![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
167 Cards in this Set
- Front
- Back
|
Epidural Hematoma
|
- Collection of blood between the dura and the skull
- Due to fracture of temporal bone with rupture of middle meningeal artery - Lucid interval may precede neurologic signs - Herniation is lethal complication |
|
|
Subdural Hematoma
|
- Collection of blood underneath the dura
- Due to tearingof bridging veins between the dura and arachnoid - Usually arises with traumaS |
|
|
Clinical Presentation of Subdural Hematoma
|
- Progressive neurologic signs
- Herniation is a lethal complication |
|
|
Unique Features of the CNS
|
- Selective Vulnerability of neuronal systems
- Mature neurons are post-mitotic cells - Unique anatomic/physiologic characteristics |
|
|
Unique Features of CNS: Selective vulnerability of neuronal systems
|
- Degeneration of specific nuclei and connections
- Example: ALS - anterior horn cells and nerves arising from the anterior horn cells are degenerated and those along the cortical spinal tract re as well, but none of the other cells are degenerated. - Example: Alzheimer's - cerebral cortex bears the brunt of the injury |
|
|
Unique Features of CNS: Mature neurons are post-mitotic cells
|
- Loss cannot be repaired
- Recent discovery of stem cells in CNS * In strokes, this is especially important because once these neurons are dead and removed through a reaction and there is glial scar formation, there is no replacement of those neurons and no replacement of that function. - There are stem cells that do occur in the CNS, but these are fairly limited in their distribution and are not able to repair the loss that occurs during a stroke. |
|
|
Unique Features of CNS: Unique Anatomic/ Physiologic Characterisitcs
|
- Bony enclosure
- Metabolic substrate requirements (brain doesn't store fuel and time without this can result in damage) - No lymphatic system (Since there is no lymphatic system in the brain, disease from the lymphatic system outside the brain will not enter) - Presence of CSG - Limited immune surveillance (physical barrier that prevents molecules from going from the blood vessels into the brain due to the blood brain barrier. There are also less immune cells within the brain) ** For most injuries, there is an astrocytic reaction rather than a fibrotic reaction. |
|
|
Characteristics of Normal Neurons
|
- Integration and transmission of cells of the CNS and they use chemical and electrical means to accomplish this.
- Morphology varies by location - Most have nucleus with a prominent nucleolus - Shape varies depending upon location |
|
|
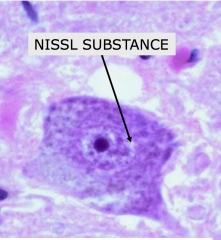
Internal features of the neuron
|
- Nucleus with prominent nucleolus
- Well-defined cytoplasm containing Nissl substance (Nissl Substance = ER) - Branching processes (dendrites) and longer processes (axons) Axons have terminal synapses for chemical transmission to another neuron. |
|
|
Shape of neuron in cerebral cortex
|
Pyramidal and granual neurons
|
|
|
Shape of neuron in Primary Motor Cortex
|
Betz Cells
|
|
|
Shape of neuron in Hippocampus and Cerebellum
|
Granular Neurons
|
|
|
Shape of neuron in Cerebellum
|
Purkinje
|
|
|
Shape of neuron in Spinal Cord
|
Anterior horn cells
|
|
|
Shape of neuron in Basal Ganglia, Thalamus, Brainstem
|
Globoid shaped cells in deep gray nuclei
|
|
|
Shape of neuron in Brain Stem (substantia nigra, locus ceruleus)
|
Melanin containing cells
|
|

|
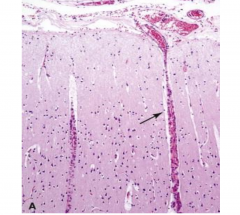
Anterior Horn Cell
|
|

|
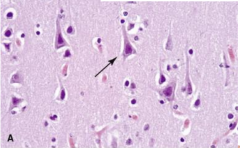
Cerebral Cortex Neurons - Pyramidal Shape
|
|

|
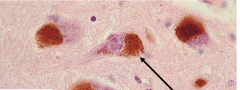
Neuromelanin-containing neurons in brainstem (substantia nigra, locus ceruleus, motor nucleus of vagus)
|
|

|
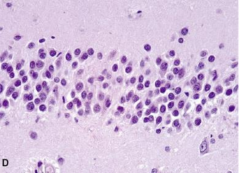
Granular neurons of the dentate facia of hippocampal formation
|
|

