![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
|
What is the epithelium of the bronchi? What are some causes of ciliary dyskinesia?
|
Pseudostratisfied ciliated columnar cells with goblet (mucus secreting) cells.
Primary ciliary dyskinesia: AR disorder that renders cilia unable to beat. Secondary ciliary dyskinesia: cigarette smoking. |
|
|
Describe the differences between bronchi and conducting bronchioles.
|
Bronchi: many layers of SMCs, cartilage is present, pseudostratified columnar, densely ciliated, diameter is independent on lung volume.
Bronchioles: 1-3 layers of SMCs, no cartilage, simple columnar with few ciliated cells, diameter depends on lung volume. |
|
|
Where is resistance the lowest in the lung airways?
|
Conducting bronchioles because they are arranged in series. Small airways are aligned in parallel, which reduces resistance greatly (1/= 1/R1+ 1/R2...).
|
|
|
What are the layers of the pulmonary membrane?
|
Surfactant, alveolar epithelium (mostly type I pneumocytes), BM, and capillary epithelium.
|
|
|
What vertebral level does the trachea begin? What vertebral level does the trachea bifurcate?
|
The trachea begins just inferior to the cricoid cartilage, C6, and ends at the sternal angle (T4) level where it bifurcates.
|
|
|
What equation is used to calculate physiological dead space?
|
Vd = Vt * ((PACO2 - PECO2)/PACO2)
Vt = tidal volume PACO2 = PCO2 of alveolar gas PECO2 = PCO2 of expired air |
|
|
How is alveolar ventilation calculated?
|
Alveolar ventilation = (tidal volume - dead space) * breaths/min
|
|
|
Which of the following can be measured by spirometry?
Tidal volume, total lung capacity, functional residual capacity, residual volume, vital capacity? |
Tidal volume and vital capacity. All other volumes listed contain residual volume which cannot be measured.
|
|
|
Use boyles law to explain inspiration of air?
|
PV= k. Increasing lung volume decreases the pressure which allows atmospheric air to flow in the lungs (down a pressure gradient).
|
|
|
What muscles are used in inspiration? Expiration?
|
Inspiration: diaphragm and during exercise or respiratory distress: external intercostals, scalenes, sternocleidomastoids.
Expiration: normally expiration is passive, but during exercise: internal intercostal, innermost intercostal, and abdominal muscles |
|
|
What are the sources of resistance during inspiration?
|
Airway resistance: air molecules colliding with wall = friction
Compliance resistance: expansion of alveolar and paranchyma tissue Tissue resistance: parietal and visceral pleura friction |
|
|
What are the sources of resistance during expiration?
|
Intrathoracic pressure increases which compresses airways and reduces airway diameter. Reduced airway diameter is the primary source of resistance.
|
|
|
Compliance work (resistance) is the energy required to overcome the intrinsic elastic recoil of the lungs. It accounts for 75% of the total work in breathing. Is compliance work increased or decreased in emphysema?
|
Emphysema destroys lung paranchyma. Compliance work is decreases and inspiration is easy. Expiration is difficult.
|
|
|
Does elastance increase or decreased in restrictive lung disease?
|
Elastance will increase in restrictive lung diseases. Elastance = resist deformation. Is is inversely proportional to compliance. E = change in P/change in V.
|
|
|
Explain how emphysema changes the functional residual capacity.
|
Lung compliance (distensibility) is increased in emphysema and the tendency of the lungs to collapse decreases. The lung-chest wall system will seek a higher FRC until the two opposing forces (tendency of the chest wall to expand and collapsing force of lung) reach a new equilibrium.
|
|
|
What is LaPlace's law? What decreases the collapsing force on alveoli?
|
P = 2T/r
P = collapsing pressure on alveolus T = surface tension r = radius of alveolus Surfactant. |
|
|
Describe surfactant and its function.
|
Phophatidylcholine (phospholipid) synthesized by type II alveolar cells and reduces surface tension by disrupting the intermolecular forces between liquid molecules. Lecithin:sphingomyelin ratio greater than 2:1 reflects mature levels of surfactant in the fetus.
|
|
|
What is Dalton's law of partial pressure? What is the partial pressure of oxygen in dry air, inspired air, alveolar air, systemic arterial blood, and venous blood?
