![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
200 Cards in this Set
- Front
- Back
|
What is the most common bacteria involved in infection superimposed upon coryza?
|
Strep pneumoniae
|
|
|
Is acute coryza usually due to virus or bacteria?
|
Virus (Adenovirus, rhinovirus, echovirus, etc..)
|
|
|
What is the pathogenesis of hay fever? What the is the clinical name for hay fever?
|
allergic rhinitis
type I hypersensitivity (IgE mediated and degranulation of Mast cell) |
|
|
What is the most common cause of nasal polyps?
How are NSAIDs related to the pathogenesis of nasal polyp formation? What genetic disease is associated with nasal polyps? |
Most common cause: allergic rhinitis
NSAIDS block COX --> more Leukotrine C, D, E4 formation --> bronchoconstrction --> aggravate the allergy associated with cystic fibrosis |
|
|
What are Curshmann spirals? What disease is associated with it?
|
Curshmann spirals are spiral shaped mucus plugs.
Associated with allergic fungal rhinosinusitis (usually due to Aspergillus) |
|
|
What is the most common organism associated with allergic fungal rhinosinusitis?
|
Aspergillus
|
|
|
What populations are most prone to invasive fungal rhinosinusitis? (2)
What is the causative organism? |
Diabetic ketoacidotic pts and immunocompromised
Mucur (wide branching with no septae) |
|
|
What is the most common etiologic agent involved in sore throat?
|
Virus
|
|
|
What is the most common bacteria causing sore throat?
|
Group A strep pyogene
|
|
|
What is the etiology of sinonasal papilloma? What other ENT tumor share the same etiology?
What is the complication of sinonasal papilloma? |
HPV type 6, 11
Also associated laryngeal papilloma can lead to squamous carcinoma (~5%) |
|
|
What are 2 common etiologies of laryngeal nodules? What is the most noticeable Clinical manifestation?
|
smoking and vocal cord strain (e.g. singing)
change in voice |
|
|
A 1 year old boy presents with croup cough, dysphagia, dysphonia, drooling, and destress.
Lateral Xray reveals thumb sign. What is the dx? etiologic agent? |
Epiglottitis
Haemophilus influenza |
|
|
Name 4 etiological agents for Head and neck square cell carcinoma? Which is most common?
|
tobacco (most common)
Alcohol (synergistic with tobacco) EBV HPV |
|
|
What is the most common malignancy of nasopharynx?
|
Nasopharyngeal square cell carcinoma
|
|
|
What is the most common site of square cell carcinoma in the larynx? Which site has the poorest prognosis
|
glottis: most common
infraglottis: least common but poorest prognosis |
|
|
What population is prone to benign otitis externa? malignant otitis externa?
|
Benign: swimmers (aka Swimmer's ear)
Malignant: diabetes mellitus and immunocompromised |
|
|
what are aural polyps? Where are they usually located? result from?
|
Aural polyps are inflammatory polyps located in the middle ear. They are a complication of otitis media.
|
|
|
Describe the pathogenesis of cholesteatoma. What is the morphology cholesteatoma?
|
Chronic otitis media with perforation of tympanic membrane + ingrowth of squamous epithelium from ear canal through perforation --> formation of squamous cell nest that becomes cystic
lined with squamous epithelium and contains keratinous debris with or without cholesterol crystals |
|
|
why is squamous cell carcinoma of the external acoustic meatus fatal?
|
can invade into the brain.
|
|
|
what part of the nose is more prone to epistaxis in children?
|
Anterior portion (anterior bleed at Kiesselbach plexus)
|
|
|
Hypertension can cause bleeding in what part of the nose in elderly?
|
posterior part (bleeding from sphenopalatine or ethmoid arteries)
|
|
|
What is the Ludwig's angina? what is common etiology?
|
Infection of the floor of the mouth.
usually due to strep or staph infection |
|
|
Name 2 most common salivary gland tumors.
|
Pleomorphic adenomas in parotid gland (most common)
Remember the rules of 80: 80% benign, 80% pleomorphic, 80% in superficial lobe Warthrin tumor |
|
|
what is the most common type of influenza virus?
|
type A
|
|
|
What is the difference b/t antigenic shift and antigenic drift?