|
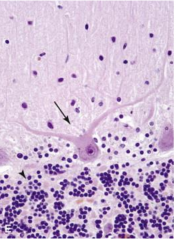
Purkinje cells (arrow) and granular cells (arrowhead) of the cerebellar cortex.
|
|

|
Lipofuscin - accumulates in neuronal cytoplasm with age. Gold and brown pigment. Occurs with all neurons with age.
|
|

|
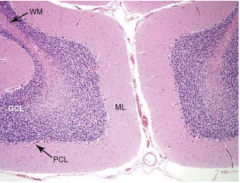
Cerebellum. Cerebellar cortex contains a sparsely cellular molecular layer (ML), Purkinje Cell Layer (PCL), a granular cell layer (GCL), and white matter (WM)
|
|
|
Reactions of neurons to injury
|
- Eosinophilic change (ischemia/hypoxia)
- Central chromatolysis (axonal damage) - Intraneuronal inclusion formation |
|
|
Eosinophilic Degeneration
|
- Indicated lethal ischemia, hypoxia, or hypoglycemia
- Takes 12-24 hours to manifest - Morphologic criteria: Shrinkage of neuronal cell body Loss of Nissl with cytoplasmic eosinophilia Loss of nucleolus with nuclear pyknosis |
|

|
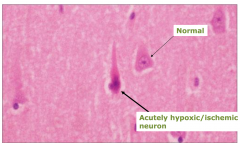
Eosinophilic Neurons (acute hypoxia/ischemia)
|
|

|
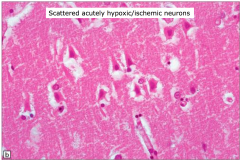
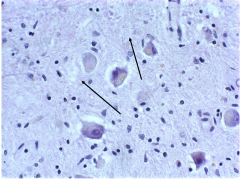
Scattered acutely hypoxic/ischemic neurons
|
|
|
Central Chromatolysis
|
- Manifestation of switch from manufacture of synaptic to structural proteins in response to axonal damage.
- The cell changes its metabolism in response to the damage and begins to make structural proteins instead of synaptic protein. - Reversible, if axonal repair is successful - Cellular swelling with margination of Nissl substance and nucleus and accumulation of filaments and organelles |
|

|
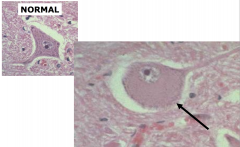
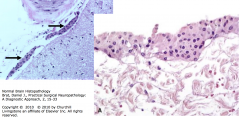
Central Chromatolysis
|
|
|
Macroglia
|
Derived from the neuroectoderm (90% of all CNS cells)
- Astrocytes - Oligodendrocytes - Ependymal Cells * Disease processes that affect one will typically affect the other |
|
|
Microglia
|
Derived from bone marrow.
* Diseases that affect microglia are different than those that affect macroglia |
|
|
Astrocytes
|
- Primary replicating cell within the CNA
- Round to oval nucleus with radiating cytoplasmic processes |
|
|
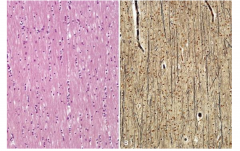
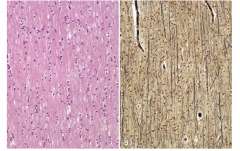
Histology of astrocytes
|
- Star shaped cytoplasm, normally invisible on H&E staining (unless reacting to injury)
- Glial fibrillary acidic protein (GFAP) - major cytoplasmic structural protein - Antibodies to GFAP help visualization of astrocytes |
|
|
Functions of astrocytes
|
- Contribute to the blood-brain barrier
- Cytoplasmic processes (end-feet) on blood vessel walls - Control flow of macromolecules between blood, CSF, and brain - Responsible for repair and scar formation - Maintain extracellular environment - Metabolic buffers or detoxifiers and supply nutrients - Structural support |
|

|
Astrocyte
|
|
|
Reactive Astrocytosis
|
- Astrocytes activate in response to various pathologic conditions
- Provides evidence of disease process - Astrocytes divide and become larger - Increase in GFAP filaments that are reflected in visible eosinophilic cytoplasm - GFAP antibody will help identify the reactive astrocytes - The cytoplasm may appear starlike (fibrillary) or large and round ("gemistocytic") |
|

