![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
158 Cards in this Set
- Front
- Back
|
Red Flags associated with a headache
|
- First or worst
- abrupt onset - pattern change - new headache pattern when <= 5 or >= 50 - cancer, HIV, pregnancy - abnormal physical exam - neuro symptoms >= 1 hour - headache onset with seizure or syncope or with exertion, sex, valsalva |
|
|
Comfort Signs associated with a headache
|
- Stable pattern
- Long-standing history - Family history of similar headaches - Normal physical exam - Consistently triggered by hormonal cycle, specific foods, specific sensory input (light, odors) - Weather changes |
|
|
Primary Headache
|
- Headache is idiopathic
- No identifiable underlying pathology - No diagnostic test - Defined by clinical symptomatology - Diagnosis based on ruling out pathology |
|
|
Secondary Headache
|
- Headache is a symptom reflecting underlying pathology
- Diagnostic tests - Diagnosis based on defining pathology |
|
|
Causes of a primary headache
|
- Migraine
- Cluster - Tension-type |
|
|
Causes of a secondary headache
|
- Trauma
- Vascular - Infection - Metabolic (CO Poisoning) - Oncologic - Inflammatory |
|
|
Pain sensitive intracranial structures
|
- Meningeal arteries
- Proximal portions of the cerebral arteries - Dura at the base of the brain - Venous sinuses - CN 5,7,9,10 and cervical nerves 1-3 |
|
|
Neuroimaging in a patient with a recurrent migraine
|
No CT or MRI except:
- recent change in pattern - new seizures - focal neurologic signs or symptoms |
|
|
Neuroimaging in a patient with a Nonmigraine headache
|
Role of CT or MRI is unclear, but some secondary headache causes may not be evident on CT
|
|
|
Common Diagnostic Tests in Headache
|
CBC
CMP Thyroid Panel Sedimentation Rate C-reactive protein Cervical spine x-ray Carotid Doppler Transcranial Doppler |
|
|
Cluster Headache
|
- Frequency of attacks: 1 every other day to 8 per day
- Severe - Unilateral orbital, supraorbital, and/or temporal location - lasts 15 to 180 minutes - can have associated symptoms (miosis, ptosis, rhinorrhea, nasal congestion) |
|
|
Horner's Syndrome in Cluster Headache
|
Cluster headaches may involve pain around one eye, along with drooping of the lid, tearing and congestion on the same side as the pain
|
|
|
Migraine without aura: diagnostic criteria
|
at least 5 attacks with:
- headache attach lasts 4 to 72 hours. No or inadequate Rx. - two of the following: unilateral location, pulsating quality, moderate or severe intensity, aggravation by walking up stairs or similar physical activity - one of the following (nausea, vomiting, photophobia and phonophobia) |
|
|
Best predictors of a diagnosis of migraine
|
Nausea, Disability, and Photophobia
|
|
|
Tension-Type Headache: Diagnostic Criteria
|
Headache occurring on approximately 15 days per month on average for greater than 3 months
- headache lasts hours or may be continuous - two of the following: (pressing/tightening, mild or moderate intensity, bilateral location, no aggravation by walking up stairs) - no more than 1 (photophobia, phonophobia, mild nausea, neither moderate or severe nausea nor vomiting) |
|
|
Tension Headache
|
- stress is an associated event
- location - tension headache as premonitory symptom - usually neck pain |
|
|
Sinus Headache
|
- location
- autonomic symptoms - weather as a trigger - nasal stuffiness and pressure |
|
|
Chronic Daily Headache : Risk Factors that are not readily modifiable
|
- migraine
- female - low education - low socioeconomic status - head injury |
|
|
Chronic Daily Headache : Risk Factors that are readily modifiable
|
- attack frequency
- obesity - medication overuse - stressful life events - snoring |
|
|
Cortical Neuronal Hyperexcitability: Multiple Mechanisms
|
- Enhanced release of excitatory neurotransmitters (elevated plasma glutamate conc. in patients with migraine)
- Identified genetic mutations in familial hemiplegic migraine (FHM) - Reduced intracortical inhibition - brain stays excited - low brain Mg2+ - altered brain energy metabolism |
|
|
Initiating Mechanisms of Headache Pain: Cortical Spreading Depression
|
- wave of intense cortical neuron activity (increased rCBF)
- followed by neuronal suppression (decreased rCBF, often coincides with headache onset) - velocity is 2-3 mm/min - underlies visual aura - associated with the release of arachidonic acid |
|
|
Initiating mechanisms of migraine: Brainstem Dysfunction
|
- Dysfunction in areas involved in central control of nociception (PAG)
- induction of migraine (brainstem generator) - Facilitates activation of sensitization of TNC neurons (decreased descending inhibition during a migraine attack) |
|
|
Serotonin Synthesis
|
- from tryptophan
- tryptophan hydroxylase is RLS - tryptophan conc. limits synthesis in brain (requires oxygen and reduced pteridine cofactor) - L-aromatic amino acid decarboxylase - similar enzyme used for catecholamine synthesis |
|
|
Metabolism and termination of action of serotonin
|
Metabolized to 5-hydroxyindole acetic acid by monoamine oxidase.