Which one is worse? |
Antigenic drift: minor changes in neuraminidase and hemagglutinin.
Antigenic shift: major shifts in NA and HA Antigenic shift is worse; can cause pandemic |
|
|
What is Reye's syndrome? Associated with what drug?
|
Post-influenza hepatic encephalopathy (elevated NH3, liver function enzymes, and CPK)
associated with aspirin |
|
|
What agent is associated with "pink eyes"?
|
adenovirus
|
|
|
Is sinusitis commonly due to bacterial or viral cause?
|
Bacterial
|
|
|
What 2 bacteria are associated with sinusitus?
|
Strep pneumonia and hemophilus influenza
|
|
|
When you see a pt with headache and maxillary toothache (teeth are fine though), what do you suspect?
|
sinusitus
|
|
|
What are 2 main types of pulmonary edema?
|
Cardiogenic pulmonary edema (usually due to left heart failure)
non-cardiogenic pulmonary edema (e.g. ARDS, ALI) |
|
|
What are "heart-failure" cells seen in lungs?
In what condition are they found in? |
They are hemosiderin-laden macrophages found in CHRONIC cardiogenic pulmonary edema. they have hemosiderin deposits due to ruptured RBCs.
|
|
|
Name 4 common conditions that can lead to ARDS or ALI. Which is most common?
|
Sepsis (most common)
pulmonary infection trauma aspiration of gastric contents |
|
|
A prematurely born infant presents with cyanosis and dyspnea. AP chest Xray shows extensive opacification. what do you suspect?
|
Hyaline membrane disease (or neonatal respiratory distress syndrome)
|
|
|
Describe pathogenesis of ARDS.
|
injury to the alveocapillary membrane --> 2 things
1. activate alveolar macrophages --> secrete IL-1 and TNF --> recruit neutrophils --> further damage pneumocytes I and II 2. increased capillary permeability --> leakage of protein-rich exudates (esp. fibrin) --> hyaline membrane formation |
|
|
Describe 3 pathologic phases of diffuse alveolar damage (DAD).
|
1. Exudative phase: injury to the alveolocapillary membrane, congestion, edema, inflammation, and hyaline membrane formation
2. Proliferative phase: proliferation of pneumocyte II, endothelial regeneraiton 3. Fibrotic phase: interstitial fibrosis +/- honeycombing |
|
|
What is Hamman-Rich Syndrome?
|
aka Acute interstitial pneumonia
It is an idiopathic DAD presenting in proliferative phase. Has a high mortality rate (>60%) |
|
|
A pt is diagnosed with non-cardiogenic pulmonary edema. If PaO2:FiO2 ratio is 250 mmHg, what is dx? what if it is 150mmHg?
|
Acute lung injury if the ratio is <300mmHg
Acute respiratory distress syndrome if the ratio is < 200mmHg |
|
|
A mechanical ventilator can be used to treat ARDS. What specific settings are recommended? (2)
|
1. low tidal volume at 6 ml/kg
2. high positive end expiratory pressure (PEEP) to keep the alveoli distended |
|
|
What is the difference b/t hyperemia and congestion?
|
Hyperemia is an active, physiological process that pulls plasma to the tissue (e.g. skeletal muscle after exercise)
Congestion is a passive process that pulls plasma to the interstitium due to a pathological process (e.g. left heart failure --> blood backs up --> pulmonary edema) |
|
|
Where is the most common site of DVT formation?
|
Lower exteremities (>95%)
|
|
|
What is cor pulmonale?
what are lines of Zahn? |
Cor pulmonale is a heart failure due to pulmonary problem.
Lines of Zahn are visible lamination of blood and platelet on arterial. They indicate the thrombus was formed when alive. |
|
|
What is the clinical significance of pelvic DVT?
|
can be easily visualized
|
|
|
Are pulmonary infarction usually red or white? why?
|
Red due to dual blood supply (pulmonary and bronchial)
|
|
|
What is a saddle embolus? What is the clinical significance?
|
A large embolus in the bifurcation of the main pulmonary artery. Causes sudden death.
|
|
|
What causes pain with minor breathing in pts with PE?
|
A wedge shaped area of necrosis extend to the pleural wall and inflames. This area rubs against the chest wall when breathing --> causing peritoneal pain.
