![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
104 Cards in this Set
- Front
- Back
|
Neoplastic Disorders of the Lungs
|
1. Bronchogenic Carcinoma
2. Pulmonary Metastases 3. Lymphoma |
|
|
Bronchogenic Carcinoma
|
Arises from the mucosa of the bronchial tree.
- is the common malignant neoplasm. - precise cause unknown but has been closely linked to smoking and to the inhalation of cancer-causing agents such as air pollution, exhaust gases and industrial fumes. |
|
|
Types of bronchogenic carcinoma
|
- squamous carcinoma
- adenocarcinoma - bronchiolar (alveolar cell) carcinoma - small cell (oat cell) carcinoma |
|
|
Squamous Carcinoma
|
typically arises in the major central bronchi and causes gradual narrowing of the bronchial lumen
|
|
|
Adenocarcinomas
|
Usually arise in the periphery of the lung rather than in the lareger central bronchi.
|
|
|
Bronchiolar (alveolar cell) Carcinoma
|
Lease common type of lung tumor.
|
|
|
Small Cell (oat cell) Carcinomas
|
Cause bulky enlargement of hilar lymph nodes, often bilaterally.
|
|
|
Diagnosing Bronchogenic Carcinomas
|
May be diagnosed by detection of cancer cells in teh sputum, but usually requires biopsy of the tumor during bronchoscopy or a needle biopsy.
|
|
|
Radiographic Appearance of Bronchogenic Carcinomas
|
These produce a broad spectrum of abnormalities that depend on the site of the tumor and its relationship to the bronchial tree. Two ways it might appear:
1. discrete mass 2. undetectable and identifiable only by secondary changes |
|
|
Airway obstruction and Bronchogenic Carcinomas
|
Airway obstruction by bronchogenic carcinoma may cause atelectasis of a segment of lung and often leads to pneumonia that develops in the lung distal to the obstructed bronchus.
|
|
|
Air Bronchogram Sign
|
An important radiographic sign differentiating postobstructive pneumonia (bronchogenic carcinoma w/airway obstruction) from a simple inflammatory disease. An air bronchogram sign will not be visible in pneumonia caused by a bronchogenic carcinoma.
|
|
|
Earliest sign of Bronchogenic Carcinoma
|
A unilateral enlargement of the hilum is often the earliest sign of bronchogenic carcinoma. The enlarged hilum represents either a primary carcinoma arising in the major hilar bronchus or metastases to pulmonary lymph nodes from elsewhere in the lungs.
|
|
|
Cavitation
|
Cavitation often occurs in bronchogenic carcinoma. It represents central necrosis of the neoplasm.
|
|
|
Treatment for Bronchogenic Carcinoma
|
Most commonly treated with surgical resection of the lobe. Radiation therapy and chemotherapy may be used as a palliative measure.
|
|
|
Progression of Bronchogenic Carcinomas
|
The prognosis is poor due to direct lymphatic spread of the tumors. Distant metastases most often include the bones. Of all types, small cell carcinomas grow most quickly.
|
|
|
Pulmonary Metastases
|
1/3 of patients with cancer develop pulmonary metastases. It may develop from hematogenous or lymphatic spread from musculoskeletal sarcomas, myeloma, and carcinomas of the breast. Primary lung lesions may metastasize by spread through the bronchial tree.
|
|
|
Radiographic Appearance of Pulmonary Metastases
|
Hematogenous metastases - appear as multiple, relatively well-circumscribed, round or oval nodules throughout the lungs.
Lymphangitic metastases - appears as coarsened interstitial markings that have an irregular contour and are poorly defined. Found most prominently in the lower lobes and may cause pulmonary edema. |
|
|
Treatment of Pulmonary Metastases
|
Treatment includes surgical resection, radiation therapy, and chemotherapy, but all are just palliative.
|
|
|
Bronchogenic Carcinoma Facts
|
Squamous Cell - is centrally located, accounts for 80%, and is slow growing and slow to metastasize so it has the best prognosis. Is mostly what smokers get.