Neuronal action terminated primarily by a high affinity active uptake system (SERT) and then intraneuronal conversion to 5-hydroxyindole acetic acid. |
|
|
What is serotonin converted to?
|
Melatonin in the pineal gland
|
|
|
Location of serotonin
|
GI system - 90%
Platelets - 8% (no synthesis) CNS - 2% (cell bodies in midbrain raphe nuclei) |
|
|
Serotonin Receptors
|
- Most are GPCR
- 5HT1: inhibition of adenylate cyclase. 5-HT1A also opens K+ channel - 5HT2 - PI hydrolysis - 5HT3 - ligand gated cation channel - 5HT4-7: activation of adenylate cyclase or uknown |
|
|
How does serotonin affect the cardiovascular system
|
-potent vasoconstrictor of large arteries and veins; cranial (5HT1D) blood vessels
- Bezold-Jarish reflex: coronary chemoreceptors (bradycardia, hypotension, hypoventilation) - Platelet aggregation - active uptake of serotonin from circulation |
|
|
CNS Pharmacology with Serotonin
|
- Neurotransmitter - cell bodies in midbrain raphe nuclei - projects both rostrally and caudally
- May be involved in: sensory perception - LSD, sleep (slow wave deep sleep - not REM sleep), temp regulation, neuroendocrine regulation (release of ACTH, GH, prolactin, TSH, FSH, and LH) - learning and memory are particularly short term |
|
|
CNS Pharmacology - Serotonin - Pain Perception
|
Spinal and Brain sites of action
|
|
|
Emesis - serotonin
|
5HT3 receptors
|
|
|
Serotonin and Mental Illness
|
Affective Disorders - SSRIs and SNRIs
Schizophrenia - atypical antipsychotics OCD- SSRIs Anxiety -5HT1A receptors Aggressive Behavior |
|
|
Ondansetron
|
Nausea and Vomiting
|
|
|
Phenelzine
|
Depression
|
|
|
Fluoxetine
|
Depression
|
|
|
Cyproheptadine
|
Itch
|
|
|
Buspirone
|
Anxiety
|
|
|
Tegaserod
|
Constipation predominant IBS
|
|
|
Serotonin Agonisits (3)
|
1. Lysergic acid diethylamide
2. Buspirone 3. Sumatriptan |
|
|
Lysergic Acid Diethylamide
|
Relatively nonspecific 5HT2 receptor - potent hallucinogenic
|
|
|
Buspirone
|
5HT1A receptor partial agonist - antianxiety
|
|
|
Sumatriptan
|
5HT1B/D receptors on cerebral blood vessels.
Treatment of migraine headaches. Stops existing ones. |
|
|
Pharmacological Treatment of Migraine
|
Abortive Treatments
Migraine Prophylaxis |
|
|
Targets for Drug Action for Migraines
|
- Triptans (serotonin, CGRP, neurotranmission - trigeminal and cortical)
- Hormonal Manipulation (estrogen) - NSAIDs (prostaglandins) |
|
|
Triptans
|
Major class of drugs used to stop existing headaches
Serotonin 1B/1D agonists Inhibit release of vasoactive peptides - CGRP Promote vasoconstriction Block brainstem pain pathways Inhibit trigeminal nucleus caudalis |
|
|
Side effects of Triptans
|
Common Side effects:
- peripheral vasoconstriction - nausea and vomiting - angina - dizziness - flushing |
|
|
Contraindications associated with Triptans
|
Stroke and MI
Uncontrolled HTN, Ischemic Heart Disease |
|
|
Other abortive treatments for headaches
|
Ergots-DHE- ergotamine
NSAIDS with caffeine Steroids Butalbita/Caffeine/Acetaminophen = BAD CHOICE |
|
|
TCA
|
Amityrptyline, Nortriptyline (sedating, anticholinergice, effective for many pain sources)
|
|
|
Antiseizure Agents
|
Divalproex Sodium or Valproic Avid
Topiramate Others - gabapentin, pregabalin, lamotrigine |
|
|
Vasoactive Agents
|
Beta Blockers - Propranolol, Atenolol
CCBs- Verapamil, Diltiazem Variable efficacy - side effects |
|
|
General Principles of CNS Tumors
|
Both low and high grade neoplasms have significant morbidity and mortality (they are diffusely infiltrative, involve critical anatomical areas, and are not able to resected.)