Usually located at the lower lobe of the lung due to high perfusion rate. |
|
|
How is the PE diagnosed? What criteria are used? What is "PERC"
|
PE is diagnosed based on a number of symptoms and their probability of being correlated with PE.
Wells criteria is used to dx PE. PERC (PE rule out criteria): if qualify, less 1% chance of being diagnosed with PE. |
|
|
what is the name of the defective protein in familial pulmonary artery hypertension?
How does this defect cause pulmonary hypertension? |
Bone morphogenic protein receptor type 2 (BMPR 2).
Causes intimal, medial thickening of the pulmonary artery. |
|
|
Describe the morphology of following vessels in pulmonary hypertension.
1. Main pulmonary artery 2. Muscular artery , low grade 3. Muscular artery, high grade |
1. Main pulmonary artery: athersclerosis
2. Muscular artery, low grade (reversible): intimal thickening due to fibrosis and medial hypertrophy 3. Muscular artery, high grade (irreversible): plexiform lesions (a network of vessels) and angiomatoid lesions (capillaries around the thickened lesion) |
|
|
Name syndromes associated with diffuse alveolar hemorrhage (DAH). (3)
|
Goodpasture's syndrome.
Idiopathic pulmonary hemorrhage (IPH) with hemosiderosis. Vasculitis-associated pulmonary hemorrhage (Microscopic polyangitis, Wegeners granulomatosis, SLE) |
|
|
List risk factors of developing DVT.
|
Virchow's triad:
1. Stasis (immobilization, Right heart failure, sickle cell, morbid obesity) 2. hypercoaguable state (post-op, pregnancy, pregnancy, oral contraceptive, smokers) 3. Endothelial damage (post-op, trauma) |
|
|
You observe diffuse alveolar hemorrhage (DAH) under the microscope. IF shows linear pattern.
What disease do you suspect? |
Goodpasture's
|
|
|
You observe diffuse alveolar hemorrhage (DAH) under the microscope. It also shows hemosiderosis.
What do you suspect? What age group is this common? |
idiopathic pulmonary hemorrage in children.
|
|
|
You observe diffuse alveolar hemorrhage (DAH) under the microscope
What do you suspect if the pt is c-ANCA positive? if p-ANCA positive? |
c-ANCA: Wegerner's granulomatosis
p-ANCA: microscopic polyangitis |
|
|
What is the name of a functional respiratory unit? What are its components?
|
An acinus
A respiratory bronchiole and associated alveolar ducts and alveolar sacs |
|
|
Describe 4 types of overinflation. Are they classfied as emphysema?
|
They are not emphysema
1. Focal emphysema (in CWP): development of focal nodules, which pull the airway open and cause overinflation 2. compensatory overinflamtion: dilation of alveoli but no destruction of septal walls in response to loss of lung substance elsewhere 3. Obstructive overinflation: air trapped due to a mass 4. senile overinflation: reduced elasticity |
|
|
What type of emphysema is this?
Affects the upper zone, only involves the respiratory bronchioles, 90% due to tobacco smoking. |
Centrilobular (centriacinar) emphysema
|
|
|
What type of emphysema is this?
affects the lower zones, involves the entire acinus, main cause is due to alpha-antitrypsin deficiency. |
Panalobular (panacinar) emphysema
|
|
|
What type of emphysema is associated with spontaneous pneumothorax?
|
distal acinar (paraseptal) emphysema
|
|
|
Describe the pathogenesis of emphysema due to smoking.
|

Smoking causes:
1. an increase in free radicals 2. inactivation of AAT --> an increase in neutrophil elastase and macrophage elastase and MMP 3. an increase in chemoattractants --> recruit neutrophils |
|
|
Why does smoking cause emphysema at the respiratory bronchiole level?
|
Inhaled smoking particles accumulate at the bifurcation of respiratory bronchioles.
|
|
|
What are the changes of RV, TLC, and FRC in emphysema patients?
Describe the mechanism behind. |
RV, TLC, and FRC are all increased.