Pulmonary Adenocarcinoma - Has a faster growth rate so prognosis is worse (down to 15% survival rate). Usually non-smokers. Small Cell Carcinoma - Create multiple lesions, is diffuse, so metastasizes very quickly. Prognosis is down to about 10% survival rate. |
|
|
Lymphoma
|
A proliferation of abnormal lymph cells in the lymph system. Can be Hodgkins (pediatric) or Non-Hodgkins.
|
|
|
Indicators of lymphoma
|
Usually creates a "full" sensation in lungs and is found in the mediastinal area. Beginning Indicators:
1. Wide mediastinal area 2. White markings in lungs due to pressure creating retention of fluid. |
|
|
Hodgkins Lymphoma
|
Pediatric lymphoma. Has Reed Steinberg cells which makes it more susceptable to chemo. Higher survival rate (up to 40%).
|
|
|
Non-Hodgkins Lymphoma
|
Not as susceptable to chemo so harder to treat. Usually found in 30-50 yr olds. Often involves other organs besides lymph nodes such as spleen and intestines.
|
|
|
DISORDER: Bronchial Adenoma
|
Location: Glandular structure of major/segmental bronchi
Radiographic Appearance: Peripheral atelectasis (obstruction) with obstructive pneumonia Treatment: Surgical resection |
|
|
DISORDER: Bronchogenic Carcinoma
|
Location: Lung parenchyma
Radiographic Appearance: Solitary lesion, ill-defined including atelectasis with obstruction, hilar enlargement, and cavitation in the upper lung. Treatment: Surgical resection, radiation therapy, and chemo. |
|
|
DISORDER: Pulmonary Metastases
|
Location: Throughout the lungs
Radiographic Appearance: Multiple nodules with sharp margins, Snowstorm nodules, solitary nodule, and coarsened interstitial markings Treatment: All treatments are palliative only - surgical resection, radiation therapy, and chemo. |
|
|
Atelectasis
|
A condition (not a disease) in which there is diminished air within the lung associated with reduced lung volume. Most commonly caused by bronchial obstruction. Air cannot enter that part of the lung supplied by the obstructed bronchus so air is trapped in the lung and then absorbed in the bloodstream so the lung collapses.
|
|
|
Causes of Atelectasis
|
Obstruction due to neoplasm, foreign body, or mucous plug, pneumothorax, pleural fluid, or lung abscess.
|
|
|
Radiographic Appearance of Atelectasis
|
Most common: local increase in density caused by the airless lung.
Direct sign: displacement of interlobar fissures which shift and become bowed, conforming to the contour of the collapsed segment. Indirect Signs: elevation of the hemidiaphragm, displacement of the heart, mediastinum, and hilum toward the atelectatic segment, and compensatory overinflation of the rest of the lung. |
|
|
Treatment of Atelectasis
|
Since it often looks like fluid, they will do a decubitus to make sure it is atelectasis.
To treat, they try to locate and fix the cause and then use spirometry to increase lung volume. |
|
|
Cystic Fibrosis
|
Hereditary disease process of the 7th chromosome which affects mostly caucasians. Cystic Fibrosis is an endocrine disorder where mucous membranes make excessive mucous with high chloride and salt content. This creates an electrolyte imbalance that hardens the mucous in the lungs.
|
|
|
Cystic Fibrosis environment
|
Creates a good environment for bacteria to grow so the heavy mucous is hard to expel and bacterial infection and complications arise. Causes sclerosing of the bronchial passages. Also affects the pancreas and creates sterility in 90% of men who have it.
|
|
|
Signs and Symptoms of Cystic Fibrosis
|
SOB, chronic deep cough, difficulty breathing, lower oxygen sats, decreased growth, fatigue, digestive difficulty. Shortened life expectancy!
|
|
|
Diagnosis of Cystic Fibrosis
|
Diagnosed with the "sweat test" - it identifies excessive chloride and salt in sweat indicating cystic fibrosis. Then they know to look at the 7th chromosome.
