![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
134 Cards in this Set
- Front
- Back

|

|
|
|
Leptomeningeal Infection
|
Pia and arachnoid mater. Results in meningitis
|
|
|
Parenchymal Inflammation
|
- Encephalitis/cerebritis/myelitis (spinal cord)
- When meninges and brain tissue are affected: meningoencephalitis - Brain abscess |
|
|
Subdural or epidural inflammation
|
Subdural/epidural empyemas
|
|
|
How does infection manifest in the brain?
|
Routes of entrance:
- hematogenous spread (arterial spread, retrograde venous spread - anastomotic connections between face veins and cerebral circulation & paravertebral venous plexus, batson (at the caudal spinal cord)) - Local extension, air sinuses, indected tooth - Neural route (extension from PNS to CNS) - Direct implantation - trauma, iatrogenic |
|
|
Neurotropism
|
A special affinity for nervous tissue
|
|
|
Menchanisms of Neurotropism
|
- Viral specific receptors on brain cells
- Poliovirus for motor neurons of anterior horns of spinal cord - Mumps virus for ependymal cells lining ventricles - Capsule proteins that adhere to meninges and possess antiphagocytic properties (Group B strep, E. coli subtypes) - Viral spread along nerves (HSV, Rabies, Varicella zoster virus) |
|
|
Signs and symptoms of meningitis
|
Headache, photophobia, stiff neck (nuchal rigidity), clouded consciousness, fever
|
|
|
Hyperacute Meningitis
|
< 24 hours
Meningococcal meningitis (aggressive organism, spreads quickly, not very much inflammation) - Sparse inflammation, numerous organisms, congestion |
|
|
Acute Meningitis
|
2-7 days
Most common infection in CNS Usually bacterial Usually results from hematogenous spread |
|
|
Subacute/Chronic Meningitis
|
> 1 week
Tuberculosis, syphilis (often brain parenchyma also affected - doesn't necessarily restrict themselves to the meninges) Lymphocytes, plasma cells, macrophages appear in exudate |
|
|
Aseptic Meningitis
|
Usually viral
Much less fulminant than bacterial meningitis and less severe symptoms Summer & early fall Lymphocytic infiltrate in meninges |
|

|
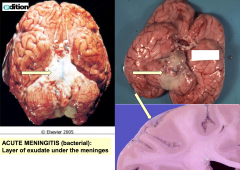
Acute Meningitis
|
|

|
Acute Bacterial Meningitis
|
|
|
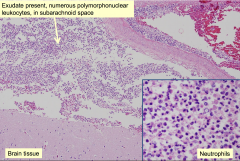
Complications of bacterial meningitis
|
Brain Infarcts
Secondary Vasculitis Phlebitis may occur and cause infarction of underlying brain tissue |
|

|
Complications of bacterial meningitis
|
|
|
Aseptic Meningitis
|
Causative organisms are arboviruses, enterovirus (most common) echovirus and coxsackie.
Less severe inflammatory process. Much more sparse Lymphocytes and some have accumulated around the superficial brain. |
|
|
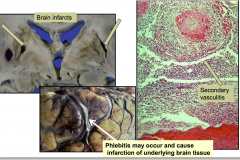
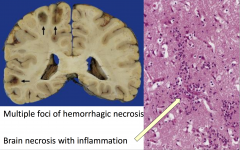
Brain Abscesses
|
Parenchymal Infection
Brain abscesses Circumscribed focus of infection (tend to be walled off by fibroblastic proliferation and collage. Get a capsule wall - in the center - there will be necrosis. Can get a mass lesion. May not present with evidence of infection) Clinical S/S are focal deficits, raised intracranial pressure. Usually bacterial or fungal origin |
|
|
Brain Abscess causes in an immunocompetent host
|
- Strep
- Staph |
|
|
Brain Abscess causes in an immunocompromised host
|
- Toxoplasma
- Nocardia - Listeria - Gram neg bacilli - Mycobacteria - Fungi |
|