Alveolar wall destruction --> decreased elastic recoil and decreased airway support --> less tethering of the airway also, increased airway caliber during inspiration and decreased caliber during expiration --> air trapping |
|
|
List 3 complications of emphysema. Which one can lead to pneumothorax?
|
Bullae
Blebs: can lead to pneumothorax pulmonary hypertension |
|
|
What are "pink puffers" and "blue bloaters"?
|
Pink puffers are pts suffering from emphysema. They tend to over-ventilate and look pink. They are usually cachexic.
Blue bloaters are associated with chronic bronchitis. They have cyanosis, productive cough, decreased O2 and polycythemia. They appear overweight and deconditioned. |
|
|
What is Reid index? What is it used for?
|
Reid index is a ratio of mucous gland thickness and wall thickness. It is usually <0.4 but >0.5 in chronic bronchitis pts due to hyperplasia of mucous glands.
|
|
|
A pt had productive cough for 3 consecutive months in over 2 years. The lung biopsy shows hypertrophy of mucous glands in the airways. He is a 30-yr pack smoker. what is the dx?
|
Chronic bronchitis
|
|
|
Hyperresponsiveness of the airway is associated with what disorder?
|
Allergic asthma
|
|
|
A pt complains of multiple asthma attacks in the past. But the diagnosis of asthma is uncertain and spirometry is normal. What is the next step?
|
Do methacholine challenge test.
|
|
|
Describe the pathogenesis of allergic asthma.
|
These pts have a strong predisposition to strong Th2 reactions against antigens (type I hypersensitivity)
Th2 cells secrete IL4 and IL 5 --> IgE formation --> Mast cell degranulation and IL-5 secretion IL-5 also activates eosinophils |
|
|
What is eotaxin? What do you observe this?
|
Eotaxin is a chemoattrant secreted from epithelial cells that recruit and activate eosinophils.
they are secreted in the late phase of repeat exposure during asthma attacks. |
|
|
How does chronic use of NSAIDs lead to asthma?
|
NSAIDs block COX and shift the pathway to activate LOX. This will increase synthesis of leukotrienes, which are bronchoconstrictive.
|
|
|
Describe 3 findings of airway remodeling in asthmatic patients.
|
1. Edema, inflammation, and sub-basement fibrosis of airway.
2. hyperplasia of submucosal glands 3. airway SMC hypertrophy and hyperplasia |
|
|
List 3 things you are expected find in sputum of an asthmatic patient.
|
1. eosinophils
2. Charcot-Leyden crystals: diamon-shpaed crystalloids, eosinophil protiens 3. Curshmann spirals: mucus stands |
|
|
What is status athmaticus?
|
severe, prolonged asthmatic attack
associated with pulsus paradoxus Can lead to death |
|
|
What is Kartegener syndrome?
|
absent dynenin arm in cilia --> decreased cilia action in the airway --> impaired airway clearance --> --> airway dilatation
Can lead to bronchietasis |
|
|
What is bronchietasis?
|
Permanent dilatation of bronchi and bronchioles caused by destruction of muscle and elastic tissue secondary to chronic necrotizing inflammation.
|
|
|
What is the most common cause of bronchiectasis in US? worldwide?
|
In US: cystic fibrosis
worldwide: TB |
|
|
Describe spirometry findings in COPD pts.
|
increased RV, TLC, FRC.
Decreased FEV1/FVC ratio (< 0.70) |
|
|
What lung sounds do you expect to hear in chronic bronchitis?
|
Wheezing: due to smaller airways
crackles: due to mucus hypersecretion |
|
|
Differentiate early asthmatic response with late asthmatic response
|
Early asthmatic response is due to bronchospasm with an onset of 15-30 minutes and lasts for 1 to 2 hrs
late asthmatic response is due to inflammation with an onset of 3 to 8 hrs and lasts for 24 hrs. |
|
|
Methylxathines are used as bronchodilators. What is the mechanism? Name 2.
|
PDE inhibitors.