Most of the time they do not spread outside the brain, but they may spread through the subarachnoid space |
|
|
Localization of CNS tumors (adult)
|
Localization of adult CNS tumors follows a mass distribution- most occur in the cerebral hemispheres, most frequently frontal lobes - as they are the largest
|
|
|
Localization of CNS tumors (child)
|
Occur in the posterior fossa (cerebellum or brainstem)
Intraspinal tumors are uncommon (in both adults and children) |
|
|
Astrocytomas
|
The most common glial tumor
Diffuse astrocytomas have an inherent tendency to be anaplastic over time |
|
|
Clinical Features of Astrocytomas
|
Seizures
Focal neurological deficits (gradual- not abrupt) Headaches |
|
|
Mean age of biopsy of Astrocytoma and median survival (years)
|
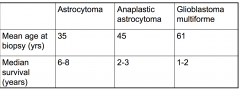
Mean age = 35
Survival = 6-8 yrs |
|
|
Mean age of biopsy of Anaplastic astrocytoma and median survival (years)
|
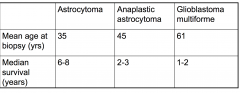
Mean age = 45
and Survival = 2-3 yrs |
|
|
Mean age of biopsy of Glioblsatoma multiforme and median survival (years)
|
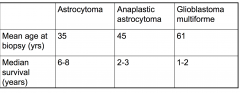
Mean age = 61
Median Survival = 1-2 yrs |
|
|
WHO Grading Scheme for Astrocytomas: Grade 1
|
Pilocytic astrocytoma (tends to not get worse)
|
|
|
WHO Grading Scheme for Astrocytomas: Grade 2
|
Astrocytoma (diffuse). Cellularity is moderately increased and occasional nuclear atypia
|
|
|
WHO Grading Scheme for Astrocytomas: Grade 3
|
Anaplastic astrocyoma - increased cellularity, distinct nuclear atypic, marked mitotic activity
|
|
|
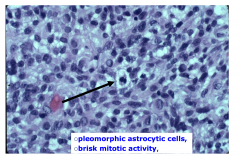
WHO Grading Scheme for Astrocytomas: Grade 4
|
Glioblastoma multiforme: Pleomorphic astrocytic cells, brisk mitotic activity, prominent micovascular proliferation and/or necrosis
|
|
|
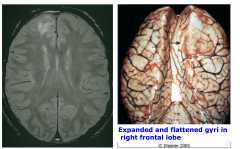
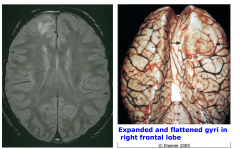
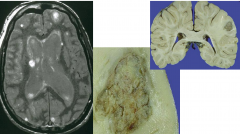
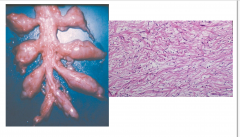
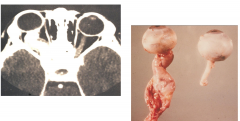
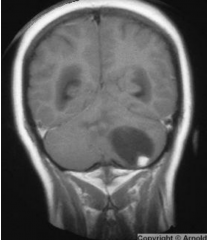
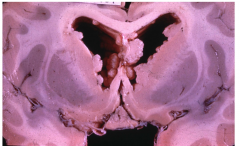
Astrocytoma, diffuse, WHO grade 2 MRI and gross brain.
There is expanded and flattened gyri in the right frontal lobe. Also edema |
|

|

Astrocytoma, diffuse, WHO grade 2
Tumor beyond corpus callosum Uncal herniation as well. |
|