|
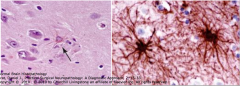
LT - Fibrillary Reactive Astrocytosi
RT - GFAP: Fibrillary reactive astrocytosis |
|
|
Gemistocytic
|
Astrocyte is stuffed with GFAP material
|
|

|
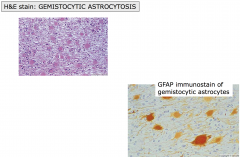
Reactive astrocytosis
|
|
|
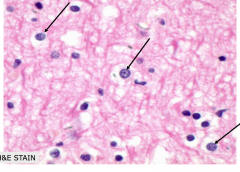
Oligodendroglia
|
- Responsible for myelination in the CNA
- More numerous in white matter than in gray matter - Smaller nucleus and fewer processes than astrocytes - Round dense nucleus - Peri-nuclear halo (artifact) - Does not synthesize GFAP - Lethal injury results in demyelination |
|
|
Diseases involving oligodendrocytes
|
- MS
- Progressive multifocal leukoencephalopathy (caused by a viral infection) - Oligodendrogliomas |
|

|
Oligodendrocyte
|
|
|
White Matter
|
|
|
Ependymal Cells
|
Cuboidal to columnar glial ciliated cells that line ventricular surfaces
Lateral surfaces have cell junctions forming CSF-brain barrier |
|
|
Ependymal Cells
|
|
|
Choroid Plexus
|
-Tufts of epithelium projecting into ventricles
- Secrete CSF - Papillary architecture - Cell junctions between cells ensure CSF-brain barrier |
|
|
CHoroid Plexus
|
|
|
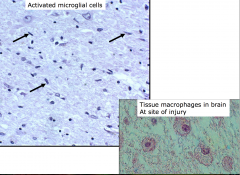
Microglia
|
- Monocyte/Macrophage derived cells that reside in the CNS
- Normally inconspicuous, sparse, rod-shaped nuclei without visible cytoplasm - |
|
|
What happens to microglia with CNS injury?
|
They may become activated and migrate to the site of injury, proliferate, and can differentiate into tissue macrophages (foamy clear cytoplasm)
|
|
|
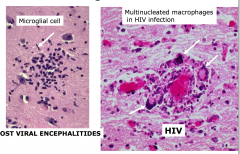
What happens to microglia and astrocytes during a viral infection
|
- Astrocytes and microglia form microglial nodules at sites of neuronal injury
- HIV infection stimulates cellular fusion resulting in multinucleated giant cells in microglial nodules. |
|
|
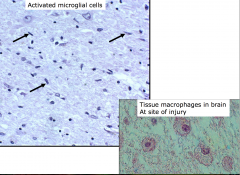
Activated Microglial cells
|
|
|
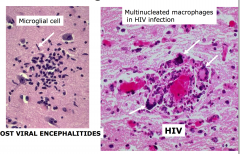
Microglial Nodules
|
|
|
Virchow-Robin Space
|
Large arteries within the subarachnoid space supply the brain by penetrating into the parenchyma creating a space and this space (Virchow-Robin) separates the vessel from the neuropil
|
|
|
Neuropil
|
Network of dendrites and axons in gray matter (in between cell bodies)
|
|

|
Virchow-Robin Space
|
|
|
Meningothelial Cells
|
Present thoughout the arachnoid membranes covering the brain and spinal cord
|
|