Aminophylline and theophylline |
|
|
Name 4 beta-2 agonists used as bronchodilators. Which one is short-acting?
|
Albuterol: short-acting
Metaproteranol Pirbuterol: short-acting Salmeterol: long-acting |
|
|
Name 3 anticholinergic used in asthma.
|
Atropine
Ipratropium bromide tiotropium |
|
|
What are cromoly and nedocromil. What is the mechanism of action?
|
Anti-inflammatories
MOA: 1. inhibit mast cells 2. inhibit IgE antibodies |
|
|
What are Zafirlukast, Montelukast, and Zileuton?
What is the mechanism of action? |
Leukotriene modifiers.
|
|
|
What is Xolair?
|
Anti-IgE; a bronchodilator
|
|
|
What is the most common side effect of using inhaled steroids in asthma?
|
candida thrush
|
|
|
What radiologic tool is used frequently to diagnose DILD (diffuse infiltrative lung disease)?
|
high resolution CT scan (HRCT)
|
|
|
What are 4 common causes of DILD (diffuse infiltrative lung disease)?
|
Environmental disease (25%)
Sarcoidosis (20%) idiopathic pulmonary fibrosis (15%) autoimmune, collagen vascular disease (10%) |
|
|
A histological section shows patchy interstitial fibrosis, fibroblast foci, and regions of normal lung parenchyma. What pattern of DILD do you predict?
What gross feature would expect at the end of this patterned disease? |
Idiopathic pulmonary fibrosis (IPF)
"honey comb lung" (diffuse interstitial pulmonary fibrosis) |
|
|
Idiopathic pulmonary fibrosis:
Epidemiology? prognosis? treatment? |
predominant in old male smokers
poor prognosis (mean survival is less than 3yrs) lung transplant |
|
|
What are 2 types of pattern in nonspecific interstitial pneumonia (NSIP)?
Do you see fibroblast foci and honeycombing of the lung? prognosis? |
celluar: lymphocyte and plasma cells
fibrosing: diffuse and patchy NO honeycoming and fibroblast foci good prognosis (75-90% 5 yr survival) |
|
|
What are Masson bodies? Where are they usually located? What disease is it associated with?
|
Masson bodies are plugs of organizing fibrotic tissue in the small air spaces (alveolar ducts, alveoli, and bronchioles).
Associated with crytpogenic organizing pneumonia (COP) |
|
|
What group is most affected by nonspecific interstitial pneumonia (NSIP)?
|
mainly females <50 and nonsmokers
|
|
|
Name 3 autoimmune (collage vascular) diseases that have lung involvement?
|
1. systemic sclerosis (scleroderma lung)
2. systemic lupus erythematosis 3. rheumatoid arthritis (rheumatoid lung) |
|
|
What is Caplan syndrome?
|
Presence of rheumatoid nodules and pneumoconiosis
|
|
|
A 50 YO black male presents with dyspnea, chest pain and cough. CXR shows hilar lymphanopathy. Lab shows increased ACE, AST, ALT, AP and serum calcium. Lung biopsy shows non-caseating granuloma. what do you suspect?
|
sarcoidosis
|
|
|
Why is the calcium level high in sarcoidosis?
|
hypercalcemia due to increased secretion of 1,25 Vit D by macrophages.
|
|
|
Hismorphology shows NSIP around the bronchioles, non-caseating granulomas, organizing pneumonia and patient is a farmer. what do you suspect?
|
hypersensitivity pneumonia.
|
|
|
What 3 fibrosing lung diseases are associated with noncaseating granuloma?
|
sarcoidosis
hypersensitivity pnemonitis berylliosis |
|
|
What fungal infection is associated with PIE (pulmonary infiltrates with eosinophilia)?
What vasculitis is associated with PIE? |
Allergic bronchopulmonary aspergillosis.
allergic angiitis and granulomatosis (Churg-Strauss Syndrome) |
|
|
What are 3 syndromes associated with pulmonary eosinophilia?
|
Eosinophilic pneumonia
simple pulmonary eosinophilia (Loffler syndrome) Secondary pulmonary eosinophilia (e.g. tropical, hypersensivity) |
|
|
What are 2 smoking related infiltrative lung diseaess?