|
|
|
Treatment of Cystic Fibrosis
|
Treated with bronchodilators, chest physiotherapy (tapping on chest), and prophylactic antibiotics.
|
|
|
Radiographic Appearance of Cystic Fibrosis
|
Irregular thickening of linear markings throughout the lungs and invariable hyperinflation of the lungs.
|
|
|
ARDS
|
Stands for Adult (or Acute) Respiratory Distress Syndrome - not a disease process! Is severe, acute onset, unexpected, life-threatening respiratory distress in people with no underlying lung disorder. Often called "shock lung".
|
|
|
What happens in ARDS
|
The structure of the lung completely breaks down leading to massive leakage of cells and fluid into the interstitial and alveolar spaces. The structural breakdown results in sever hypoxemia caused by pronounced respiratory impairment in the ability to oxygenate blood.
|
|
|
Radiographic Appearance of ARDS
|
Patchy, ill-defined areas of alveolar consolidation scattered throughout both lungs (bilateral infiltrates - meaning white markings). Can look like pulmonary edema, but unlike PE, the heart remains normal size and there is no evidence of redistribution of blood to upper zones.
|
|
|
Treatment of ARDS
|
Diuretics to decrease fluid load. Oxygen therapy and ventilation to help breathing. May treat with steroids or epinephrine (antihistamine) to decrease inflammation.
|
|
|
Mediastinal Emphysema
|
A rupture in the mediastinal area which traps air in the mediastinum. Can cause damage to the lung tissue because it is pushing the lungs away from the vascular area.
|
|
|
Radiographic Appearance of Mediastinal Emphysema
|
Frontal Chest Radiographs: Lateral displacement of the mediastinal pleura which appears as a long, linear opacity that runs parallel to the heart border but is separted by the air.
Lateral Projection: Air collecting behind the sternum, extending in streaks downward and anterior to the heart. |
|
|
Subcutaneous Emphysema
|
Caused by penetrating or blunt injuries that disrupt the lung and parietal pleura and force air into the tissues of the chest wall. Can hear crepitation (crackling) when papating the skin of the chest.
|
|
|
Radiographic Appearance of Subcutaneous Emphysema
|
Streaks of lucency outlining muscle bundles.
|
|
|
Treatment of Mediastinal and Subcutaneous Emphysema
|
If emphysema is minimal and does not progress then no treatment is needed. If the air does not absorb and increases, surgical resiction to block off the source of air may be required.
|
|
|
DISORDER: Atelectasis
|
Location: Obstruction of segment/lobe or lung collapse
Radiographic Appearance: Local increased density, platelike streaks Treatment: Positioning of the patient with incentive spirometry |
|
|
DISORDER: ARDS
|
Location: Lung structure breakdown
Radiographic Appearance: Patchy, ill-defined areas of consolidation Treatment: Diuretics to decrease fluid build up and oxygen therapy and ventilation |
|
|
DISORDER: Mediastinal Emphysema
|
Location: Air in bronchovascular sheath
Radiographic Appearance: Radiolucency running parallel to heart border Treatment: If minimal, none...Surgical resection to prevent more air escape |
|
|
DISORDER: Subcutaneous Emphysema
|
Location: Air in surrounding muscle bundles
Radiographic Appearance: Air streaks in muscle bundles Treatment: If minimal, none...Surgical resection to prevent more air escape. |
|
|
Pleural Disorders
|
1. Pneumothorax
2. Pleural Effusion 3. Empyema |
|
|
Pneumothorax
|
The presence of air in the pleural cavity resulting in partial or complete collapse of the lung. The increased air in the pleural cavity compresses the lung, causing it to collapse. Caused by rupture from emphysema or spontaneous rupture, trauma, or iatrogenic causes.
|
|
|
Symptoms of Pneumothorax
|
Sudden, severe chest pain and dyspnea.
