![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
|
What is the most common type of Cardiovascular Disease in adults?
|
Coronary Artery Disease
|
|
|
What is the most common cause or Coronary Artery Disease?
|
Atherosclerosis
|
|
|
What is Atherosclerosis?
|
An accumulation of fats and fibrous tissue in the lining of the arterial blood vessel walls causing a narrowing or complete blockage. It can also be an inflammatory response to an injury to a vessel wall. These injuries can result from Smoking, Hypertension, or DM.
|
|
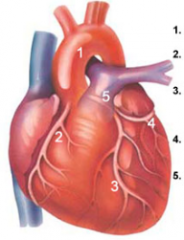
Name 1, 2, 3, 4, & 5.
|
1 - Aorta
2 - Right Coronary Artery 3 - Left Anterior Descending Coronary Artery 4 - Circumflex Coronary Artery 5 - Left Main Coronary Artery |
|
|
What are some modifiable risk factors r/t Atherosclerosis?
|
* Hyperlipidemia
* Tobacco use * Hypertension * DM * Metabolic Syndrome * Obesity * Sedentary Lifestyle |
|
|
What constitutes a diagnosis of Metabolic Syndrome?
|
3 out of the 6 following conditions
* Insulin Resistance * Abdominal Obesity (waist > 35 in women or > 40 in men) * Dyslipidemia * Hypertension * Proinflammatory state (elevated C-reactive protein) * Prothrombotic state (elevated Fibrinogen) |
|
|
What are some non-modifiable risk factors r/t Atherosclerosis?
|
* Family history
* Increasing age * Gender * Race |
|
|
How often should a fasting lipid profile be performed & started at what age?
|
At age 20 a fasting lipid profile should be performed q 5 years. If any abnormal results are found OR if a patient has had an acute event (MI, Percutaneous Coronary Intervention, CABG) in which case lipids should be monitored q 6 weeks until desired levels are achieved and then q 4-6 months.
|
|
|
What are the desired lipid profile values for Cholesterol, HDL, LDL & Triglycderides?
|
Cholesterol: < 200
HDL: > 40 (optimal >60) LDL: < 130 (optimal < 100) Triglycerides: < 150 |
|
|
Define angina pectoris.
|
Chest pain brought about by myocardial ischemia (restricting blood flow & oxygen supply). Basically the oxygen demand exceeds the supply.
|
|
|
Explain the pathophysiology of angina pectoris.
|
Angina is usually caused by atherosclerosis causing a significant obstruction of a major coronary artery. The myocardium, under normal circumstances, requires a large amount of oxygen from coronary circulation, when demand increases and an athersclerotic area exists, circulation cannot increase to meet these demands and ischemia results.
|
|
|
What are some factors that can bring on angina pectoris?
|
* Physical exertion - increasing demand
* Exposure to cold - causing vasoconstriction * Eating heavy metals - shunts blood for digestion, reducing blood flow to the heart & inducing anginal pain. * Stress - releases catecholamines: > BP, > HR, > Myocardial Workload |
|
|
What are 4 types of Anginas?
|
Stable
Unstable Variant Silent |
|
|
What are the characteristics of Stable Angina?
|
Occurs on exertion/stress and is relieved by rest &/or nitroglycerine
|
|
|
What are the characteristics of Unstable Angina?
|
Occurs on exertion, stress; however, It increases in frequency, severity & duration over time.
It is not relieved by rest &/or Nitroglycerine It can have an onset while at rest. |
|
|
What is another name for Variant Angina?
|
Prinzmetal's angina
|
|
|
What are the characteristics of Variant Angina?
|
Onset often occurs90 while at rest
Caused by vasospasm Reversible ST-segment elevation |
|
|
What are the characteristics of Silent Angina?
|
No pain or discomfort occurs
Ischemic changes are visible on ECG |
|
|
How can angina pectoris be asymptomatic?
|
Compensatory collateral circulation allowing blood flow to areas that would otherwise be blocked.
|
|
|
How is the diagnosis of Angina Pectoris made?
|
Exercise or Stress test while monitored by ECG or ECHO.
Cardiac Catheterization Blood Tests (elevated C-Reactive Protein) Pain is relieved by Nitroglycerine |
|
|
What are some non pharmacological treatments for Angina Pectoris?
|
* Diet
* Exercise * Smoking Cessation * Surgical Intervention |
|
|
What are some pharmacologic treatment options for Angina?
|
Nitroglycerin - Coronary Vasodilator
Beta Adrenergic Blockers Calcium Channel Blockers |
|
|
What are some surgical interventions to treat Angina?
|
PTCA - Percutaneous Transluminal Coronary Angioplasty
STENTS CABG |
|
|
Provide some patient education r/t Nitroglycerin.
|
* Admin w/ moist mouth, tongue still, do not swallow saliva until tabled dissolved.