What is the common histological feature in both? |
Desquamative interstitial pneumonia (DIP)
Respiratory bronchiolitis-associated interstitial lung disease (RB-ILD) smoker's macrophages |
|
|
Histomorphology shows accumulation of surfactants in alveoli and bronchioles. What infiltrative lung disease pattern do you suspect?
|
Pulmonary alveolar proteinosis
|
|
|
What type of hismophological patterns are shown in scleroderma lung?
|
NSIP and IPF patterns
|
|
|
What type of hismophological pattern is shown in rheumatoid lung?
|
subacute: NSIP pattern
chronic: IPF pattern |
|
|
What type of hismophological pattern is shown in SLE associated infiltrative lung disease?
|
NSIP, IPF, and COP pattern
|
|
|
What is the aerodynamic particle diameter? Why is it important?
|
1-5 microns
able to reach respiratory bronchiole and alveolar ducts |
|
|
Inorganic dusts are associated with what major type of lung disease?
Organic dusts are associated with what 2 major types of lung disease? |
inorganic: fibrotic
organic: asthma and hypersensitivity pnemonitis |
|
|
A pt is diagnosed with Coal Worker's pneumoconiosis (CWP) and histology show rheumatoid nodules with coal dust. What is this syndrome called?
|
Caplan syndrome
|
|
|
What differentiates complicated CWP (coal worker's pneumonconosis) from simple CWP?
|
simple CWP: no significant pulmonary dysfunction and small nodules and macules
Complicated CWP: pulmonary dysfunction is observed and nodules are > 1cm. |
|
|
Silicosis is caused by inhalation of what substance? how about silicatosis?
|
silicosis: silicon dioxide (silica, e.g. quartz)
Silicatosis: silicates |
|
|
What is the most prevalent chronic occupational disease in the world?
|
silicosis
|
|
|
Describe the morphology of acute, massive silicosis. how about chronic?
|
acute, massive: pulmonary alveolar proteinosis (PAP)
chronic: nodular silicosis with whorls of collagen, birefrigent silica particles |
|
|
How is the morphology of silicosis different form silicatosis?
|
Silicatosis has no collagen whorols, less fibrosis, and larger particles
|
|
|
Where do you expect to see opacification in silicosis?
|
nodular opacities in upper zones and "Egg-Shell" calcification in hilar nodes
|
|
|
What pneumoncosis is associated with increased risk of TB? lung cancer? neither?
|
Coal workers pneumonoconiosis: does not increase the risk for TB and lung cancer
Silicosis: increase the risk for both Asbestosis: increase the risk for cancer (especially lung carcinoma and malignant mesothelioma) but no increased risk for TB Berylliosis: increase the risk for cancer (not sure about TB) |
|
|
Those in aerospace and nuclear industries are at risk for what lung disease?
|
berylliosis
|
|
|
What is the histomorphology of chronic cobalt inhalation?
|
giant cell interstitial pneumonia
|
|
|
Name 2 medically relevant forms of asbestos particles. Which one is more pathogentic, why?
|
Serpentine
Amphibole: more pathogenic b/c longer, straighter, stiff, less soluble than serpetine. Also has the aerodyamic particle diameter and long half-life |
|
|
What is the histologic hallmark findings for asbestos-related diseases? describe it.
|
Ferruginous bodies with clear core.
macrophages coat the asbestos particle (clear core) with ferritin. Can be seen with Prussian blue stain. |
|
|
What are parietal pleural plaques in asbestosis? Where are they located?
|
calcified plaques on pleura or diaphragm
|
|
|
What are the criteria for asbestosis? What are gross features of the lung when the disease is advanced?
|
criteria: interstitial pulmonary fibrosis and asbestos bodies
advanced: diffuse interstitial pulmonary fibrosis ("Honeycomb lung") |
|
|
What 2 cancers are associated asbestosis? which one is more common?
|
lung carcinoma (more common)
Mesothelioma |
|
|
Describe the pathogenesis of alveolitis.
|
1. injurious agent in alveolar space
2. inflammatory cells and immune effector cells 3. activation of alveolar macrophages --> secrete IL 8 and LTB4 (chemoattractants) --> recruit neutrophils and secrete fibrogenic factors --> recruit and stimulate fibroblasts and stimulation 4. free radicals from neutrophils injure type 1 pneumocytes --> proliferation of type 2 pneumocytes 5. type 2 pneumocytes produce chemotactic proteins to attract more alveolar macrophages |
|
|
Describe pulmonary function abnormalities in interstitial disease.
