![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
·  ÂWhat is the most common cause of acute nontraumatic symmetric paralysis?
- G |
uillain-Barre syndrome
|
|
|
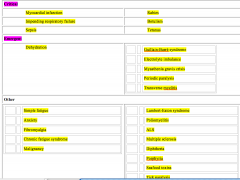
Provide a DDX for weakness (not trauma, strokes, or mass lesions). Consider critical, emergent, and nonemergent neuromuscular and non-neuromuscular causes. (Table 12-1)
|
|
|
|
o ÂWhat two groups of muscles are crucial for maintaining adequate respiration?
|
Upper airway muscles
- Palatal - Pharyngeal - Lingual Inspiratory muscles - Sternocleidomastoids - Diaphragm - Scalenes - External intercostals |
|
|
How does primary weakness of the upper airway muscles present?
|
- Hoarse or nasal voice
- Difficulty swallowing - Cranial nerve palsies - History of descending weakness |
|
|
What is an important differential for primary upper airway muscle weakness?
|
- Botulism
- Myasthenia gravis - Multiple sclerosis |
|
|
What are the nervous inervations for the muscle of inspiration?
|
Sternocleidomastoids o CN XI
Diaphragm o Phrenic nerve (C3,4,5) Scalenes/Intercostals o C4-T8 |
|
|
What is the presentation of primary weakness of the inspiratory muscles?
|
- Tachypnea (compensation for small tidal volumes)
- Paradoxical abdominal movement (diaphragm weakness) |
|
|
In general, which is more worrisome for rapid progression to ventilatory failure, descending or ascending paralysis?
|
des
|
|
|
What PFT measures can be obtained at the bedside that aid in the descision to intubate patients with respiratory muscle fatigue?
|
- Forced vital capacity (<10-12cc/kg: Indication to intubate)
- Negative inspiratory force (<20cm H2O: Indication to intubate) |
|
|
What are the indications for intubation in a patient with weakness and ventilatory insufficiency? (Box 12-3)
|
Severe fatigue
Inability to protect airway or handle secretions Rapidly rising Paco2 Hypoxemia despite supplemental O2 FVC< 12 mL/kg NIF< 20 cm H2O |
|
|
Provide a management algorithm for non traumatic, non stroke weakness. (Figure 12-1)
|

|
|
|
Pattern recognition (Pivotal findings; Table 12-2)
|
to follow
|
|
|
Presentation: C/O: SOB and weakness; O/E: fatigued, respiratory distress, tachypnea, paradoxical breathing, abnormal phonation; Labs: increasing PaCO2, decreasing PFTs
|
Diagnosis: Impending respiratory failure (cause: who cares)
|
|
|
Presentation: C/O: fever, cough, weak; O/E: prostrated, febrile, lung findings; Labs: CXR findings or CBC changes
|
Diagnosis: pneumonia, influenza
|
|
|
Presentation: C/O: Fever, altered mental status, weak; O/E: delirious/demented, no focal findings; Labs: UA or CBC abnormalities
|
Diagnosis: Sepsis, UTI,…
|
|
|
Presentation: C/O: global weakness, sometimes worsened by a meal or exercise; O/E: normal appearance, 4/5 strength, normal reflexes; Labs: electrolyte abnormality
|
Diagnosis: Electrolyte abnormality (i.e. Hypokalemia *including familial periodic paralysis), other metabolic…
|
|
|
Presentation: C/O: preceding viral infection, ascending paralysis; O/E: normal appearance, flaccid paralysis, absent DTRs; Labs: CSF albumino-cytologic dissociation
|
Diagnosis: Guillian-Barre syndrome
|
|
|
Presentation: C/O: global weakness; O/E: normal appearance, 4/5 power, normal reflexes; Labs: normal
|
Diagnosis: Botulism, Lambert-Eaton, Myasthenia gravis
|
|
|
Presentation: C/O: rapidly progressive weakness; O/E: normal appearance, spinal level, hyperreflexic DTRs; Labs:normal
|
Diagnosis: Transverse myelitis
|
|
|
Presentation: C/O: ascending paralysis; O/E flaccid paralysis, ataxia, absent DTRs, imbedded tick
|
Diagnosis: tick paralysis
|
|
|
What is albumin-cytologic dissociation in the CSF?
|
- Protein >400mg/dl, with WBC<10/ml
|
|
|
List physical signs that localize neuromuscular lesion. (Box 12-1)
|
Upper Motor Neuron Lesions
Plantar reflex upgoing Deep tendon reflexes increased Normal to increased muscle tone or spasticity (late finding) Lower Motor Neuron Lesions Plantar reflex normal or absent Deep tendon reflexes decreased, usually absent Decreased to flaccid muscle tone Neuromuscular Junction or Muscle Lesions Plantar reflex normal or absent Deep tendon reflexes usually preserved, may be decreased Decreased to flaccid muscle tone |
|
|
Provide a differential diagnosis of neuromuscular weakness by level of the lesion. (Box 12-2)
|
Upper Motor Neuron Lesions
Transverse myelitis Poliomyelitis Amyotrophic lateral sclerosis (mixed upper and lower) Multiple sclerosis Lower Motor Neuron Lesions Guillain-Barré syndrome Toxic neuropathies – organic solvents, lead, mercury, arsenic, EtOH, steroids, amiodarone, lithium, isoniazid, dapsone Impingement syndromes Diphtheria Porphyria Ciguatera, shellfish, or puffer fish toxin Myoneural Junction/Muscle Fiber Lesions Myasthenia gravis Lambert-Eaton syndrome Botulism Periodic paralyses Electrolyte imbalances Tick paralysis Cephalic tetanus |

