![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
What is hysteresis and why is it seen on the volume - pressure graph of inspiration and expiration?
|
When the path to inflation takes a different course than the path to deflation. This is occurs in breathing because during expiration some intrathoracic airways will be compressed and closed and thus the expiratory change in volume (per pleural pressure) will be different than for inspiration.
|
|
|
why is surfactant important? (what other 2 roles does it have?)
|
(Made by type II pneumocytes that develop in 7th month)
Smaller alveoli have a tendency to collapse in on themselves (water more attracted to itself than to air), If left alone all the little alveoli would coalesce into big ones. Surfactant lowers ST on expiration, AND it has an antibacterial protein component, AND helps prevent water from being drawn into the alveoli. |
|
|
|
|
|
|
|
|
What causes turbulent flow in the airways? How would you treat this and why?
|
An obstruction in the lumen will cause turbulent flow. Once the flow is turbulent the density of the gas will determine it's ability to flow (more dense gases will have trouble navigating the corners of the airways, can't flow). Turbulance will produce stridor.
Tx: put the patient on a mix of 20% O2 and 80% He as this gas is lighter than Nitrogen (will be less dense and have less resistance) |
|
|
Where does the majority of the lung resistance come from? Why is this?
|
From the subsegmental airways. This is because the smaller airways produce resistance that is in parralel and thus lowers the overall resistance of the system. (subsegmental airways are in series)
|
|
|
How is airway resistance affected by lung volume? Significance of this in COPD and emphysema?
|
At high lung volumes the resistance is low, conversely at low lung volumes the resistance is high. Thus, people with COPD will breathe at high lung volumes (hyperinflate) and this can give them near to normal flows.
Emphysema - compliance of lung is high (less tethering of the lungs) so when lungs at high volumes then airways not pulled open! |
|
|
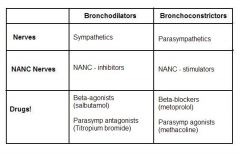
What 4 factors will influence airways resistance?
|
1. Lung compliance, airways are intraparenchymal!
2. Bronchial smooth muscles 3. Secretions 4. # of bronchial glands |
|
|
Of what clinical use is the inspiration limb of a flow-volume curve?
|
It will tell you if there is an extra-thoracic obstruction, by having a V50 that is less than the expiratory V50. Normally, the inspiratory V50 is larger as this portion is entirely effort dependent!
|
|
|
Describe the phenomena of the equal pressure point?
|
As air in the alveoli flows towards the mouth it slowly decreases in pressure, until it eventually becomes equal to the pleural pressure, as the alveolar pressure continues to fall it will become less than the pleural pressure and will get collapsed. In emphysema this equal pressure point occurs distally. In the healthy lung in occurs more proximally where the airways are supported by cartilage.
|
|
|
Describe the location and stimulus for the 3 main sensors of the lungs.
|
1. Central - in the medulla
CO2 will diffuse into the CSF and the sensors here are VERY sensitive to changes in pH. If low they will stimulate ventilation. 2. Peripheral - Carotid bodies and arch Sensitive to pO2, will fire at low amplitude if pO2 starts to fall, becoming very active when pO2<50torr. Potentiated by high pCO2. 3. Lung receptors - on vagus nerve Stretch receptors in the airway smooth muscle that inhibit inflation |
|
|
What 4 things will decrease a person's CO2 response?
|
1. Genetics
2. Narcotics 3. Elite athletes 4. Increased WOB (habituation to higher pCO2) |
|
|
What happens to respiratory control when a pt has chronic hypoventilation?
|
The pCO2 will be chronically elevated and the body will respond with stronger buffering (ie more HCO3). Thus low pO2 becomes the stimulus for breathing
|
|
|
What are 3 possible causes for cheyne-stokes breathing? What is the physiologic basis of it?
|
L ventricular failure, hypoxemia, brain damage.
There is difficulty in the arterial blood reaching the respiratory centres leading to a defect in the feedback mechanism. |
|
|
What is the difference between central and obstructive sleep apnea?
What are 4 consequences of sleep apnea? What is the treatment? |
In central - it's a problem with the pacemaker thus during apnic periods the chest and abdomen don't move.
In obstructive there is paradoxical movement of chest/abdomen during apnea. Sleep apnea causes: pulm & syst HTN, erythrocytosis, daytime somnolence, and L vent failure. Tx: CPAP and wt loss |
|
|
describe the blood supply, nerves and lymph to the pleura.
|
Visceral pleura - bronchial arteries to pulmonary veins
Parietal pleura - systemic Pain fibers are located in the parietal pleura, the diaphragmatic pleura is supplied by the phrenic. Lymph: visceral goes to hilar lymph. Parietal pleura has holes that lead to local lymph nodes. |
|
|
Why are lymphatics so important in regulating the intrapleural fluid?
|
They are the only structures that can absorb proteins, in doing so they regulate the intrapleural oncotic pressure (ie prevent it from rising)
|
|
|
Define Transudate and Exudate
|
T = an ultrafiltrate of plasma (pleural membrane is intact)
E = solute concentrations are higher than in an ultrafiltrate (destruction of pleural membrane) |
|
|
What are the 4 causes of a transudate?
|
1. Cardiac failure
2. Liver failure 3. Nephrotic syndrome 4. Lymphatic obstruction |
|
|
After a thoracentesis, how do you tell if the fluid you got was transudate or an exudate?
|
Look at the amount of LDH, if it's greater than 2x the upper limit of normal serum LDH the fluid must be a transudate!
|
|
|
How does a tension pneumo lead to death?
|
The lung collapses and the mediastinum shifts. If the shift is big enough the veins will get kinked shut and this will lower venous return to heart = lowered cardiac output = low Bp = syncope = death.