|
Partial pressure = total pressure * concentration of gas
O2: 160, 150, 100, 100, 40 CO2: 0, 0, 40, 40, 46 |
|
|
What is Fick's law of diffusion?
|
D = change in P * A * S / T
A = surface area S = solubility coeff. of oxygen T = distant oxygen must diffuse across pulmonary membrane |
|
|
How is V/Q optimized for the most efficient gas exchange (ventilation matches perfusion)?
|
Hypoxia-induced vasoconstriction. Paradoxical vasoconstriction in response to hypoxia.
|
|
|
How does V/Q ratio change in exercise?
|
V/Q at rest is 0.8. During exercise, V/Q approaches 1.0 and is more efficient. Under perfused areas become more perfused due to increased PA blood pressures and under ventilated areas become more ventilated (apices).
|
|
|
In terms of V/Q, whats the difference between a shunt and dead space?
|
In a shunt V/Q approaches 0, e.g. airway obstructions.
In dead space V/Q approaches infinity, e.g. pulmonary embolism occluding a pulmonary artery. |
|
|
An A-a gradient greater than ____ mmHg indicates a pathological condition. How are both PAO2 and PaO2 calculated?
|
30 mmHg
PAO2 = PiO2 - PACO2/R PaO2 is measured with arterial blood gas labs. |
|
|
What is the oxygen saturation in arterial blood? Venous blood?
|
Arterial partial pressure of oxygen in arterial blood is approximately 100 mmHg. At this PP, Hb is 100% bound. In venous blood, the PP of oxygen is 40 mmHg. At this PP, Hb is 75% bound to hemoglobin.
|
|
|
What are some causes of hypoxia with an increase in A-a gradient? Normal A-a gradient?
|
Increased A-a: ventillation, perfusion, or diffusion defects, R-L shunts.
Normal A-a: CNS depression, phrenic nerve lesion, upper airway obstruction (?) |
|
|
How come the pH of venous blood only drops to 7.26 (from 7.4) despite the large offloading of H+ (via CO2 + H20 yielding H + HCO3)? (In other words, who is buffering the H+ so efficiently)
|
Deoxyhemoglobin buffers H+ inside the RBCs.
|
|
|
What is the chloride shift?
|
Cl ions are taken up by RBCs in exchange for HCO3. HCO3 is transported to the lungs via plasma. This is how CO2 is transported to the lungs.
|
|
|
20% of CO2 is transported in the blood by Hb. What is the Bohr effect?
|
Binding of CO2 to Hb decreases the O2 affinity of Hb (facilitates offloading of oxygen).
|
|
|
Where in the medulla is the respiratory center located? What part controls inspiration? Expiration?
|
Reticular formation. Inspiration and the basic rhythm for breathing is controlled by the dorsal respiratory group. Expiration (not active in normal breathing) is controlled by the ventral respiratory group.
|
|
|
What two centers in the pons help to control breathing?
|
Apneustic center: lower pons, stimulates deep and prolonged inspiratory gasp
Pneumotaxic center: upper pons, inhibits inspiration, thus, regulating volume and rate |
|
|
What do central chemoreceptors in the medulla respond to?
|
Central chemoreceptors respond to acidosis (high CO2 levels) in the CSF and in response they increase ventilation (breathing rate).
|
|
|
What do peripheral chemoreceptors in the carotid (via CNIX) and aortic (via CNX) bodies respond to?
|
Decreased PaO2 ( < 60 mmHg), decrease pH, and increase PaCO2.
|
|
|
What is Ondine's curse?
|
Impaired autonomic control of breathing.
|
|
|
What receptors are responsible for Hering-Breuer reflex?
|
Lung stretch receptors. When stimulated by distention of the lungs they produce a reflex decrease in breathing frequency.
|
|
|
Explain why climbers must ascend mountains slowly.
|
Initially, decrease PaO2 stimulates hyperventilation via peripheral chemoreceptors. This causes respiratory alkalosis. The increase pH inhibits the central chemoreceptor induction of hyperventilation. Meanwhile, the kidney excretes HCO3 in response to resp. alkalosis (1-3 days). When pH returns to normal, peripheral chemoreceptors can again stimulate hyperventilation.