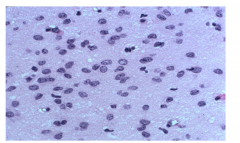
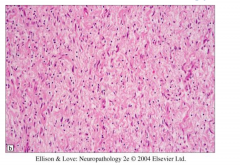
Pathology of WHO grade 2
|
Moderate increase in cellularity
Occasional nuclear atypia Increased nuclei, not much cytoplasm |
|
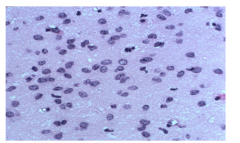
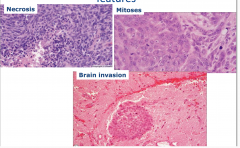
Anaplastic astrocytoma WHO grade 3 - Pathology
|
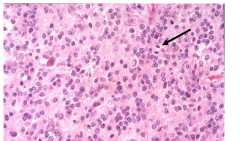
- further increased cellularity
- distinct nuclear atypia - marked mitotic activity |
|
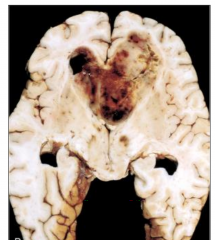
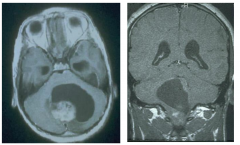
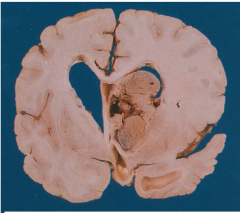
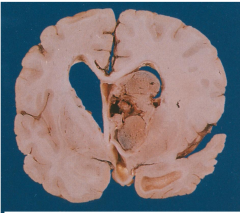
WHO Grade 4
|
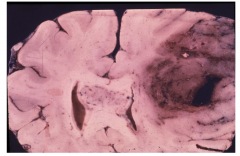
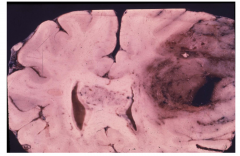
WHO Grade 4
A lot of necrosis and hemorrhage |
|
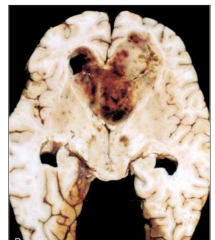
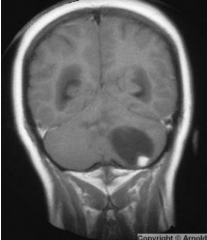
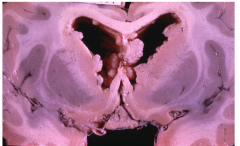
Glioblastoma multiforme WHO grade 4
|
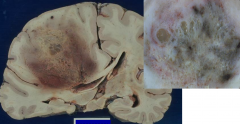
Glioblastoma multiforme WHO grade 4
Necrosis Subfalcine herniation |
|
|
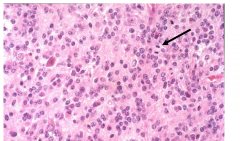
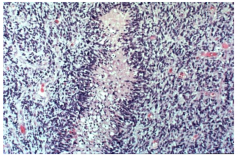
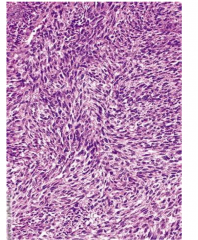
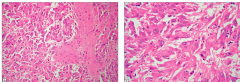
GBM: Necrosis with pseudopalisading
Tumor cells line up around necrosis Neoplastic cells migrating away from injury Lots of blue - cells are packed together and are hyperchromatic |
|
|
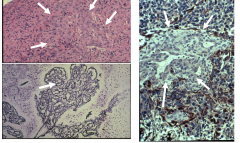
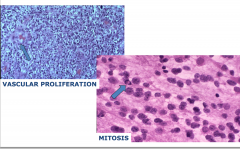
GBM - vascular proliferation
Clusters of endothelial cells Complex vascular network |
|
|
GBM - high power
- pleomorphic astrocytic cells - brisk mitotic activity |
|
|
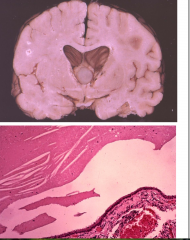
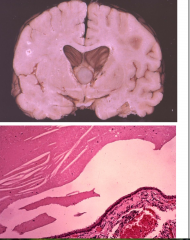
Pilocytic Astrocytoma
|
Most common glioma in children (usually in cerebellum or brainstem)
Typically present in 1st two decades |
|
|
Clinical Features of Pilocystic Astrocytoma
|
- Most commonly occur in cerebellum
- May also occur in optic nerve, 3rd ventricle, hypothalamus, brainstem, and occasionally cerebral hemisphere - Presentation with focal neurologic deficit, seizures, or S/S of increased intracranial pressure |
|
|
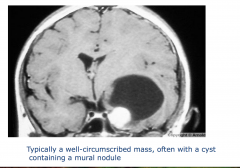
Imaging of Pilocystic Astrocytoma
|
Well demarcated, often cystic contrast-enhancing tumor. Some endothelial proliferation.