|
|
|
Radiographic Appearance of Pneumothorax
|
Hyperlucent area in which all pulmonary markings are absent. The radiographic hallmark of pneumothorax is the demonstration of the visceral pleural line which is outlined centrally by air within the lung and peripherally by air within the pleural space. May do a decub to identify.
|
|
|
Treatment of Pneumothorax
|
If large, then a chest tube drainage with suction is used to remove the air and prevent recurrence. It reates a negative pressure again to "reinflate" the lung.
|
|
|
Tension Pneumothorax
|
Emergency in which air continues to enter the pleural space but cannot exit. Causes complete collapse of the lung and depression of the hemidiaphragm. The heart and mediastinal structures shift towards the opposite side. Can be fatal.
|
|
|
Pleural Effusion
|
The accumulation of fluid (plasma) in the pleural space. Most common causes: CHF, PE, infection such as TB, pleurisy, neoplastic disease, and connective tissue disorders. BASICALLY, a vascular obstruction of some sort causing fluid to move into the pleural space.
|
|
|
Radiographic Appearance of Pleural Effusion
|
Blunting of the costophrenic angle and upward concave border of the fluid level. Small pleural effusions are seen best on laterals. Larger amounts of fluid produce a homogeneous radiolucency (whiteness) that may obscure the diaphragm and borders of the heart. Massive effusions may compress the adjacent lung and displace the heart and mediastinum to the opposite side.
|
|
|
Treatment of Pleural Effusion
|
Thoracentesis to remove fluid and finding the cause and fixing it.
|
|
|
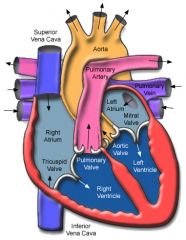
Anatomy of the Heart
|
|
|
Circulation of Blood Through the Heart and Lungs
|
Oxygen-poor blood from the body enters the Right Atrium via the IVC and SVC. This blood flows from the Right Atrium into the Right Ventricle via the Tricuspid valve. The blood leaves the Right Ventricle via the Pulmonary valve and goes to the lungs via the pulmonary artery . Oxygen is exchanged in the capillary beds and then returns to the heart via the pulmonary vein. Oxygen-rich blood enters the left atrium, goes to the left ventricle via the bicuspid (or mitral) valve. It leaves the left atrium via the Aorta valve into the aorta and out to the body.
|
|
|
Pulmonary Embolism
|
Blood clots in the vasculature (pulmonary arteries) of the lungs, usually in the lower lobes due to preferential blood flow to these regions.
|
|
|
Radiographic Appearance of Pulmonary Embolism
|
Cardinal sign of a Pulmonary Embolism is a white "pie-shaped" wedge. The bigger the wedge, the bigger the embolism and therefore it is in a bigger vessel. May be accompanied by edema.
|
|
|
Diagnosis of Pulmonary Embolism
|
To diagnose, the patient is sent to Nuc Med (least invasive) for a perfusion/ventilation scan, to CT to use contrast to see the vasculature (large amount of contrast makes reaction probability high) or to angio, but this is most invasive.
|
|
|
Treatment of Pulmonary Embolism
|
Anticoagulant therapy and thrombolytics.
|
|
|
Pulmonary AV Malformations
|
An abnormal vascular communication from a pulmonary artery to a pulmonary vein. Can cause shunting of blood from arteries to veins so proper oxygen exchange does not occur and this can lead to cyanosis. Common in congenital hemolytic disorders or in trauma.
|
|
|
Radiographic Appearance of AV Malformations
|
Round or oval lobulated soft tissue mass most commonly situated in the lower lobes.
|
|
|
Treatment of AV Malformations
|
A pulmonary angiogram can be done before surgical intervention to prove the diagnosis. A detachable balloon can be placed to block teh flow of blood through the connection.
|
|
|
Acquired Heart Disease
|
1. Coronary Artery Disease
2. Congestive Heart Failure 3. Pulmonary Edema |
|
|
Coronary Artery Disease
|
Narrowing of the coronary arteries causes oxygen deprivation of the myocardium and ischemic heart disease. Narrowing of the lumen is usually due to the deposition of fatty material on the inner arterial wall. Damage to the cell wall (tunica intima) causes platelets to come in to fix it, then cholesterol (LDL) catches on the platelets causing sclerosing of the wall.