* If severe pain, can crush tablet between teeth to hasten absorption. * Tablets should never be removed from original container and stored in metal/plastic pill boxes. * NTG is inactivated by heat, moisture, air, light, & time so prescription must be renewed q 6 months. * Take before predictable pain causing activities (exercise, stress, stair-climbing, sex). * Admin. 1 tablet q 5 minutes, if pain persists, call for emergency services. * SE: Flushing, throbbing headache, hypotension & tachycardia. * Remain seated during admin. to avoid hypotension or syncope. |
|
|
How does nitroglycerin work?
|
It reduces myocardial oxygen consumption, which decreases ischemia & relieves pain.
|
|
|
How do beta adrenergic blockers help with anginal pain?
|
They reduce myocardial oxygen consumption by blocking beta-adrenergic sympathetic stimulation of the heart resulting in a reduction in HR, slowed conduction of impulses through the SA & AV nodes, decreased BP, & reduced myocardial contractility to balance demands and supply.
|
|
|
What two systems to beta blockers affect & why? What impacts do beta blockers have on these systems?
|
Affects - cardiac & respiratory
Why? Beta receptors are located in the heart & lungs Impacts - Lower HR/BP & Bronchoconstriction (so avoid w/ asthma or COPD pts) |
|
|
What particular group of people might experience asymptomatic angina? Why?
|
DM r/t neuropathy.
|
|
|
What are the cardiac side effects r/t Beta Adrenergic Blockers?
|
Hypotension
Bradycardia Advanced Atrioventricular Block Decompensated Heart Failure |
|
|
What particular group of people might have issues with Beta Adrenergic Blockers? Why?
|
DM because BAB can mask the symptoms of hypoglycemia. Therefore, it is recommended that they check their blood sugars frequently.
|
|
|
How do calcium channel blockers help with angina?
|
Calcium channel blockers increase myocardial oxygen supply by dilating smooth muscle wall of the coronary arteries.
Calcium channel blockers decrease myocardial oxygen demand by reducing systemic arterial pressure and the workload of the left ventricle. |
|
|
What are the most common Beta Blockers used?
|
metoprolol (Lopressor, Toprol)
atenolol (Tenormin) |
|
|
What are the most common Calcium Channel Blockers used?
|
amlodipine (Norvasc)
diltiazem (Cardizem, Tiazac) |
|
|
Which calcium channel blockers should be avoided in a patient with heart failure & which calcium channel blockers are preferred with heart failure?
|
Avoid - nifedipine
Preferred - amlodipine (Norvasc) & felodipine (Plendil) |
|
|
When are calcium channel blockers typically used?
|
*If pts. can't take Beta Adrenergic Blockers
*If pts. experience negative side effects of BAB *If pts. still experience pain despite BAB & Nitroglycerin *After invasive interventional procedures |
|
|
What is the treatment goal for Angina?
|
Prevention & Control of Pain.
|
|
|
What are some possible NANDA's related to Angina?
|
Alteration in comfort, chest pain
Decreased cardiac output Activity intolerance Anxiety Knowledge deficit |
|
|
What medications are often prescribed after the placement of a STENT? How long is this treatment suggested?
|
Anticoagulant - Plavix
Antiplatelet - Aspirin Treatment - Long Term |
|
|
Explain the pathophysiology of an MI.
|
An area of infarction can occur over minutes to hours. As cells are deprived of oxygen, ischemia develops, cellular injury occurs, and the lack of oxygen results in infarction, or the death of cells.
|
|
|
What does acute coronary syndrome mean?
|
It is the continuum from angina to MI.
|
|
|
What are the most common presenting symptoms of patients with MI?
|
Chest pain that occurs suddenly & continues despite rest & medication.
|
|
|
What are the classic S&S of an MI that we should know for NCLEX?
|
Severe, Crushing or Vice-Like pain
Radiates to Jaw, Arms or Back Weakness Hypotension & either Tachy or Bradycardia N/V Pallor Cool/Clammy Skin High Anxiety |
|
|
How is a diagnosis of MI made?
|
Presenting Symptoms
ECG ECHO (if ECG is nondiagnostic) Labs (Troponin T or I, CK & CKMB, Myoglobin) |
|
|
If it is suspected that a patient is presenting with MI, when should the ECG be completed? What would you see on the ECG?
|
Performed & results read within 10 minutes
Inverted T-Wave ST-Segment elevation Abnormal Q Wave |
|
|
What are the 3 Creatine Kinase isoenzymes?
|
CK-MM (Skeletal Muscle)
CK-MB (Cardiac Muscle) CK-BB (Brain Tissue) |
|
|
When does CKMB increase, peak & return to normal in the event of an MI?
|
Increase - within a few hours
Peak - 24 hours normal - 3-4 days |
|
|
When does myoglobin increase, peak & stay elevated in the event of an MI?
|
Increase - 1-3 hours
Peak - 4-12 hours Normal - 12 hours |
|
|
Is an increase in myoglobin specific to an acute cardiac event?
|
No, it is not specific to acute cardiac event; however, it is an excellent parameter for ruling out an acute MI.
|
|
|
What does Troponin do & where is it found?
|
Do - regulates the myocardial contractile process.
Found - A protein found in the myocardium. |
|
|
When does Troponin increase, peak & return to normal in the event of an MI?
|
Increase - within a few hours
Peak - 4-24 hours Return to normal - 1-3 weeks |
|
|
Which test is used most frequently to detect an MI?
|
Troponin is used most frequently. Levels rise quickly & stays up for days to weeks so it works well to detect a recent MI.
|
|
|
What is the prescribed treatment for an MI?
|
ICU w/ Cardiac Monitoring
Antiarrhythmics (Lidocaine) Oxygen Morphine Sulfate Anticoagulants &/Or Thrombolytics (w/in 3-6 h) Vasodilators (ACE Inhibitors) |
|
|
What must you ensure of before administering ACE inhibitors?
|
The patient is NOT hypotensive, hypovolemic, hyponatremic, or hyperkalemic.
|
|
|
What are some nursing diagnoses r/t MI?
|
Chest pain
Decreased cardiac output Acute anxiety High risk for injury; arrhythmias Activity intolerance Alteration in tissue perfusion Knowledge deficit Risk for fluid overload Alteration in nutrition Social isolation Sensory Overload Sleep Deprivation |

