![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
Definition of high output failure and ddx |
hyperdynamic state with CO and ¯O2 extraction with pulmonary/peripheral edema because diastolic dysfunction and circulatory overload
§ DDx: 1.anemia, 2.hyperthyroid, 3.AV fistula, 4.Paget’s disease, 5.thiamine deficiency, 6.sepsis |
|
|
Def low output |
o low output – most common; ¯CO (systolic dysfunction), filling pressures (diastolic dysfunction), systemic O2 extraction |
|
|
HF R sided vs L sided |
– useful in acute CHF as gives indication as to which chamber failing § L - Anterior MI: hypotension, pulmonary edema, S3
|
|
|
HF · Systolic vs Diastolic – allows specific tx |
o Diastolic (1/3) |
|
|
PATHOPHYSIOLOGY |
Primary insults in heart failure myocyte loss and volume overload which lead to pump dusfunction |
|
|
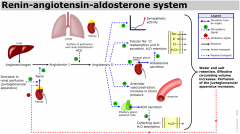
renin angiotensin system |
|
|
|
ETIOLOGY OF CHRONIC HEART FAILURE |
· Things that increase the workload of the heart: |
|
|
ETIOLOGY OF ACUTE DECOMPENSATED HEART FAILURE |
Dietary indiscretions |
|
|
NYHA classification |
I- no limitations - asymptomatic during usual daily activities
II - slight limitation - mild symptoms with ordinary activities (dysp,fatigue,CP)
III-moderate limitation - symptoms noted with minimal activity
IV- severe limitation - symptoms at rest |
|
|
HF CXR |
|
|
|
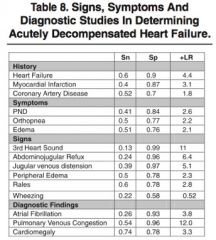
Signs and symptoms HF |
|
|
|
NIPPV what does it do and whats the evidence |
o Increases FRC
o Vital FMR, et al. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema. Cochrane Database of Systematic Reviews 2013, Issue 3. reduced mortality significantly(NNT 13)
Gray A, Goodacre S, et al. Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med 2008;359:142-151 § Severe APE excluded
Li H et al. A comparison of bilevel and continuous posi- tive airway pressure noninvasive ventilation in acute cardiogenic pulmonary edema. Am J Emerg Med. 2013 Sep;31(9):1322-7. PMID: 23928327. \
no diff cpap/bipap |
|
|
Morphine |
No evidence that it venodilates centrally, there are Swan studies to suggest that it increases CVP
|
|
|
Nitrates |
o Mainstay of treatment |
|
|
What level of hypotension should NTG be stopped?
How much to give? |
o Depends on patient; SBP 75 and talking is OK, SBP 90 and decreased LOC not OK
|
|
|
Nitroprusside |
o Potent vasodilator: venous decreases preload, arterial decreases afterload |
|
|
Lasix 1. how does it work? 2. dose and how to give? |
MOA: inhibits 2Na/Cl co-transporter in thick ascending loop of Henle :. increases Na and water excretion and decreases preload; also diuretic induced neurohormaonal changes of PGE2, ANP |
|
|
· ACE-I in acute CHF |
ACE-I good in acute setting for afterload reduction |
|
|
Niseritide |
|
|
|
Treatment of APE in Hypotensive Patients |
1.Fluids 2. Dopamine 3. Dobutamine 4. norepi 5.milrinone |
|
|
Fluids fluids for APE? |
o Clinically, small fluid challenge and monitor response of BP and possible worsening of oxygenation |
|
|
Dopamine - for APE? |
o Low doses: 2-5 ug/kg/min: dopaminergic; renal/splanhnic vasodilation |
|
|
Dobutatmine for APE? |
Mainly B1 agonist, some B2 and some alpha |
|
|
· Norepinephrine |
|
|
|
MI and cardiogenic shock with acute pulmonary edema |
|
|
|
ACEi systolic dysf in HF |
Decrease mortality and hospitalization rates |
|
|
Angiotensin Receptor Blockers (ARBs) systolic dysf in HF |
Used for contraindication or intolerance of ACE-I |
|
|
BetaBlockers in HF? |
Cardioselective: metoprolol, carvidolol |
|
|
Spirnolactone (Aldactone) - sys HF |
· Aldosterone antagonist thus decreases Na+ resorption and increases K+ retention |
|
|
Lasix |
· Symptomatic control, no reduction in mortality |
|
|
Nitroglycerin |
· Symptomatic control, no reduction in mortality |
|
|
Digoxin |
· |
|
|
CCB + what other interventions? |
· CCB have no role in CHF managment |
|
|
ICDs |
|
|
|
Chronic Resynchronisation Therapy (CRT) rationale? |
· Rationale: prolongation of QRS in patients with CHF has been shown to be an independant predictor of adverse outcomes |
|
|
CRT trials? |
CRT trials have looked at CHF patients with EF < 35%, QRS > 120 msec and LBBB and/or evidence of dyssynchrony on echo, normal sinus node function (NOT afib), appropriate chf therapy (ace-i, bb, etc)
|
|
|
Diastolic Dysfunction |
|