|
|
|
What Coronary Artery Disease Does
|
Occlusion of a coronary artery deprives an area of myocardium of its blood supply and leads to the death of muscke cells (mycardial infarction) in the area of vascular distribution. Can lead to CHF and be fatal.
|
|
|
Radiographic Appearance of Coronary Artery Disease
|
Chest radiographs mostly look normal so people are sent to have radionuclide perfusion,intravascular ultrasound, or CT. Definitive test is coronary arteriography.
|
|
|
Treatment of Coronary Artery Disease
|
Angioplasty and stent placement, cholesterol lowering through meds or diet, blood thinners, exercise, and open heart (bypass) surgery.
|
|
|
Congestive Heart Failure
|
CHF refers to the inability of the heart to propel blood at a rate and volume sufficient to provide an adequate supply to the tissues. Cause include cardiac abnormalities, hypertension, or any obstructive process that abnormally increases the peripheral resistance to blood flow.
|
|
|
Radiographic Appearance of Left-Sided Congestive Heart Failure
|
Left-sided heart failure produces an appearance of cardiac enlargement, redistribution of pulmonary venous blood flow (enlarged superior pulmonary veins and decreased caliber of the veins draining teh lower lungs, interstitial edema, alveolar edema (irregular, poorly defined patchy densities) and pleural effusions.
Causes include: coronary heart disease, valvular disease, and hypertension. |
|
|
Radiographic Appearance of Right-Sided Congestive Heart Failure
|
Dilation of teh right ventricle and right atrium is present. Increased pressure may cause dilation of the SVC, widening of the right superior mediastinum, and edema of the lower extremeties. Also, elevation of the right hemidiaphragm due to enlargement of congested liver.
Common causes: pulmonary valvular stenosis, emphysema, and pulmonary hypertension from pulmonary emboli. |
|
|
Cardinal Sign of Congestive Heart Failure
|
For both right and left-sided CHF, cardiomegaly is a cardinal sign due to insufficient cardiac output.
|
|
|
Treatment of Congestive Heart Failure
|
Pull off excess fluid with drugs such as lasix. Low salt diet, no overexertion, and plethora of drugs for comfort measures such as diuretics, beta-blockers, antithrombotic therapy, digitalis, etc...
|
|
|
Pulmonary Edema
|
Abnormal accumulation of fluid in the extravascular pulmonary tissues. Most common cause is an elevation of the pulmonary venous pressure often due to left-sided heart failure.
|
|
|
Pulmonary Edema Cardinal Sign and Radiographic Appearance
|
"Bat Wing" sign - also called a perihilar haze due to the guazy look. It is a diffuse, bilaterally symmetric, fan-shaped infiltration that is most prominent in the central portion of the lungs and fades toward the periphery.
|
|
|
Treatment of Pulmonary Edema
|
Is the same as treatment for congestive heart failure.
|
|
|
Congenital Heart Disease
|
1. Ventricular Hypertrophy
2. Septal Defects 3. Aortic Disorders |
|
|
Ventricular Hypertrophy
|
Enlargement of the right ventricle due to the atrial septal defect which is the failure of the foramen ovale to close after birth. Because the left atrial pressure is usually higher than the pressure in the right atrium, the shunting of blood between the atria from left to right causes increased pulmonary blood flow and overloading of the right ventricle. The right atrium is also enlarged.
|
|
|
Atrial Septal Defect
|
See card on Ventricular Hypertrophy
|
|
|
Ventricular Septal Defect
|
Hole between the two ventricles. Causes increased pulmonary blood flow and increased pulmonary venous return. This leads to diastolic overloading and enlargement of the left atrium and left ventricle.