|
Meningothelial Cells
|
|
|
CT Scan
|
- Circulary gantry
- X-rays (ionizing radiation is used) - Axial Scan - Cor & sag reformates - Iodinated contrast (head CTs typically don't get contrast - if it does happen, use iodine) - Fast, available, expensive - Can do coronal, but don't see it too often |
|
|
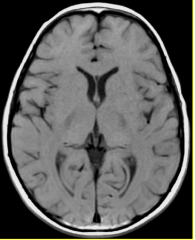
MRI
|
- Cylindrical magnet
- Strong magnetic field, radio waves (no x-rays) - Multiplanar images - Gadolinium contrast - Slower, less available, expensive - Safety issues with metal; compatibility with sick patients |
|
|
Image types in CT
|
- Scan once (twice if giving IV contrast)
- View images using different "windows" (brightness and contrast settings) |
|
|
Image types in MRI
|
- Scan several times (3 to 8+)
- Multiple planes (at least 2 for brain MRI) - Different pulse sequences - View each image set with only one window |
|
|
What is CT used to analyze?
|
- Bone
- Acute hemorrhage - Hydrocephalous - Trauma - Fluid ok for soft tissue |
|
|
What is MRI used to analyze?
|
- Soft tissues and bone marrow (strength)
- Contrast enhancement |
|
|
Substances from bright to dark on CT
|
Bone > Hemorrhage> Brain - gray matter> Brain - white matter > CSF > Fat > Air
|
|
|
Substances from bright to dark on MRI - T1W1
|
Fat > Brain - White Matter > Brain - Gray Matter > CSF > Air, cortical bone
|
|
|
Substances from bright to dark on MRI - T2W1
|
CSF > Fat > Brain - Gray Matter > Brain - White Matter > Air, cortical bone
|
|
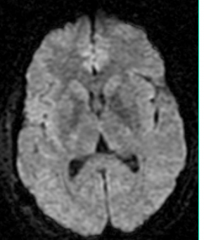
MR DWI
|
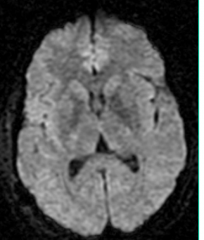
Diffusion weighted imaging. Extremely sensitive for showing acute stokes and abcesses
|
|

|

CT Brain Window
|
|

|
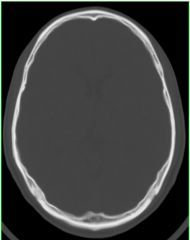
CT Bone Window
|
|
|
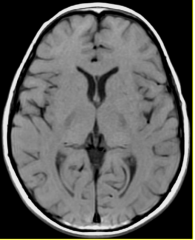
MR T1W1
|
|

|
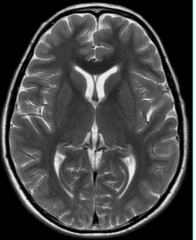
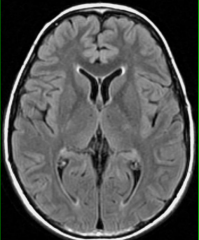
MR T2W1
|
|

|
MR T1W1 + C
|
|

|
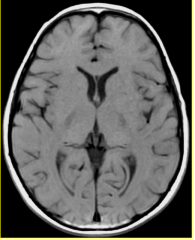
MR T1W1
|
|

|
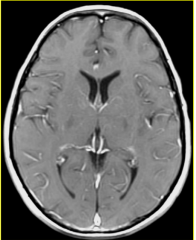
MR FLAIR - T2 weighted image, but darken the CSF
|
|

