![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
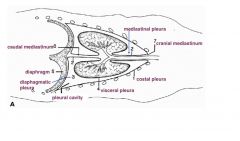
thoracic cavity
|
mechanical source of ventilation (through changes in thoracic volumes.
cavity lined by pleura |
|
|
thoracic cavity bounded by
|
ribcage and intercostal muscles
sternum thoracic vertebra diaphragm thoracic inlet |
|
|
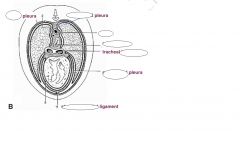
pleura
|
serous membrane covering all surfaces within thoracic cavity
forms mediastinum between two pleural cavities |
|
|
pulmonary or visceral pleura
|
covers surface of all organs and vessels within thorax
|
|
|
parital plura
|
lines inner walls of thoracic cavity
named according to region continous with plulmonary pleura |
|
|
sternopericardial ligament
|
folds of pleura attaching heart to sternum
|
|
|
plica venae cava
|
fold of pleura suspending caudal vena cava
|
|
|
pleural cavities
|
two complete sacs
air tight cavities containing only small amount of fluid |
|
|
mediastinum
|
encloses thymus, heart, trachea, major thoracic vessels and nerves
|
|
|
cranial mediastinum
|
cranial to heart
|
|
|
middle mediastinum
|
containing heart
|
|
|
caudal mediastinum
|
caudal to heart
|
|

|
|
|
|

|
|
|
diaphragm
|
principle muscle of inspiration- used during normal breathing
separates thoracic cavity from abdomen thin sheet of muscle and tendon |
|
|
diaphragmatic attachments
|
transverse processes of the first 2-3 lumbar vertebrae
interal aspect of ribs bear costal arch caudal end of sternum |
|
|
external intercostal and scalaneus muscles
|
only used during forced inspiration
|
|
|
external intercostal muscles run
|
caudoventrally between adjacent ribs
|
|
|
scalenus muscles originate
|
on the transverse process of cervical vertebrae and inset on first few ribs
|
|
|
calenus and external intercostal muscles function
|
draw ribs cranially and laterly-- expansion of throax
|
|
|
expiration
normal |
normal expiration is passive
utilises elastic recoil of lungs explusion of air continues until contraction of thorax reaches point of equilibrium between elastic recoil of lung tissue and resistance to stretching of inspiratory muscles. |
|
|
expiration
active |
occurs when requirment for ventilation elevated
contraction of internal intercostal and abdominal muscles reduces thoracic volume below equilibrium volume |
|
|
internal intercostal muscles run
|
caudodorsally between adjacent ribs and callpase thoracic cavity
|
|
|
abdominal muscles
|
move viscera cranially, pressure on diaphragm
|
|

|

|
|

|

|
|
|
diaphragm innervated by
|
phrenic nerve which orginates from spinal cord in 5th-7th cervical nerves
|
|
|
other respiratory muscles innervated by
|
intercostal nerves
|
|
|
gas flows from an area of
|
high pressure to an area of low pressure
|
|
|
atmospheric pressure
|
760 mm Hg
|
|
|
alveolar pressure
|
760 mm Hg when muscles of ventilation realxed or fixed and glottis open
|
|
|
alveolar pressure decreases during
|
inspiration
|
|
|
alveolar pressure increases during
|
expiration
muscles compress thorax against closed glottis |
|
|
intrapleural thoracic pressure
|
756 mm Hg
|
|
|
transmural pressure gradient
|
difference between alveolar and intrapleural pressure
|
|
|
inspiration steps
|
1. contraction of diaphram, increase volume of thorax
2. expansion of throax- increase volume of pleural cavity 3. drop in pressure in plueral cavity (754 mm Hg) 4. expansion of lungs and drop in intra alveolar pressure 5. airflow down pressure gradient into lungs ( until pressure is equal to atmospheric) |
|
|
expiration steps
|
1. relxation of insipratory muscles
2. decrease in thoracic and lung volume 3. increased intra alveolar pressure (761 mm Hg) due to increase gas molecules 4. airflow down pressure gradient out of lungs |
|
|
contraction of accessory muscles of inspiration together with diaphgram causes an
|
increase in thoracic volume above resting volume and therefore a greater drop in intra alveolar pressure and greater pressure gradient
|
|
|
contraction of muscles of expiration along with relaxation of diaphragm causes
|
a reducing in thoracic and lung volume below resting level and therefore a greater increase in intra alveolar pressure and a greater pressure gradient, and a faster and more complete emptying of lungs
|
|
|
pneumothroax
|
entery of air into pleural space due to trauma to lung or thoracic wall
|
|
|
airflow into throax results in
|
loss of partial vaccum and lung collapse
|
|
|
respiratory dead space
|
the volume of airways that does not participate in gas exchange
|
|
|
anatomical dead space
|
not anatomically adapted for gas exchange ( all airways from nose to terminal bronchioles- conducting airways)
|
|
|
physiological dead space
|
total volume of airways not participating in gas exchange
includes anatomical dead space plus volume of any alevoli with inadquate circulation virtually identical to anatomical dead space in healthy animals |
|
|
pulmonary minute ventilation (ml/min)=
|
tidal volume (ml/breath) X respiratory rate (breaths/min)
|
|
|
alveolar ventilation =
|
(tidal volume- dead space)X respiratory rate
volume of air entering of leaving alveoli in one minute |
|
|
it is more beneficial to .... .... ventiliation by.... .... .... than by... .... rate ( because all additional air taken in is available for gas exchange
|
increase pulmonary ventiliation
increasing tidal volume increasing respiratory |