|
|
|
Prognosis of Pilocystic Astrocytoma
|
- Slow growing
- Overall excellent prognosis; surgery is often curative |
|
|
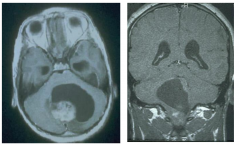
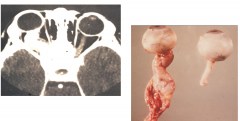
Pilocystic astrocytoma MRIs
characteristic cyst. |
|
|
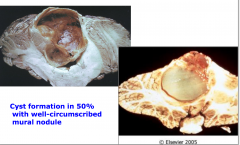
Pilocystic astrocytoma
Cystic formation with well-circumscribed mural nodule |
|
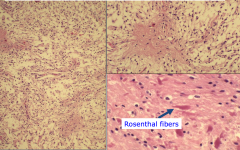
Pathology of Pilocystic Astrocytoma
|
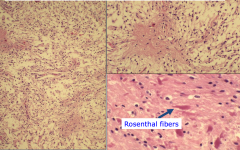
Biphasic Pattern: densely fibrillary (pilocytic) areas alternating with microcystic component
Hair like processes (pilo means hair) Classic finding is a rosenthal fiber - for diagnosis pilocystic astrocytoma |
|
|
Oligodendroglioma
|
Adults in 5th to 6th decade
Clinical S/S: long history of progressive neurological symptoms (seizures, headache focal signs) |
|
|
Imaging of Oligodendroglioma
|
Well defined hypodense/hypointense mass, may see calcification
|
|
|
Prognosis of Oligodendroglioma
|
Median survival - 5 to 10 years for grade II
Better survival than with astrocytomas |
|
|
Oligodendroglioma WHO grades
|
There are two:
II - oligodendroglioma III - anaplastic oligodendroglioma Allelic loss of chromosome 1p and 19q are predictors of prolonged survival and susceptibility to chemotherapy in anaplastic oligodendrogliomas |
|
|
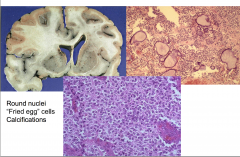
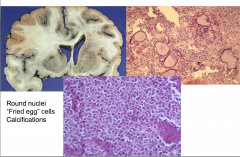
Oligodendroglioma
Round Nuclei "Fried egg" cells calcifications Halo around nucleus |
|
|
Anaplastic oligodendroglioma WHO grade 3
Hemorrhage and necrosis |
|
|
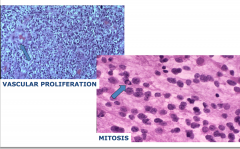
Anaplastic oligodendroglioma, WHO grade 3
Features are mitosis and vascular proliferation |
|
|
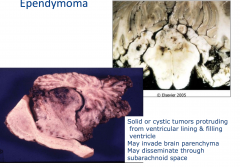
Ependymoma
|
Typically occurs in children and young adults
Occurs along ventricular system, usually posterior fossa (4th ventricle) |
|
|
Clinical S/S of Ependymoma
|
Hydrocephalus, occasionally seizures
|
|
|
Imaging of Ependymoma
|
Well-circumscribed mass
|
|
|
WHO grades associated with Ependymoma
|
Enpendymoma (WHO II)
Anaplastic ependymoma (WHO III) |
|
|
Prognosis of ependymoma
|
Average survival for posterior fossa tumors is 4 years
|
|
|
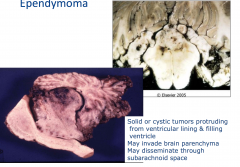
Mass that is distending the ventricle
Can be solid or cystic |
|
|
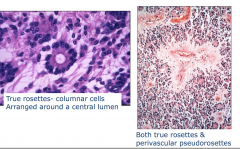
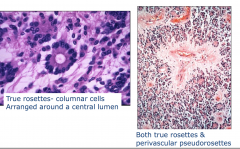
Ependymoma:Histology
Pseudorosette - line up around the vessel True rosettes - columnar cells - trying to make a ventricle Arranged around a central lumen |
|
|
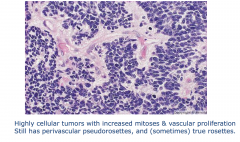
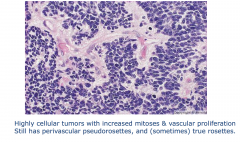
Anaplastic ependymoma
|
|
|
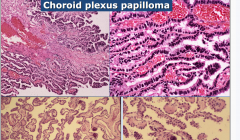
Choroid Plexus Papilloma
|
Typically found in first two decades (in children)
Occurs in 4th ventricle, lateral ventricle, 3rd ventricle and cerebello-pontine angle |
|
|
Presentation of choroid plexus papilloma
|
Hydrocephalus
Overproduction of CSF Obstruction of CSF flow |
|
|
Choroid Plexus Carcinoma
|
Occurs in children < 10 years old
Rare in adults |
|
|
Prognosis of Choroid Plexus Papilloma/Carcinoma
|
Choroid Plexus Papilloma - very good with surgical resection
Choroid Plexus Carcinoma - Poor Prognosis |
|
|
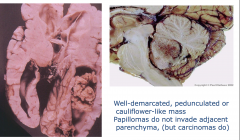
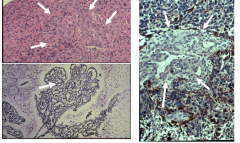
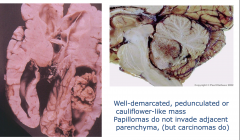
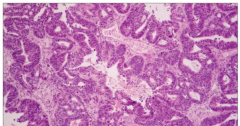