|
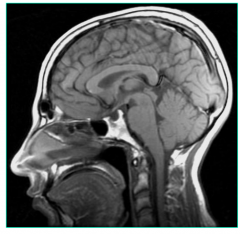
MR T1WI Sagittal
|
|
|
Common CNS Pathology - Brain
|
- Stroke
- MS - HTN - Aneurysm - Tumor - Trauma |
|
|
Common CNS Pathologies - Spine
|
- Trauma
- Degenerative Disease - Infection - Metastatic Disease |
|
|
Common CNS Pathologies - Head & Neck
|
- Facial Trauma
- Infection - SCC - Atherosclerotic Vascular Disease - Other Malignant Disease |
|
|
Neuro CT exams are usually performed without contrast except?
|
- CTs of the head and neck soft tissues looking for infection or malignancy
- CT angiograms of the head and neck - CT venograms of the head and neck |
|
|
Indications for IV gadolinium contrast in MRI
|
- Infection
- Primary tumors or metastatic disease - Demyelinating disease (like MS) |
|
|
For MRI contrast is not usually necessary when evaluating?
|
- Stroke
- Trauma - Degenerative Spine Disease |
|
|
MRA of head
|
without contrast
|
|
|
MRA neck and MRV best done
|
with contrast
|
|
|
CT vs. MRI (CT)
|
- Cheaper
- Cancer Risk due to Ionizing Radition - Takes seconds to minutes to acquire - Allergic reactions more common, nephrotoxicity (contrast material) - Can still scan if pt has pacemaker, aneurysm clip, bullet |
|
|
CT vs. MRI (MRI)
|
- More expensive
- No ionizing radiation - takes 30-50 min to acquite - contrast material usually well tolerated - Usually not safe with pacemakers, aneurysm clips, bullets |
|
|
Acute Intracranial Hemorrhage
|
- Acute hemorrhage is hyperdense (bright) while chronic hemorrhage is hypodense (dark) on CT
- Locations include subarachnoid, subdural, epidural, parenchymal, and intraventricular |
|
|
Two most common causes of subarachnoid hemorrhage
|
Trauma and Ruptured Aneurysm
|
|
|
To look for an aneurysm on CTA what is needed?
|
Contrast.
No contrast necessary for MRA. |
|
|
How do acute infarcts look on CT?
|
- Hypodense (dark) areas, though may not see in first few hours
- Loss of gray/white differentiation - Swelling/edema leads to sulcal effacement or asymmetrically smaller sulci - Hyperdense (bright) vessel sign |
|
|
Blood Brain Barrier
|
- Tight intercellular junctions
- Endothelium has low pinocytotic rate and basement membrane - Dynamic interaction of endothelium with astrocytes and pericytes - Small substances and small lipophilic molecules freely diffuse through membrane - Large substances and hydrophilic molecules require active transport |
|
|
Cerebral Edema
|
- Accumulation of excess fluid in intracellular or extracellular spaces of the brain.
- Major consequence is increased intracranial pressure - Results from a variety of processes and associated with significant morbidity/mortality |
|
|
Two major forms of cerebral edema
|
- Vasogenic edema
- Cytotoxic edema |
|
|
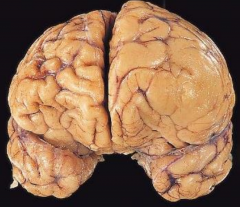
Characteristics of cerebral edema
|
Widened, flattened gyri with narrowed sulci
|
|
|
Vasogenic Edema
|
Extracellular Edema
- Disruption (increased permeability of BBB) - results in shift of fluid from the intravascular to the extravascular compartment - Predominantly involves white matter - Most common causes: Primary or secondary brain tumors, abscesses, contusions, intracerebral hematomas |
|
|
Mechanism of Vasogenic Edema
|
- Newly formed vessels (in tumors) deficient in tight junctions
- Production of vascular endothelial growth factor by tumor cells - Production of inflammatory mediators, chemokines, cytokines, and other growth factors |
|
|
What does vasogenic edema respond to?
|
Corticosteroids and anti-VEGF antibody (bevacizumab)
|
|
|
Gross features of vasogenic edema
|
- Narrowed sulci
- Flattened gyri - Compressed ventricles - Brain softening |
|

|
Vasogenic Edema
|
|

|
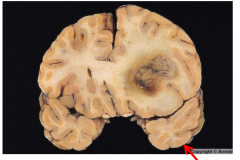
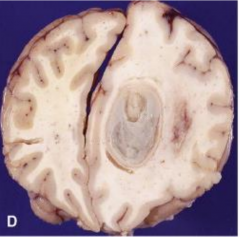
Primary Brain Tumor (Glioblastoma)
|
|

|
Vasogenic cerebral edema. Malignant brain tumors have extensive associated angiogenesis with microvascular proliferation and poorly formed BBB. Result is extensive vasogenic edema and mass effect.
|
|

|
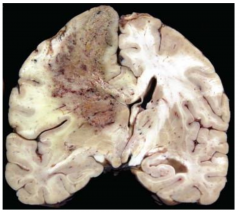
Cerebral Abscess
|
|
|
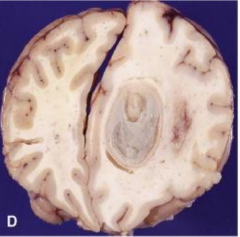
Cerebral Abscess
|
|
|
Cytotoxic Edema
|
"Intracellular Edema"
- occurs secondary to cellular energy failure - results in a shift of water from the extracellular to intracellular compartment - intracellular swelling - large amounts of sodium enter cells, water follows - histologically brain tissue vacuolation - more pronounced in gray matter |
|
|
Most common causes of cytotoxic edema
|
- Ischemia/ infarct
- Meningitis - Trauma - Seizures - Hepatic encephalopathy |
|
|
Mechanisms of cytotoxic edema
|
Dysfunction of neuronal and astrocytic membrane pumps (caused by excess glutamate, extracellular potassium, inflammatory cytokines
|
|
|
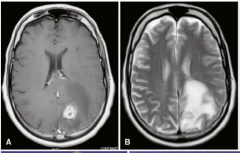
Cytotoxic Edema. Left MCA territory infarct.
Early edema with shift of midline structures from left to right |
|
|
Increased intracranial pressure
|
- Brain volume = Brain + blood + CSF (+lesion)
- Increased volume = increased pressure - Increased pressure leads to decreased perfusion and/or herniation syndromes - Rigid dural folds (falx, tentorium) dictate what type of herniation |
|
|
Subfalcine Herniation
|
- Cingulate gyrus herniates under the falx
- Caused by asymmetric expanding hemispheric lesions - May cause in compression of ant. cerebral art. resulting in infarction |
|