|
|
|
Patent Ductus Arteriosus Defect
|
The ductus arteriosus is a vessel that extends from the bifurcation of the pulmonary artery to join the aorta just distal to the left subclavian artery. It is supposed to close soon after birth. Due to blood flow from the high pressure aorta to the pulmonary artery, there is increased pulmonary blood flow and excess volume of blood returned to the left atrium and left ventricle. On a radiograph you see enlargement of the left atrium and left ventricle, as well as the central pulmonary arteries. You also see a prominent aortic knob.
|
|
|
Treatment of Septal Defects
|
Small defects may resolve on their own. Larger defects may be treated by the use of prostoglandin synthetase inhibitors to achieve closure. Surgery may be needed to close holes.
|
|
|
Tetralogy of Fallot (Blue-baby syndrome)
|
Four abnormalities:
1. High ventricular septal defect 2. Pulmonary stenosis 3. Overriding of the aortic orifice above the ventricular defect 4. Right ventricular hypertrophy |
|
|
Radiographic Appearance of Tetralogy of Fallot
|
Cardinal Sign is "boot-like" appearance of heart called coeur en sabot which indicates upward and lateral displacement of the apex of the heart.
|
|
|
Treatment of Tetralogy of Fallot
|
Surgical - must repair the ventricular septal defect to repair all of the other problems.
|
|
|
Coarctation of the Aorta
|
A narrowing or constriction of the aorta that most commonly occurs just beyond the branching of the blood vessels to the head and arms.
|
|
|
Radiographic Appearance of Coarctation of the Aorta
|
Rib notching from pressure erosion and missing aortic bulb on chest radiograph.
|
|
|
Treatment of Coarctation of the Aorta
|
Surgical repair to include one of the following three choices:
end-to-end anastomosis, patch aortoplasty, and left subclavian flap aortoplasty. |
|
|
Aortic Aneurysm
|
When the vessel stays dilated and this weakens the walls. Can be caused by high blood pressure. Treatment can be to put a stent in, but also to find the cause and fix it. Visualized as an enlarged aortic bulb.
|
|
|
Dissecting Aneurysm
|
When the tunica intima pulls away from the tunica media. Creates a false lumen between the two tunicas.
|
|
|
Radiographic Appearance of Dissection of the Aorta
|
Due to the blood entering the wall of the aorta and separating the layers, we see a progressive widening of the aortic shadow with an irregular or wavy border. Often seen in those with Marfan's syndrome.
|
|
|
Treatment of Dissection of the Aorta
|
These are fatal if not treated immediately with surgery (grafts) or stents.
|
|
|
Aortic Stenosis
|
Narrowing of the aorta due to plaque formation.
|
|
|
Infectious Disorders of the Heart
|
1. Rheumatic Heart Disease
2. Pericardial Effusion 3. Pericarditis |
|
|
Rheumatic Heart Disease
|
Rheumatic fever is an autoimmune disease that results from a reaction of the patients antibodies against antigens from a previous streptococcal infection. If left untreated, the major damage of the fever is to the valves of the heart (mitral and aortic). The allergic response causes inflammation of the valves. Small nodules develop around the valves and the thickened valves stick together rather than opening properly.
|
|
|
Treatment of Rheumatic Heart Disease
|
Prevention by treating the strep infection is the best approach. Once someone has rheumatic heart disease, it is treated with antibiotics, antiinflammatories, and restricted activity.
|
|
|
Pericardial Effusion
|
The accumulation of fluid within the pericarial space surrounding the heart. May result from bacteria, viruses, or neoplastic involvement.
|
|
|
Radiographic Appearance of Pericardial Effusion
|
Seen as an enlargement of the cardiac silhouette. However, since over 200 ml of fluid must have accumulated to see this, echocardiography is better suited for seeing pericardial effusion.
|
|
|
Treatment of pericardial effusion
|
Treatment depends on the cause. Pericardiocentesis is performed to remove the fluid buildup and a drain may be inserted.
|
|
|
Pericarditis
|
Infection of fluid around the pericardial sac. Use a needle to drain the fluid and antibiotics or antivirals.
|