Choroid Plexus Papilloma
Exaggerated choroid plexus Forms papillary structures Well-demarcated, penduculated, or cauliflower mass Papillomas do not invade adjacent parenchyma (but carcinomas do) |
|
|
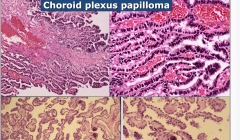
Bottom = Normal
Choroid Plexus Papilloma (top) - hyperchromatic, complex |
|
Colloid Cyst
|
- Usually attached to roof of 3rd ventricle
- Intermittent obstruction of the foramen of Monro Positional Headache Think-walled cyst lined by cuboid/columnar epithelium |
|
|
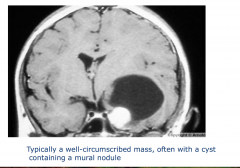
Ganglioglioma
|
Usually in the first three decades
Long standing history of seizure is common Typically supratentorial and in temporal lobe Imaging; solid or cystic, often calcification Surgical resection is usually curative No radiation or chemo needed Consists of neurons and astrocytes |
|
|
Ganglioglioma
-typically a well-circumscribed mass, often with a cyst containing a mural nodule - increasing the pressure in the temporal lobe |
|
|
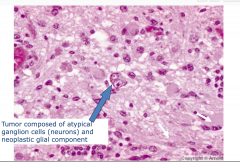
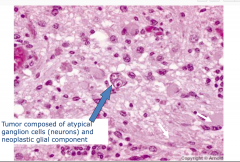
Ganglioglioma Pathology
-tumor composed of atypical ganglion cells (neurons) and neoplastic glial component Looks like a normal neuron but can have multiple nuclei |
|
|
Medulloblastoma
|
Primitive neuroectodermal neoplasm of posterior fossa (small cells that don't show much differentiation)
1/3 of pediatric posterior fossa tumors |
|
|
Clinical S/S of Medulloblastoma
|
-Cerebellar dysfunction (ataxia)
Increased intracranial pressure |
|
|
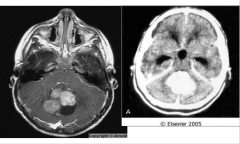
Imaging of Medulloblastoma
|
Well defined contrast enhancing mass; may see leptomeningeal spread
|
|
|
Treatment of Medulloblastoma
|
Surgical resection followed by radiation
|
|
|
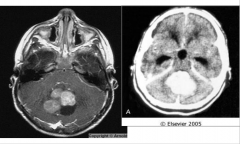
Medulloblastoma
|
|
|
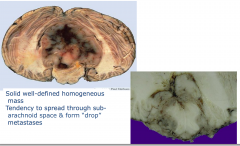
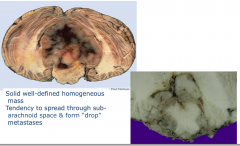
Medullolastoma
- solid well defined homogenous mass - tendency to spread through sub-arachnoid space and form "drop"metastases |
|
|
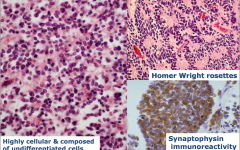
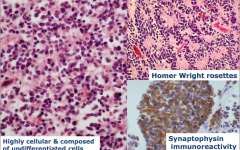
Medulloblastoma
-highly cellular and composed of undifferentiated cells |
|
|
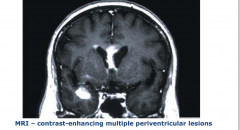
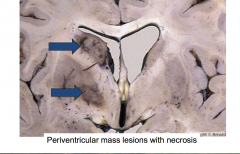
Primary CNS Lymphoma
|
40-60 y/o
Epstein-barr virus association 98% B-cell 2% T-cell Symptoms are non-specific, referable to mass lesion 2/3 are supratentorial poor prognosis - most die within one year (Rx - chemotherapy and radiation, spread of disease outside of CNS is rare) |
|
|
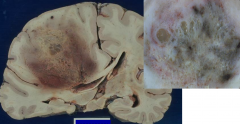
Primary CNS Lymphoma
|
|
|
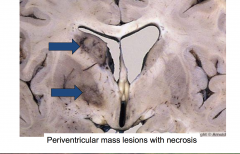
Primary CNS lymphoma
Mass lesions around the ventricular system |
|
|
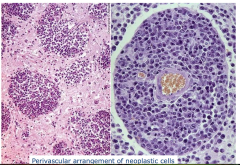
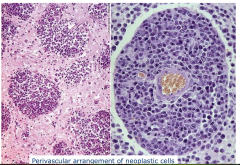
Primary CNS Lymphoma
- perivascular arrangement of neoplastic cells |
|
|
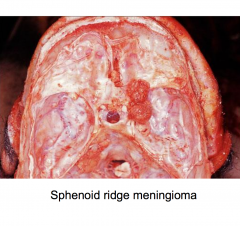
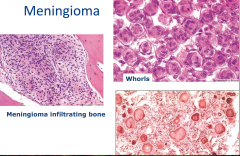
Meningioma
|
- Most common extraparenchymal neoplasm of CNS
- Middle to late adult life - Women > men - Symptoms due to enlarging mass; may have increased intracranial pressure or focal neurologic signs |
|
|
Imaging of Meningioma
|
Dural based, vascular, contrast enhancing, well-defined
On the surface of the brain, not deep in the brain. |
|
|
What radiation treatment is associated with meningioma?