|

|
|

|
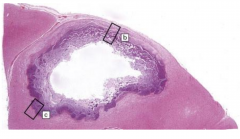
Brain abscess: center is necrotic and at edges are inflammatory cells and fibrous capsule
|
|
|
Parenchymal Infections: Encephalitis
|
Diffuse involvement of brain parenchyma
|
|
|
Conditions associated with inflammation of the brain
|
- Spinal cord myelitis
- Meninges and brain meningoencephalitis - Maybe be bacterial, viral, or fungal in origin |
|
|
Bacterial meningoencephalitis
|
Can be caused by tuberculosis
Syphilis Lyme Disease |
|
|
Mycobacterium tuberculosis
|
CNS involvement in 10-15%
HIV infection is a risk factor |
|
|
Meningoencephalitis
|
- Most common form of TB in CNS
- CSF elevated pressure and protein, decreased glucose, and lymphocytic pleocytosis - S/S: headache, lethargy, confusion, and vomiting - Meninges contain lymphocytes, macrophages, granulomas with extension into underlying brain |
|

|
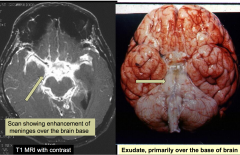
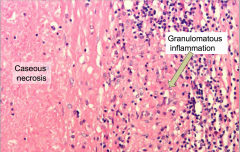
Tuberculosis meningitis
|
|

|
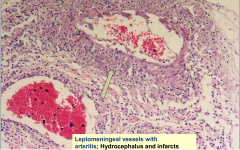
Leptomeningeal vessels with arteritis
|
|
|
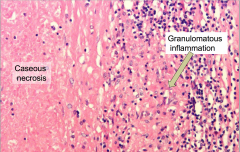
Tuberculosis in the CNS: Tuberculoma
|
Mass lesion with central necrotic core of caseation, surrounded by fibroblasts, epithelioid histiocytes, giant cells, and lymphocytes
- AFB are present in necrosis |
|

|
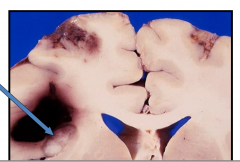
Tuberculosis in the CNS: Tuberculoma
|
|

|

|
|
|
|
|
|
Spondylitis (Pott's Disease)
|
- Granulomatous process involves vertebral bodies & discs
- Causes epidural abscess - Cord compression, vertebral collapse - Epidural extension of the granulomatous inflammation |
|
|
Neurosyphilis
|
- Treponema pallidum
- Months/ yrs after initial infection, 10% of untreated patients develop tertiary syphilis |
|
|
Major forms of neurosyphilis
|
- General paresis (paretic neurosyphilis)
- Meningovascular - Tabes dorsalis |
|
|
General Paresis (Paretic Neurosyphilis)
|
- Gradual impairment of cognition/attention
- Meningo-encephalitis: thickened meninges and atrophic brain meningeal and parenchymal perivascular lymphocytes, plasma cells, and microglia |
|

|
General Paresis (Paretic Neurosyphilis)
|
|
|
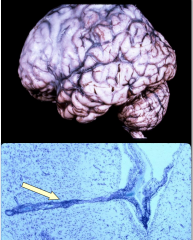
Meningovascular Type (chronic meningitis and multifocal arteritis)
|
- Severe at base of brain
- Causes of infarcts and hydrocephalus - Meningeal and arterial/arteriolar lymphocytes and plasma cells with collagenous thickening of wall and eventual occlusion - Often focal neurologic deficits due to vascular compromis secondary to arteritis |
|

|
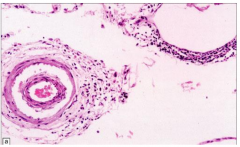
Meningovascular type - chronic meningitis and multifocal arteritis
|
|
|
Tabes Dorsalis
|
- Chronic inflammation in dorsal roots and ganglia with loss of neurons and associated degeneration of posterior columns (axons and myelin)
- ' Lightening pains' or paraesthesias in affected roots, eventual loss of position/vibration sense; shuffling broad-based gait |
|