|
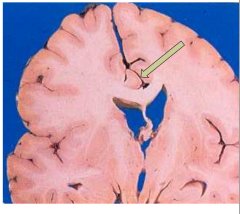
Subfalcine Herniation
|
|
|
Transtentorial Uncal Herniation
|
- Medial temporal lobe displaced through the tentorial opening because of asymmetric expanding lesion
|
|
|
Complications of Transtentorial Uncal Herniation
|
- Ipsilateral CN III compression with pupillary dilatation
- Contralateral peduncular compression (Kernohan's notch) causes ipsilateral hemiparesis - Posterior cerebral artery compression (ipsi- or bilateral) - Duret Hemorrhage |
|

|

Transtentorial Uncal Herniation
|
|
|
Duret Hemorrhage
|
- Fatal brainstem hemorrhage
- Secondary to progression of uncal herniation and resultant tearing of vessels in midbrain/pons |
|

|
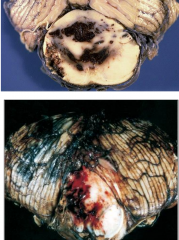
Duret Hemorrhage
|
|
|
Cerebellar Tonsillar Herniation
|
Caused by symmetric expansion of supratentorial contents into posterior fossa or expanding mass lesion in posterior fossa
- Caudal cerebellar structures "tonsils" attempt to escape through foramen magnum - Medullary compression results in cardiorespiratory arrest. |
|
|
Hydrocephalous
|
Enlargement of ventricles associated with increase in CSF volument
|
|
|
Communicating Hydrocephalous
|
- Ventricular system is patent
- Obstruction is frequently at arachnoid villi : may be due to decreased absorption at arachnoid granulations (examples: meningitis, hemorrhage in subarachnoid space, sinus thrombosis) |
|
|
Overproduction of CSF from choroid plexus (papilloma)
|
Another cause of hydrocephalus
|
|
|
Non-communication Hydrocephalus
|
- Obstruction within ventricular system
- Prevents "communication" between ventricles proximal and distal to obstruction |
|
|
Examples of Non-communicating hydrocephalus
|
- Tumor in ventricle blocking flow (ex: at foramen of Monro)
- Congenital malformation (atresia of aqueduct of sylvius) - Thick meninges at base of brain blocking flow |
|
|
Blunt Head Trauma
|
Most common
- associated with acceleration or deceleration forces to head - results in skull fractures, parenchymal injury, vascular injury |
|
|
Penetrating (Missile) Head Trauma
|
Penetration by external object (like a bullet)
|
|
|
Characterization of Trauma
|
- Open vs. Closed
- Focal vs. Diffuse - Primary Damage vs. Secondary Damage |
|
|
Primary Damage related to non-missile head injurt
|
- Scalp Laceration
- Skull Fracture - Cerebral Contusions - Cerebral lacerations - Intracranial hemorrhage - Diffuse axonal injury |
|
|
Secondary Damage related to non-missile head injury
|
- Ischemia
- Hypoxia - Cerebral Swelling - Infection |
|
|
Focal Brain Injury
|
- Typically causes focal neurological deficits/epilepsy
- Scalp contusions and lacerations - Skull fractures - Brain contusions and lacerations - Intracranial hemorrhage - Infection (2') |
|
|
Diffuse Brain Injury
|
- Typically causes coma/ vegetative state
- Diffuse axonal injury - Diffuse vascular injury - Brain swelling - Global brain ischemia |
|
|
Three patterns of skull fractures
|
1. Linear: single fracture line, through entire thickness of skull
2. Comminuted: multiple linear fractures radiate from point of impact 3. Depressed: Bone fragments displaced inward |
|
|
Characteristics of skull fractures
|
- three patterns: linear, comminuted, or depressed
- occur over convexity or base - skin may be open or closed |
|
|
Concussion
|
- Pathophysiologic process induced by traumatic biomechanical forces (aka mild traumatic brain injury)
- Caused by direct or indirect forces to head - Biochemical and physiologic abnormalities occur; usually no structural abnormalities on imaging acutely - Immediate transient neurologic impairment - Constellation of physical, cognitive, emotional, and/or sleep-related symptoms that may or may not involve loss of consciousness - duration is highly variable: several minutes to days, weeks, months, or longer |
|
|
Contusion
|
Superficial bruise of the brain
- usually at crests of gyri - occur overlying rough area of inner skull (orbital, temporal region) - results at point of impact from fall or from direct blow to the head - Small blood vessels, neurons, and glia are damaged - Clinical correlations: deficits correlate with size and location of injury |
|
|
Acute Contusions
|
- Wedge-shaped
- Superficial hemorrhage in cortex and meninges |
|
|
Acute Contusions - Microscopically
|
- Perivascular accumulation of blood
- After hours, brain edema |
|
|
Old Contusions
|
- Orbital surfaces of frontal and/or temporal lobes
- Gyri indented, cavitated, with brown/orange discoloration - Macrophages with hemosiderin, fibrillary astrocytes |
|