|
NF2
|
|
|
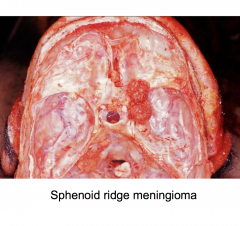
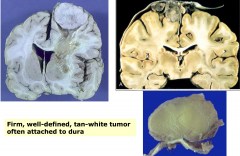
Meningioma
|
|
|
- Meningioma
- firm, well-defined, tan-white tumor often attached to dura - Circumscribed |
|
|
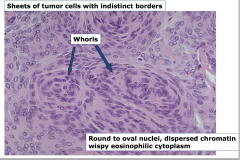
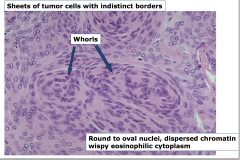
Meningioma
** -whorls - round to oval nuclei, dispersed chromatin wispy eosinophilic cytoplasm |
|
|
Meningioma
** whorls and psammomma bodies which are whorls that have calcified |
|
|
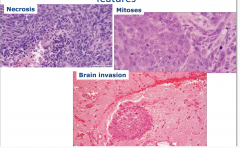
Meningioma, atypical and anaplastic features
|
|
|
Metastatic tumors to the CNS
|
May be first presentation of malignancy
Most originate in the lung or breast carcinomas Clinical S/S: headaches, focal neurologic signs, altered mental status Radiographically - distinct contrast-enhancing mass with surrounding edema, usually multiple |
|
|
Prognosis of metastatic tumors to CNS
|
poor most die within a few months
|
|
|
Metastatic Carcinoma
Usually well circumscribed with pushing margin |
|
|
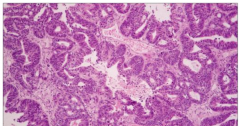
Metastatic carcinoma - adenocarcinma
|
|
|
Meningeal Carcinomatosis
Leptomeningeal proliferation - presence of tumor within meninges - can present like a meningitis or stoke |
|
|
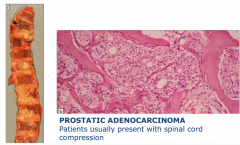
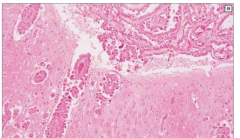
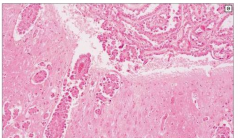
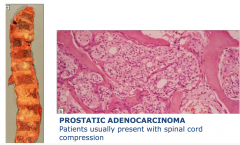
Metastasis to vertebral bodies usually from prostate
|
|
|
Schwannoma
|
Peripheral nerve sheath tumor
Benign tumor of Schwann cells 4th-6th decades Usually head and neck Asymptomatic masses Spinal tumors -radicular pain Symptoms - hearing loss, tinnitis, facial numbness |
|

|

Vestibulocochlear Schwannoma
At cerebellar-pontine angle typically example of NF-2 |
|
|
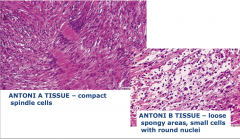
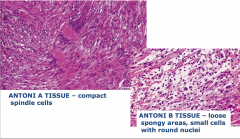
Schwannoma
Antoni A tissue = packed together Antoni B tissue = loose tissue |
|
|
Neurofibroma
|
-Benign tumor composed of Schwann cells, fibroblasts, and perineural cells
- Associated with neurofibromatosis type 1 (NF1) |
|
|
Forms of neurofibroma
|
- Cutaneous (localized) neurofibroma: most common
in dermis or subdermal usually solitary (not associated with NF1) - Peripheral Nerve solitary plexiform - usually in NF1 |
|
Neurofibroma histology
|
Hypocellular
Elongated spindle cells with wavy nuclei Diffusely infiltrate adjacent nerve and soft tissue |
|
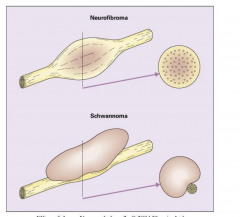
Neurofibroma vs. Schwannoma
|
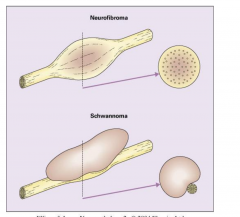
Nerve wont be destroyed with a schwannoma, but nerve is destroyed with neurofibroma
|
|
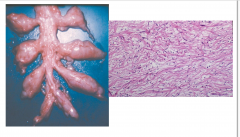
Plexiform Neurofibroma
|
- Occurs almost exclusively in NF1
- Transformation of multiple fascicles of nerves into neurofibroma with preservation of anatomic configuration - Typically affects larger nerves or a plexus - High likelihood of malignant transformation |
|
Malignant Peripheral Nerve Sheath Tumor
|
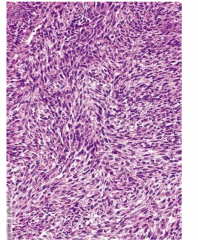
Mostly in extremities
In CNS, associated with trigeminal nerve Strong association with NF1 High grade, aggressive Infiltrative, non-encapsulated fleshy masses Highly cellular, moderate to marked nuclear pleomorphism High mitotic rate |
|
|
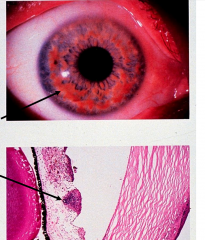
Neurofibromatosis 1
|
Autosomal Dominant
