![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
Do bacteriostatic or bactericidal drugs work better in a healthy person with a normal immune system?
|
Both of these drugs work just as well in a normal immune system
|
|
|
MOA: Bacteriostatic Agents
|
Inhibit growth and reproduction of bacteria without killing them
|
|
|
Which drugs work with the immune system to rid bacteria from the body?
|
Bacteriostatic drugs
|
|
|
Tetracyclines and Macrolides are what?
|
Bacteriostatic drugs
**Protein Synthesis Inhibitors** |
|
|
These drugs are critical when the immune system is depressed
|
Bactericidal
|
|
|
In general, cell wall agents are what type of drugs?
|
Bactericidal
|
|
|
Penecillin is a bactercidal drug with a time-dependent effect. What does that mean?
|
Once you reach the Minimum Inhibitory Concentration of penecillin it begins and continues killing as long as you are still at MIC.
Upping dosage will not increase penicillin's affect once @ MIC |
|
|
Some bacteria have concentration dependent effects. What does this mean?
|
Must reach a certain concentration of drug in body before it begins to kill bacteria
|
|
|
What type of agent is required for:
-Endocarditis or other endovascular infxn -Meningitis -Infxn in neutropenic cancer patients |
Bactericidal
|
|
|
T/F
All drugs can be harmful at high concentrations |
TRUE
|
|
|
Table for Antimicrobial TI's
|

Therapeutic Index
|
|
|
What does selective toxicity mean?
|
Drug affects only one type of cell (bacteria, etc.) and spares host cells
|
|
|
In order to obtain selective toxicity, what is targeted?
|
Microorganism
-Cell wall -protein synthesis -nucleic acid synthesis **no effect on host cells** |
|
|
What is the therapeutic index?
|
Relates the dose of desired effects to dose of undesired effects
|
|
|
High therapeutic index
|
less likely to be toxic to patients
|
|
|
Low therapeutic index
|
More likely to be toxic to patient
**May require patient monitoring for toxicity** |
|
|
What are some potential side effects of antimicrobial drugs?
|
Allergic Reaction
Toxicity--> renal damage Supression of Normal Flora |
|
|
Suppression of normal flora in the gut can cause what?
|
C. diff -->pseudomembranous colitis
|
|
|
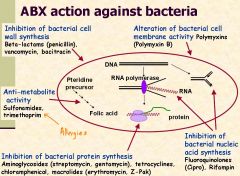
What are the 5 principle targets of antibiotics?
|
1. Inhibition of cell wall synthesis
2. Disruption of cell membrane function 3. Inhibition of protein synthesis 4. Inhibition of nucleic acid synthesis 5. Action as antimetabolites |
|
|
MOA: Agents that inhibit synthesis of bacterial cell walls
|
Inhibit different stages of cell wall sytnthesis
Beta-lactams --> penicillins and cephalosporins |
|
|
What cells have peptidoglycan?
|
Only bacteria have peptidoglycan
It makes up cell walls and is targeted by agents that inhibit cell wall synthesis |
|
|
MOA: Agents that act directly on the cell membrane
|
Increase permeability leading to leakage of intracellular components
|
|
|
Examples of Agents that act directly on the cell membrane
|
polymyxin and daptomycin
|
|
|
Agents that reversibly inhibit bacterial protein synthesis are bacteriostatic/bactericidal
|
Bacteriostatic
|
|
|
Aminoglycosides reversibly/irreversibly inhibit bacterial protein synthesis and are considered bacteriostatic/bactericidal
|
Irreversibly inhibit
Bactericidal |
|
|
MOA: Agents that affect bacterial nucleic acid metabolism
|
**affect bacterial DNA replication**
- inhibit DNA gyrase (eg, fluoroquinolones) **inhibit RNA polymerase** (eg, rifampin) |
|
|
MOA: Inhibition of synthesis of essential metabolites
|
antimetabolites that block essential
enzymes of FOLATE metabolism (eg,trimethoprim and the sulfonamides) |
|
|
What are the essential metabolites of FOLATE metabolism?
|
p-Aminobenzoic acid
Didhydrofolic acid Tetrahydrofolic acid |
|
|
Big summary slide of ABX actions
|
|
|
|
Explain Intrinsic Drug Resistance
|
-Bacteria resistant naturally, without prior exposure to antibiotics
-There is no drug target or drug cannot access target |
|
|
Explain Acquired Drug Resistance
|
Bacteria change or acquire new DNA resulting in resistance
(genetic change)---> Plasmid |
|
|
Why would a drug not reach its target?
|
decreased uptake or increased efflux
|
|
|
Why would a drug not be active?
|
increased rate of inactivation
limited formation of active drug |
|
|
How is a drug target altered?
|
-target deleted
-target modified - acquisition of a resistant form of native, susceptible target |
|
|
What are these examples of?
Altered Porins can prevent certain drugs from entering Increased efflux --> efflux pumps increase capacity to eliminate drug |
Drug does not reach target
|
|
|
Mutation and ABX selection of a resistant mutant are the molecular basis of resistance to:
|
*streptomycin*
- ribosomal mutation *quinolones* - gyrase or topoisomerase gene mutation *linezolid* -ribosomal RNA mutation |
|
|
This mechanism underlies all resistance to M. tuberculosis
|
Mutation and selective pressure
|
|
|
DNA of one bacteria introduced into another ...PHAGE MEDIATED ... same species
Important in the transfer of resistance among strains of S. aureus |
Transduction
|
|
|
DNA uptake from lysed bacteria (related species)
Molecular basis of penicillin-resistance in pneumococci and Neisseria |
Transformation
|
|
|
What is the major mechanism of resistance transfer?
|
Conjugation
|
|
|
Gene transfer through direct cell-to-cell contact
- R determinant DNA plasmids encode drug resistance - Occurs between same strain, different strains,different species - Can transfer multiple drug resistance (MDR) |
Conjugation
|
|
|
Transposons - ‘jumping genes’ -sticky ends
Can move from plasmid to plasmid or plasmid to chromosome These occur in: |
Conjugation
|
|
|
What are the 3 general uses of antibiotics?
|
empirical therapy
definitive therapy prophylactic therapy |
|
|
What are some situations where empiric therapy is highly justified?
|
-Neutropenic, febrile cancer patients
-Community acquired pneumonia |
|
|
Name the antimicrobial therapy:
-organism not yet identified - broad spectrum agent used |
empirical therapy
|
|
|
Name the antimicrobial therapy:
-organism and susceptibilities known -narrow spectrum agent used |
definitive therapy
|
|
|
Name the antimicrobial therapy:
-prevent initial or recurrent infection -spectrum of agent depends on situation |
prophylactic therapy
|
|
|
this is the appearence of a new infection during therapy of a primary infection
|
Superinfection
|
|
|
What are some Disadvantages of
Antimicrobial Combinations? |
- Increased risk of toxicity
- Increased cost *Selection of multi-drug resistant microorganisms* - Eradication of normal host flora |