|
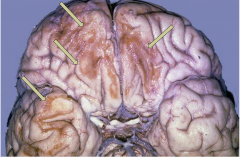
Old contusion
|
|
|
Coup Contusion
|
Contusion that occurs at point of impact
Usually secondary to blow to stationary head May occur at point of impact from fall |
|
|
Contrecoup Contusion
|
- Contusion directly opposite the point of impact
- usually occurs with fall - as the head hits ground a sudden deceleration occurs that causes the brain to "bounce" back and hit the skull on the opposite side |
|
|
Diffuse axonal injury
|
- Deceleration/acceleration injury and/or angular acceleration
- loss consciousness at onset without lucid interval - unconscious or disabled till death - lesser degrees may be compatible with varying severity of neurologic deficits - widespread damage to the axons - mechanical forces disrupt axons |
|
|
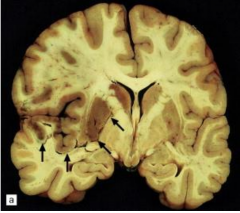
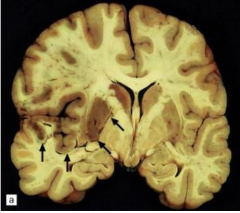
Diffuse axonal injury - gross lesions
|
White matter : corpus callosum, paraventricular white matter, superior cerebellar peduncle, superior colliculi
|
|
|
Diffuse axonal injury - Acute Changes
|
Clusters of petechial hemorrhages and soft hemorrhagic foci
|
|
|
Diffuse axonal injury - Chronic Changes
|
Hydrocephalus ex vacuo, thinned corpus callosum, gray discoloration of white matter
|
|
|
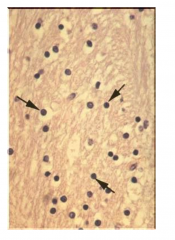
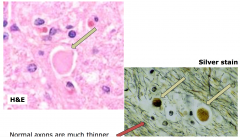
Diffuse axonal injury - microscopic changes
|
- must have microscopic exam to confirm dx
- axons are disrupted; axonal transport continues and causes axonal swellings (organelles and proteins accumulate) |
|
|
Chronology of diffuse axonal injury
|
acute: axonal swellings, positive for beta amyloid protein and silver stains
subacute: microglia and axonal swellings chronic : degeneration of involved fiber tracts |
|
|
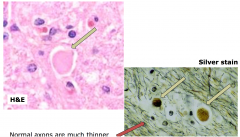
diffuse axonal injury - axonal swellings
|
|
|
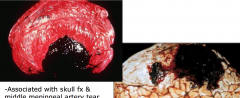
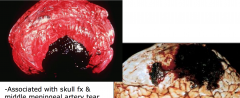
Epidural Hematoma
|
- Associated with skull fracture and middle meningeal tear
- lucid interval between trauma and clinical symptoms - slow accumulation because of adherence between skull and dura |
|
|
Epidural Hematoma
|
|
|
Acute subdural hematoma
|
- Most often nonlocalizing signs: headache, confusion
- tearing of bridging veins extending from subarachnoid space to dura - more common in elderly people with brain atrophy |
|
|
Chronic Subdural Hematoma
|
- Original injury occurred months ago
- Well organized membrane enclosing hematoma - Susceptible to recurrent bleeds from friable vessels in granulation tissue |
|
|
Subarachnoid space hemorrhage
|
Occur from contusions, lacerations, skull base fractures, escape of blood from ventricular system
|
|
|
Post-traumatic hydrocephalus
|
Obstruction of CSF resorption due to subarachnoid space hemorrhage
|
|
|
Chronic Traumatic Encephalopathy
|
- Associated with mild repetitive traumatic brain injury
- Initial impulsivity, aggression, depression, short-term memory loss - Eventually dementia, gait, speech abn, parkinsonism |
|
|
Pathology of Chronic Traumatic Encephalopathy
|