|
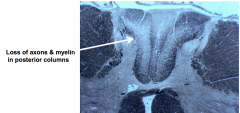
Taves Dorsalis
|
|
|
Viral (meningo) encephalitis : General features
|
Perivascular lymphocytes, microglial nodules, neuronophagia (dead neuron that is being eaten up)
|
|
|
Specific organisms associates with viral (meningo)encephalitis
|
-arboviral encephalitis
- herpes virus infections (HSV1/2, CMV, Varicella-zoster) - HIV - PML |
|
|
Viral encephalitis: Characteristic microscopic pathology
|
Cluster of lymphocytes and microglial cells and often reactive astrocytes and maybe a neuron in the center that's being eaten up.
|
|
|
HSV1 in the CNS
|
- Most common cause of sporadic acute viral encephalitis in temperate climates
- Headache, fever, mood, memory, behavior abnormalities, drowsiness, coma - MRI focal abnormalities in frontal or temporal lobes |
|
|
What happens to the CSF with HSV1?
|
- Increased pressure
- Lymphocytic pleocytosis - elevated protein - PCR for HSV1 DNA |
|
|
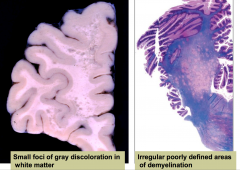
Acute herpes simplex encephalitis
|
congestion, swelling, hemorrhagic necrosis of temporal lobes
|
|

|
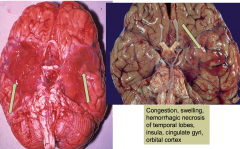
Acute Herpes Simplex encephalitis
|
|

|
Acute Herpes simplex encephalitis
- herpes is aggressive and tends to cause hemorrhage |
|
|
HSV2 in the CNS
|
Meningitis in neonates passing through the birth canal in mother with an active HSV2 infection
|
|
|
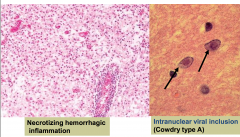
CMV in the CNS
|
Commonest opportunist viral infection in AIDS patients
Subacute encephalitis Microglial nodules Cytomegalic cells contain viral inclusions - may be either intranuclear or intracytoplasmic |
|
|
Varicella Zoster in the CNS
|
- Reactivation of latent virus residing in sensory ganglia
- Vesicles in dermatome distribution - Followed by scar and pain - Dorsal root ganglia or sensory cranial nerve ganglia have lymphocytes, sometimes necrosis |
|

|
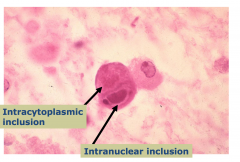
CMV viral inclusion
Cells get big with CMV infection |
|
|
Arboviral meningoencephalitis
|
Important cause of epidemic encephalitis
Generalized neurological deficits (seizures, confusion, stupor, delirium, coma) and focal signs PCR important for virus id |
|
|
HIV infection in the CNS
|
RNA virus, retrovirus
Microglia are the most common cell infected in CNS by HIV CNS is a major target of HIV infection |
|
|
Types of involvement associated with HIV infection in CNS
|
HIV meningitis
HIV encephalitis/leukoencephalopathy Vacuolar myelopathy |
|
|
HIV meningitis
|
Presents during acute flu-like illness at time of seroconversion
|
|
|
HIV encephalitis/leukoencephalopathy
|
present in >75% of autopsied HIV patients
clinical s/s are cognitive and behavioral deterioration, eventually dementia, ataxia and tremor slight diffuse atrophy ** classic lesion : microglial nodule containing multinucleated microglial cells (contain HIV virus) also perivascular lymphocytes, pathy demyelination and astrocytosis |
|

|
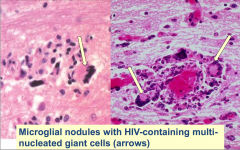
HIV encephalitis
|
|
|
Progressive multifocal leukencephalopathy
|
- Occurs in immunosuppressed hosts (often AIDS patients) with immunosuppression JC virus is reactivated. Most people are infected with JC virus early on, but overcome it. It reoccurs with HIV
- Caused by JC virus, polyomavirus, infects oligodendrocytes - Most have serologic evidence of prior JC virus infection by adolescence. JC virus is reactivated with immunosuppression |
|

|
Progressive Multifocal Leukoencephalopathy
|
|
|
Toxoplasma gondii
|
Man is intermediate host (cat is definitive host)
Infection secondary to ingestion of contaminated food (cat feces) or raw/undercooked meat from sheep or pig Congenital disease (transmission to fetus if infection occurs during pregnancy) Important infection in immunocompromised hosts It is the most common cause of mass lesions in CNS in AIDS patients Uncommon in healthy adults |
|