Tx: Breathe 100% O2 (as this will be absorbed faster), or suck air out. |
|
|
List 5 non-respiratory functions of the lungs:
|
1. Microcirculation: acts as a filter and as a resevoir. If a shunt bypasses it - can get a cerebral abcess
2. Surfactant: protects lungs from surface forces 3. NO - inflamatory modulator 4. Anti-proteases: protect lung from damage 5. Anti-oxidants: lungs have ++ side reactions to absorb oxidants |
|
|
what are 4 essential pathological components to asthma?
|
1. Bronchospasm - muscles contract
2. Mucous hypersecretion - thick 3. Airway epithelial desquamation - allows the dendritic cells below to be exposed to antigens 4. Airway inflammation - eoisinophilic infiltration |
|
|
What is the permanent long-term consequence of asthma?
|
Airway remodeling - fibrosis below the basement membrane, leading to permanent obstruction
|
|
|
The immune system (lymphocytes) have 2 pathways, which one predominates in asthma?
|
TH1 = infections
TH2 = allergies If you get lots of childhood infections then the TH1 pathways will predominate. If not (childhood is too clean) the TH2 pathway can predominate, leading to asthma. |
|
|
How is ARDS defined?
|
Non-cardiogenic pulmonary edema (transudate)
|
|
|
Describe the 3 phases of ARDS?
|
1. Exudative - increased cap permeability leads to p.edema --> hypoxia/shunt
2. Fibroproliferative - CT proliferates, causing a decrease in compliance, and ventialtion problems 3. Fibrotic - scarring of lung can do damage that in some cases is permanent |
|
|
What ratio is used to determine if a person has ARDS?
How is ARDS treated? (4 main things) Which 3 options have controversial efficacy? |
PaO2 / FiO2 < 200
(if it's < 300 = acute lung injury) Tx: Supplemental O2 --> ventilation (low volumes) permissive hypercapnea Antibiotics nutrition & mouth care Can turn prone, give steroids/surfactant, fluid volume expansion but all have mixed results. |
|
|
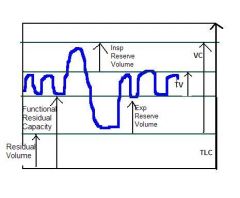
With age what 2 changes might you notice in a person's PFTs?
|
An increase in their RV/TLC, and a decrease in their FEV1/FVC
|
|
|
What are 5 effects of aging on the lungs?
|
1. loss of elastic recoil
2. blunted CO2 response 3. increased risk of infection 4. bigger A-a gradient 5. loss of chest wall muscle fibers |
|
|
With BiPAP, the size of the tidal volume is determined by what?
|
Difference between inspiratory and expiratory pressure and the compliance of the lungs.
|
|
|
What are some of the cons of an ETT tube?
|
- can't phonate
- still a risk of microaspiration - requires sedation - can damage v.cords and airways (if cuff too big - necrosis - detatched trachea) - can't cough |
|
|
What are the 2 ventilator modes?
|
1. Pressure: in this case the size of the TV will depend on pressure differences and lung compliance
2. Volume: in this mode the size of the TV is set, and the pressure will vary depending on compliance |
|
|
What does PEEP stand for? What does it do?
What happens if it's too high? (2) |
Positive End Expiratory Pressure - used to keep airways open. If increased will increase FiO2.
If it is set too high can cause Barotrauma and decreased cardiac return!! |
|
|
Minute ventilation = ?
|
Minute ventilation = TV x Resp rate
|
|
|
If a person has the following ventilator orders:
VC 10/5 RR=12 Vt = 280-320 What does this mean? |
Volume controlled
Driving pressure = 10 cm H20 above the PEEP PEEP = 5 Resp rate = 12 Vt = range of tidal volumes for this constant pressure |
|
|
Why is it dangerous to vent a pt with high FiO2?
|
1. Oxygen toxicity - will damage alv-cap membrane and can cause P edema.
2. oxygen is absorbed too quickly and can cause atelectasis in the alveoli (by being insoluble N acts as scaffolding) |
|
|
What is breath stacking/dynamic hyperinflation and how (3 ways) can you fix it?
|
When a person takes a breath before come to FRC, inhalation before complete exhalation. Will hyperinflate lung and can cause it to blow-up.
Tx: - prolong exp time - b dilators - lower the respiratory rate |
|
|
Why are pt's with ARDS sometimes placed in a prone position?
|
To minimize V/Q mismatch. Putting them prone will hopefully cause blood to flow to the non-dependent portions of the lung where there is good ventilation.
|
|
|
What are the pros (4) and the cons (3) of NO?
|
Pros:
- Very potent vasodilator - only goes to the well ventilated portions of the lungs - very short half life - almost no systemic effects Cons: -expensive - tachyphylaxis (higher doses needed to acheive the same effect) - methemoglobinemia (the Fe in Hgb gets oxidized and can no longer carry O2) |