Extensive deposition of tau in the form of neurofibrillary and glial tangles and TDP-43 inclusions
|
|
|
Brain Death
|
- unresponsive to pain/central stimulation
- absence of reflexes - pupillary, corneal, cough, gaga, dolls eye reflex, cold calorics reflex - absence of respirations - positive apnea test with pCO2>60 - T>32.2C (90F) - SBP > 90 |
|
|
Oligodendroglia
|
Myelinates multiple CNS axons (up to 50 each). In Nissl stains, they appear as small nuclei with dark chromatin and little cytoplasm. Predominant type of glial cell in white matter.
- these cells are destroyed in MS - look like fried eggs in H&E staining |
|
|
Schwann Cell
|
Each schwann cell myelinates only 1 PNS axon.
Also promote axonal regeneration. Derived from neural crest. Increase conduction velocity via saltatory conduction between nodes of Ranvier where there are high conce of Na+ channels. |
|
|
Which disease destroys Schwann Cells?
|
Guillain-Barre
|
|
|
Acoustic Neuroma
|
Type of schwannoma.
Typically located in internal acoustic meatus (CN VIII) |
|
|
BBB is formed by what three structures
|
1. Tight junctions between nonfenestrated capillary endothelial cells
2. Basement Membrane 3. Astrocyte Foot Processes |
|
|
Epidural Hematoma
|
- Rupture of Middle Meningeal Artery
- Often secondary to fracture of temporal bone - Lucid interval - Rapid expansion under systemic arterial pressure resulting in a transtentorial herniation - CN III palsy - CT shows biconvex (lentiform), hyperdense blood collection that does not cross suture lines - Can cross falx, tentorium |
|
|
Subdural Hematoma
|
- Rupture of bridging veins
- Slow venous bleeding (less pressure so hematoma develops over time) - Seen in the elderly, alcoholics, blunt trauma, shaken baby - Crescent-shaped hemorrhage that crosses suture lines. - Midline shift - Cannot cross falx, tentorium |
|
|
Subarachnoid Hemorrhage
|
- Rupture of aneurysm or an AVM. Rapid time course. Patients complain of "worst headache of my life".
- Bloody or yellow spinal tap. - 2-3 days afterward risk of vasospasm due to blood breakdown and rebleed |
|
|
Intraparenchymal Hemorrhage
|
Most commonly caused by systemic htn. Also seen with amyloid angiopathy, vasculitis, and neoplasm. Typically occurs in basal ganglia and internal capsule, but can be lobar.
|
|
|
Communicating hydrocephalus
|
Decreased CSF absorption by arachnoid granulations, which can lead to an increase in intracranial pressure, papilledema, and herniation
|
|
|
Normal pressure hydrocephalus
|
Results in increase subarachnoid space volume but no increase in CSF pressure. Expansion of ventricle distorts the fibers of the corona radiata and leads to the clinical triad of urinary incontinence, ataxia, and cognitive dysfunction.
"Wet, wobbly, wacky" |
|
|
Hydorcephalus ex vacuo
|
Appearance of increased CSH in atrophy (alzheimer's disease, adv. HIV, Pick's). Intracranial pressure is normal, triad is not seen.
|
|
|
Non-communicating Hydrocephalus
|
Caused by a structural blockage of CSF circulation within the ventricular system.
|
|
|
What is the most sensitive imaging modality to evaluate for an acute brain infarct?
|
MRI without contrast
|