|
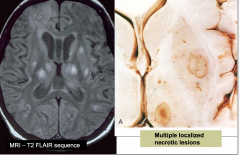
Cerebral Toxoplasmosis
|
|
|
Fungal (meningo)encephalitis
|
- Commonly occur in immunocompromised hosts
(candida, mucor, aspergillus) |
|
|
Patterns of damage for fungal (meningo)encephalitis
|
- chronic meningitis
- parenchymal invasion (encephalitis) - vasculitis (especially aspergillus and mucor) : causes hemorrhagic infarcts |
|

|
aspergillus brain infection
|
|
|
Cryptococcus
|
Affects lungs first usually and spread hematogenously to brain
most often in immunosuppressed patients, but may occur in immunocompetent hosts organism found in soil and bird excreta Main forms: - meningitis with or without brain parenchymal cysts (encephalitis) - abscesses (cryptococcomas) CSF: lymphocytes, high protein, normal or reduced glucose -india ink stains allow identification of organism (by negative staining of capsule) - assay for presence of cryptococcal antigen is more sensitive |
|

|

|
|
|
Cryptococcal meningoencephalitis
|
Multiple intraparenchymal cysts
Also called "soap bubbles" which are secondary to gelatinous capsular material occur in 50% of cases in addition to meningeal involvement |
|