Neurofibromas, cafe-au-lait spots, lisch nodules, optic glioma, osseous lesions, axillary freckling, family history NF1 gene on chr 17 gene product neurofibromin |
|
|
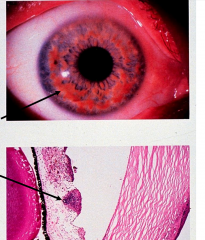
Lisch nodules: pigmented hamartomas in iris
|
|
|
Optic nerve glioma - astrocytoma replacing the optic nerve
|
|
|
Neurofibromatosis II
|
Autosomal dominant
Chr 22 gene product is merlin - bilateral vestibular schwannomas, family history, meningiomas, schwannomas, gliomas, neurofibromas - lens opacity, cerebral calcifications |
|
|
Von Hippl Lindau disease
|
Autosomal dominant
VHL gene on chr 3 |
|
|
Features of Von Hippl Lindau disease
|
Hemangioblastomas of CNS and retina
Cerebellar hemangioblastomas Renal Cell Carcinoma Pheochromocytoma Visceral Cysts |
|
Hemangioblastoma
|
Typically in the cerebellum
Symptoms usually relate to increased intracranial pressure MRI shows well-defined contrast enhancing cystic mass with mural nodule Treat with surgical resection |
|
|
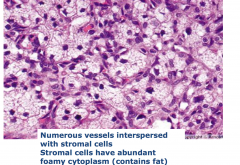
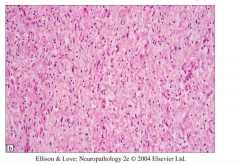
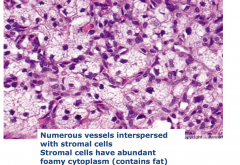
Hemangioblastoma
- numerous vessel interspersed with stomal cells - Stromal cells have abundant foamy cytoplasm |
|
|
Tuberous Sclerosis
|
Autosomal dominant
Mutations in two genes chr 9 (codes hamartin), 16 (codes tuberin) |
|
|
Features of tuberous sclerosis
|
cortical hamartomas
subcortical glioneuronal hamartomas subependymal giant cell astrocytomas |
|

Tubers
|

Firm areas in cortex
Slightly enlarged and white Pt tend to present with seizures |
|
Subependymal nodules
|
Like tuber, but subependymal location
|
|

Tuber Histology
|

Neurons haphazardly arranged in cortex
Often have glial as well as neuronal features |
|
Subependymal giant cell astrocytoma
|
Likely to cause obstructive hydrocephalus
Exophytic solid well-defined mass arising in the wall of lateral ventricle |
|
Subependymal giant cell astrocytoma
|
Large pleomorphic multinucleated tumor cells with eosinophilc cytoplasm
May be of astrocytic or glioneuronal origin No malignant transformation, local invasion reported |
|
|
Paraneoplastic Syndromes
|
Clinical syndrome produced by remote effect of a systemic malignancy that cannot be attributed to direct invasion by tumor or its metastasis, infection, ischemia, surgery, or related metabolic or nutritional disorders or toxic effects of therapy
|
|
|
Two categories of paraneoplastic syndromes
|
1. Related to ectopic hormone production
2. Neurologic syndromes: rare (strong female predominance) |
|
|
Presentation of Paraneoplastic Neurologic Syndromes
|
Subacute worsening over weeks to months
May be presenting symptom of underlying malignancy Initial cancer screening may be negative Neurosymptoms occur when malignancy is at a limited stage due to effective anti-tumor immune response Patients have more favorable oncological outcome |
|
|
Subacute cerebellar ataxia
|
Progressive ataxia, dysarthria, nystagmus, vertigo, diplopia, titubation(shaking of the head)
associated with ovarian cancer or breast cancer antibody to purkinke cells (PCA1) |
|
|
Lambert Eaton Myasthenic Syndrome
|
- Clinical : muscle weakness, especially in legs that improves with testing on exam - extraocular muscles are spared
- Antibodies to P/Q- type voltage gated calcium channels - leads to decreased acetylcholine release Most commonly associated with SCLC (small cell lung cancer) |