|
|
|
What stimulates the J receptors?
|
Engorgement of the pulmonary capillaries stimulate the J receptors which then cause rapid, shallow breathing.
|
|
|
A claustrophobic girl is stuck in an elevator. Her vision becomes blurry and she feels dizzy, why?
|
Hyperventilation decreases PaCO2. PaCO2 is a potent vasodilator for cerebral arteries. The decrease in oxygen delivery to the brain causes these symptoms.
|
|
|
Where are irritant receptors located?
|
Large-diameter airways. Mediate cough, sneeze and bronchoconstriction in response to noxious substances.
|
|
|
What is histotoxic hypoxia? Does supplemental oxygen alleviate symptoms?
|
Inability of cells to us O2 effectively (cyanide poisoning). No.
|
|
|
What are some physiological responses to high altitude (4)?
|
1) Hyperventilation
2) Renal hypoxia induces EPO = polycythmemia 3) Increased anaerobic metabolism increases 2,3-BPG production = right shift of Hb dissociation curve 4) Pulmonary hypoxic vasoconstriction = pulmonary hypertension |
|
|
What is and what causes Biot's breathing?
|
Is: abnormal pattern of breathing characterized by groups of quick, shallow inspirations followed by regular or irregular periods of apnea.
Cause: damage to the medulla oblongata due to strokes or trauma or by pressure on the medulla due to uncal or tentorial herniation. Or opioid use. |
|
|
What is and what causes Cheyne-Stokes breathing?
|
Is: periodic breathing amid higher PaCO2 to stimulate breathing. Characterized by oscillation of ventilation between apnea and tachypnea.
Causes: head trauma. |
|
|
What is Kussmaul's breathing?
|
Bodies response to metabolic acidosis. Rapid, deep breathing to expire CO2. Often occurs in type I diabetic patients experiencing ketoacidosis.
|
|
|
How is FEV1, FVC, and FEV1/FVC affected in asthma and COPD? How about in fibrosis?
|
FEV1 is greatly reduced. FVC is reduced. FEV1/FVC is reduced.
Fibrosis: FEV1 is reduced. FVC is greatly reduced. FEV1/FVC is either normal or increased. |
|
|
What are Clara cells?
|
Clara cells are located in the bronchioles and they secrete a component of surfactant, metabolize toxins, and release Cl ions into the lumen (cGMP-guanylate cyclase ion channel).
|
|
|
What are type I pneumocytes? Type II pneumocytes?
|
Type I pneumocytes are simple squamous epithelium joined by tight junctions (zonula occludens) that line alveoli and have no mitotic capacity.
Type II pneumocytes are large and cuboidal shaped cells. They secrete surfactant (stored in lamellar bodies). They are stem cells that regenerate type I and type II pneumocytes. |
|
|
What is the function of the pores of Kohn?
|
These alveolar pores are found within interalveolar septae and equalize pressure within alveoli.
|
|
|
Name some bronchoconstrictors:
Name some bronchodilators: |
BCs: LTC4, LTD4, PGF, TxA2, and parasympathetic stimulation.
BDs: PGE2, sympathetic stimulation (Beta-2 agonists). |
|
|
Describe the clinical features of pink puffers (emphysema).
|
Thin, barrel-shaped chest, tachypneic, mild hypoxemia, hypocapnia or normocapnia.
|
|
|
Describe the clinical features of blue bloaters (chronic bronchitis).
|
Muscular, barrel-shaped chest, severe hypoxemia with cyanosis, hypercapnia leading to respiratory acidosis, RV failure, and systemic edema.
|
|
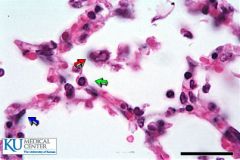
What is the blue arrow? Red? Green
|
Blue = Type I pneumocyte
Green = Type II pneumocyte Red = macrophages |
|
|
How does high altitude cause the production of 2,3 BPG?
|
Hyperventilation causes respiratory alkalosis. Alkalosis activates phosphofructokinase in glycolysis causing increased production of 1,3-BPG which is converted to 2,3 BPG.
|