|
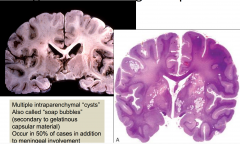
Cryptococcal meningoencephalitis
|
|
|
Cryptococcal meningitis histology
|
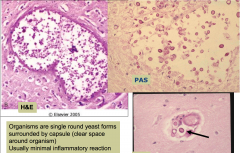
organisms are single round yeast forms surrounded by capsule (clear space around organism)
|
|
|
Parasites in the nervous system
|
- Single-celled organisms
- Infection occurs in immunocompetent and immunosuppressed - Causes meningoencephalitis or abscesses |
|
|
Epidural and subdural empyemas
|
- Usually bacterial (staph or strep commonly)
- Local extension of infectious process (can be from frontal or mastoid sinusitis, otitis media, trauma, osteomyelitis, surgical procedure) |
|
|
Most common cause of bacterial meningitis
|
Streptococcus pneumoniae
|
|
|
Most common cause of meningitis in a 66 year old or alcoholic
|
Listeria
|
|
|
Most common cause of meningitis in an AIDs patient
|
Cryptococcus
|
|
|
Most common cause of meningitis in a neurosurgery patient
|
Staphylococci
|
|
|
Most common cause of meningitis in a freshman college student
|
N. meningitidis
|
|
|
Most common cause of meningitis in a patient that presents as sick and in summer
|
enteroviral
|
|
|
Most common cause of meningitis in an Asian immigrant that has been sick for a few weeks
|
TB
|
|
|
How do you best treat a patient with meningitis that was caused by S. pneumoniae?
|
IV ceftriaxone, vanco, and corticosteroids (vanco increase it's resistant)
|
|
|
How do you treat meningitis if the pt was 66 or alcoholic?
|
Add IV ampicillin to ceftriaxone, vanco, and corticosteroids to cover for listeria
|
|
|
What can be done to try to prevent bacterial meningitis?
|
Immunizations for pneumococcus, meningococcus, and H flu.
|
|
|
Principles of CNS infection Rx
|
- prompt initiation of empiric coverage, especially if bacterial etiology is suspected
- high doses and frequent dosing -bbb lowers levels; CSF penetration is essential for activity - cidal agents instead of static |
|
|
Patient that has been "Acting crazy" with auditory hallucinations and bizarre behavior, headache, afebrile, and stiff neck. What is the most likely cause?
|
HSV
|
|
|
Patient that has been "Acting crazy" with auditory hallucinations and bizarre behavior, headache, afebrile, and stiff neck AND presents in summer. What is the most likely cause?
|
arbovirus
|
|
|
Patient that has been "Acting crazy" with auditory hallucinations and bizarre behavior, headache, afebrile, and stiff neck AND is an AIDS patient with focal neurologic deficits. What is the most likely cause?
|
Toxoplasmosis or PML
|
|
|
Patient that has been "Acting crazy" with auditory hallucinations and bizarre behavior, headache, afebrile, and stiff neck AND she removed a bat from the house. What is the most likely cause?
|
Rabies
|
|
|
Patient that has been "Acting crazy" with auditory hallucinations and bizarre behavior, headache, afebrile, and stiff neck AND symptoms have been slowly worsening over a few months. What is the most likely cause?
|
Prion
|
|
|
Treatment for encephalitis
|
- Prompt initiation - delay increase mortality and sequelae
- High dose (BBB and CNS penetration) - Acyclovir for HSV |
|
|
Meninges
|
Three membranes enclosing the brain and the spinal cord, comprising the dura mater, pia mater, and arachnoid membrane.
|
|
|
What layers can become inflamed during bacterial meningitis?
|
Pia mater and arachnoid
|
|
|
Primarily pathogens of bacterial meningitis
|
Group B Strep
S. pneumoniae N. meningitidis H. influenza |
|
|
Bacteria that cause meningitis in premies and newborns up to 3 months
|
- group B streptococci (inhibit the vagina and are mainly a cause during the first week of life)
- E. coli that normally inhabit the digestive tract and carry the K1 anitgen - listeria |
|
|
Bacteria that cause meningitis in older children
|
S. pneumoniae
N. meningitidis H. influenzae type B |
|
|
Bacteria that cause meningitis in adults
|
- N. meningitidis and S. pneumoniae
- Listeria in adults over 50 |
|
|
Group B Streptococcus (agalactiae)
|
Gram Pos
Polysacc capsule NO Conjugat vaccine properties: neonatal sepsis --> meningitis and antibiotic therapy (beta-lactams) |
|
|
Streptococcus pneumoniae
|
Gram pos
Polysacc Capsule Conjugat vaccine Also responsible for most pneumonia alpha hemolytic/optochin sensitive diplococcus identified in CSF |
|
|
Neisseria meningitidis
|
Gram negative
Polysacc capsule Conjugat vaccine Conjugate vaccine does not protect against serotype B, a di-sialic acid homopolymer similar to human structure |
|
|
H. Influenzae Type B : what is the capsular polysaccharide composed of?
|
Ribose and ribitol
|
|
|
Immunity to H. Influenzae type B
|
- Good relationship between age and susceptibility
- Children < 3 mo, maternal Ab is protective - Most invasive disease occurs between 3 mo and 3 years of age - Children under 3 show a humoral immunodeficiency to Hib - Children older than 3 develop bactericidal Ig to HIb |
|
|
1st generation Hib vaccine
|
- Purified capsular polysaccharide of Hib
- 90% effective in children > 24 mo - ineffective in children < 18 mo Problems: Polysacc are 1.) poor immunogens 2.) stimulate T-independent Ab 3.) Poor immunologic memory |
|
|
2nd generation Hib Vaccine
|
- PRP Protein Conjugates
Vaccine: PRP-D and protein carrier is the diphtheria toxoid |
|
|
How do polysaccharide conjugate vaccines work?
|
They stimulate a T-cell dependent antibody response and a memory response
