheral resistance and an increase in cardiac output, increased sympathetic tone and increased salt sensitivity(Kasper).
|
|
|
The patient is a 52-year-old male with polycystic kidney disease. Despite a strict diet, his symptoms of fatigue, pruritus, and headache recently have gotten worse, and he has episodes of hematuria and urinary tract infections almost every month. He has gained several pounds during the last week despite a low appetite. On examination, patient is edematous, has uremic fetor, sallow colored skin with "uremic
frost," and slightly icteric sclera. His blood pressure is 190/120. Laboratory shows normochromic normocytic anemia, metabolic acidosis, and the imbalance of potassium, sodium, and chlorides, with increased levels of calcium, phosphate, and magnesium, and with reduced bicarbonate. Blood urea nitrogen (BUN) and creatinine levels are elevated. Urinalysis reveals the presence of proteinuria, hematuria, bacteriuria, and leucocyturia. His glomerular filtration rate (GFR) is 14 mL/min/1.73 square meters. This patient should start dialysis. What should also be administered? |
Erthropoietin
|
|
|
Best medication for lowering the BP of a morbidly obese woman with diabetes?
|
ACE-I
|
|
|
A 45-year-old white female comes for her annual
checkup. She has been seen regularly over the last 10 years. She has had Adult Onset Diabetes for the past 10 years. Her weight is 205 pounds at a height of 5 feet 1 inch. She is unsuccessful in losing weight. Her blood pressure is 170/95, temperature is 97.6 F, and heart rate is 82. High blood pressure and diabetes are the most common cause of end-stage renal disease in the United States. In a normal kidney when the blood pressure reaches >150 mmHg the body's ability to auto regulate glomerular capillary pressure will start to fail. In talking with the client, you explain that her blood pressure should be optimally below 127/75. What is causing his polyuria? |
Nephrogenic diabetes insipidus
lithium impairs the distal water reabsorption, mediated by vasopressin (ADH), leading to the production of large quantities of dilute urine. Unfortunately, lithium use, even for as short a period as 1 year, can lead to irreversible damage of the tubules (via down-regulation and production of receptors and channels responsible for water reabsorption). |
|
|
Treatments for lithium-induced nephrogenic diabetes
insipidus include |
amiloride, a distal-tubule acting diuretic which competes with lithium for access to ion channels and thus prevents the lithium-induced polyuria,
and B) hydrochlorothiazide with a low-salt diet, in order to effectively decrease the quantity of urine produced. Depakote can be substituted for lithium, but as mentioned above, lithium may cause irreversible tubular damage |
|
|
Central Diabetes Insipidus
|
amiloride, a distal-tubule acting diuretic which competes with lithium for access to ion channels and thus prevents the lithium-induced polyuria,
and B) hydrochlorothiazide with a low-salt diet, in order to effectively decrease the quantity of urine produced. Depakote can be substituted for lithium, but as mentioned above, lithium may cause irreversible tubular damage |
|

|

|
|
|
A 59-year-old African American man with a past medical history of hypertension, benign prostatic hypertrophy, type II diabetes mellitus for the past 15 years, and chronic back pain presents to the hospital with gross hematuria. The patient states that he noticed blood in his urine last night. The patient also reports mild, intermittent flank pain. The patient states that his diabetes and blood pressure are well controlled with medications, and that he has managed his chronic back pain with 2 aspirin per
day for the past 4 years. Vital signs are Temp- 98.6°F, BP- 124/82 mm/Hg, pulse- 88/min, and RR- 14/min. Blood work is notable for HbA1C of 6.5%. A pyelogram reveals a ring sign. His current fasting glucose is 140mmol/L. Most likely cause of hematuria? |
Analgesic Nephropathy
|
|
|
Analgesic Nephropathy
|
The fact that this patient has been taking aspirin regularly for the past 4 years puts him at great risk for analgesic nephropathy. These patients occasionally present with gross hematuria.
|
|
|
A 60-year-old man presents to the emergency room with severe, tearing pain radiating to the upper back. Over a period of hours, the pain moves to the mid back and then involves both flanks. Hematuria develops shortly thereafter. What renal complication is likely associated with the patient's symptoms?
|
Bilateral renal infarction
|
|
|
Bilateral Renal Infarction can result in?
|
Dissecting aortic aneurysm that occluded the renal arteries, causing bilateral renal infarction with flank pain and hematuria. This is a very dangerous complication of dissecting aortic aneurysm
|
|
|
Acute glomerulonephritis
|
characterized by hematuria, red cell casts, and often proteinuria and edema. This syndrome typically develops over days, not hours, and would not be expected to result from dissecting aortic aneurysm.
|
|
|
Polycystic kidney disease
|
Lifelong condition characterized by bilateral polycystic changes in the kidneys. It is associated with hypertension and eventual renal failure.
|
|
|
Polynephritis
|
infection of the kidney that can develop as a complication of bacterial endocarditis, or as a consequence of vesicoureteral reflux, but would not be expected to result from aortic dissection.
|
|
|
Sickle Cell Crisis
|
can cause papillary necrosis of the kidneys with hematuria, but there is no indication that the patient has sickle cell anemia.
|