|
|
|
Virulent factors associated with Neisseria meningitidis
|
- Lipooligosaccharide: component of outer membrane (endotoxin) when stimulated TLR system to produce: fever, septic shock, and hemorrhage due to the destruction of RBCs
- Polysaccharide Capsule: prevents host phagocytosis and evasion of host immune response - Fimbriae : mediates attachment of the bacterium to cells of the nasopharynx |
|
|
Diagnosing N. meningitidis
|
- CSF fluid
- Relies on culturing organism on chocolate agar plate - PCR identifies N.m |
|
|
Pathology of N. meningitidis
|
- Fatality risk approaches 15% within 12 hours of infection, so initiate testing as quickly as possible, do not wait for results
- Persons confirmed should be hospitalized immediately for treatment |
|
|
Prevention of N. meningitidis
|
Can be transmitted. Contact of the infected patient over the 7 days before onset should receive Ab to prevent secondary infections - especially in young children.
|
|
|
Current meningococcal conjugate vaccine
|
Quadrivalent vaccine of serogroups A, C, W-135 and Y
Conjugated to diphtheria toxoid (polysaccharide-protein complex) Enhanced duration of protection Increased immunity with booster vaccinations Effective herd immunity 2-55 |
|
|
beta, alpha, and gamma hemolysis
|
beta: complete lysis
alpha: partial lysis gamma: no lysis |
|
|
Streptococcus pneumoniae
|
Elongated gram-pos cocci in pairs and short chains
cell wall includes teichoic acid |
|
|
Virulence of S. pneumoniae is determined by
|
ability to colonize oropharynx
spread into normally sterile tissues stimulate local inflammatory response evade phagocytic kiling |
|
|
Diseases associated with S. pneumoniae
|
Pneumonia
Sinusitis Otits media Meningitis Bacteremia |
|
|
Group B streptococcus, Streptococcus agalactiae
|
Beta hemolytic
Lancefield typing scheme Group B Common inhabitant of pharynx, vagina, GI tract Neonatal infections, meningitis No licensed vaccine Penicillin is the drug of choice Selective prophylaxis antibiotics for: Group B + women with preterm labor Premature or prolonged membrane rupture Fever in labor |
|
|
Rabies virus morphology
|
- rod or bullet shaped
- envelope with membrane spikes of viral glycoprotein - RNA genome |
|
|
Replication of rabies virus
|
(-) sense RNA virus
Envelope binds to receptor on cell and is endocytosed and fuses at low pH |
|
|
G glycoprotein of rabies elicits?
|
Neutralizing antibodies, but the natural 'timing' of antibody production is not protective. Antigenicity of G protein allows for vaccine production.
|
|
|
Invasion and Pathological Features of Rabies
|
- entry is through a wound or skin abrasion via a bite and introduction of infected saliva
- can be transmitted by infected cornea transplants and more recently from organ transplants - virus replicates in muscle or connective tissue during "incubation" period, which can be months |
|
|
Where does the rabies virus disseminate?
|
To distal sites via nerves - in particular the eye, salivary glands, and innervated skin. Salivary glands are important for animal dissemination
|
|
|
Incubation period of rabies
|
Asymptomatic
3-8 weeks Time depends on dose and location of bite |
|
|
Prodrome of Rabies
|
Early after infection of brain.
Symptoms include nervousness, headache, anxiety, pain at bite site, fever, nausea. Difficult to diagnose rabies based on these symptoms if pt does not reveal the possibility of exposure to rabid animals |
|
|
Last 2-10 days of prodrome of rabies
|
virus presents in brain and often disseminated to other sites (virus can be detected in skin biopsies or saliva at this time) but patients are usually antibody negative at this point
|
|
|
Acute neurological phase of rabies
|
high virus titer in brain and elsewhere, antibody in serum and CNS.
|
|
|
"Furious" or Fulminant - Classic Rabies
|
Bizarre behavior, hallucinations, seizures, hydrophobia - violent spasms of respiratory muscles triggered by drinking water: sight, sound, or mention of water can trigger it. Fury gives way to paralysis, then either coma or sudden fatal cardiac or respiratory arrest
|
|
|
Paralytic or "dumb" rabies
|
Ascending flaccid paralysis leading to fatal paralysis of respiratory muscles
|
|
|
Diagnosis of Rabies
|
- Neurologic symptoms is living persons with suspected exposure establishes initial diagnosis which can be confirmed by detecting virus in CSF, saliva, or skin by PCR.
|
|
|
Diagnosis of Rabies post-mortem
|
Confirmation is made on infected tissue by PCR, dFA
|
|
|
Prevention and Prophylaxis of Rabies
|
Immunization of domestic animals
High risk individuals such as vets, travelers are vaccinated |
|
|
Post-exposure prophylaxis of Rabies
|
Almost always effective if incubation is long enough, which is almost always the cause. Although an exposure is not a medical emergency, PEP should be administered ASAP.
|
|
|
Passive immunization of Rabies
|
Passive immunization: human or equine rabies immune globulin introduced into wound area and intramuscularly to provide Ab until immunization becomes effective - to keep the virus local
|
|
|
Active Immunization of Rabies
|
Human diploid cell vaccine of "killed virus". 4 doses at 0, 3, 7, and 14 days
|
|
|
Prion
|
No DNA/RNA associated
Do not induce an immune response Difficult to inactivate |
|
|
Prion Structure
|
protein encoded by cellular gene PRNP-
|