|
reduced TLC, RV, FVC
decreased DLCO increased FEV1/FVC arterial hypoxemia due to V/Q shunt |
|
|
Why do sarcodosis patients have anergic response to common skin testing antigens?
|
due to accumulation of CD4+ T cells in lung and their depletion in peripheral circulation
|
|
|
Where is the typical location of bronchopulmonary carcinoid tumor? What cell does the tumor originate from?
|
central, a main-stem bronchus
originate from Kulchitsky cells (neural crest derived) |
|
|
A pt presents with tachycardia, flushing, bronchoconstriction, hemodynamic instability, diarrhea and acidosis. What do you suspect?
|
carcinoid syndrome
|
|
|
Compare and contrast typical and atypical carcinoid tumor in terms of histology and prognosis.
|
Histology:
1. atypical carcinoid cells are more dysplastic (pleomorphic, more mitotic activity, hyperchromatic), hypercellular, and necrotic. 2. they both are vascular --> when disrupted, heavy bleeding Prognosis: typical: 5-10 yr survival: 75-95% atypical: 5-10 yr survival: 40-60% |
|
|
List 5 types of primary lung cancers in decreasing frequency.
|
Adenocarcinoma > squamous cell carcinoma > small cell carcinoma > large cell carcinoma > bronchial carcinoid
|
|
|
What 2 primary lung cancers are highly associated with smoking? which one has the greatest smoking association?
|
Small cell lung carcinoma
Squamous cell lung carcinoma (highest association) |
|
|
List complications from primary lung cancer. (6)
|
"SPHERE"
Superior vena cava syndrome: compression of SVC --> puffiness, blue to purple face, arm and shoulders Pancoast tumor: tumor at the apex of lung --> destroy superior cervical sympathetic ganglion Horner's syndrome: ptosis, miosis, and anhydriosis from pancoast tumor Endocrine (paraneoplastic): Cushing's Lambert-Eaton, PTHrP Recurrent laryngeal symtpoms: hoarseness Effusion (pleural or pericardial) |
|
|
A 70 YO male with a hx of 30 pack-yr smoking presents with cough, hemoptysis, chest pain, and muscle weakenss. CXR shows white opacification located centrally. Lung Bx shows small, dark, blue cells with high mitotic activity.
What is the dx? What accounts for muscle weakness? |
dx is small cell lung carcinoma
muscle weakness due to Lambert-Eaton syndrome (paraneoplastic) |
|
|
A 75 YO male with a hx of 30 pack-yr smoking presents with non-productive cough, chest pain, loss of weight, ptosis, miosis, and anhydrosis. He also broke 3 bones in the past 3 months. Lung bx shows cells with intercellular bridging and keratin pearls. Lab shows high serum calcium.
What is dx? What accounts for ptosis, miosis, and anhydrosis? What accounts for high serum calcium? |
squamous cell carcinoma
Horner's syndrome due to pancoast tumor destryoing superior cervical sympathetic gangion. High serum and osteopenia due to PTH-related protein secretion from the tumor. |
|
|
What is the typical population of adenocarcinoma of the lung?
|
non-smokers and women.
|
|
|
Describe the growth pattern of bronchoalveolar carcinoma.
|
lepidic growth pattern: grows along the alveolar septum; butterfly looking pattern
|
|
|
What primary lung tumors are centrally located? peripherally located?
|
central: typical carcinoid, squamous cell carcinoma
Peripheral: adenocarcinoma, large cell cacinoma Atypical carcinoid: 50% peripheral, 50% central |
|
|
Where is the most common site of metaplastic/dysplastic changes in smokers or people exposed to radon?
|
bronchial bifurcation: smoke particles accumulate the most here
|
|
|
What is the last clinical stage of primary lung carcinoma to be eligible for surgical resection?
|
stage IIIA
|
|
|
When is PET scan indicated for diagnosing primary lung cancer?
What is its limitation? |
PET scan is indicated when a small pulmonary nodule is found and you are not sure whether is benign calcification or tumor.
SPN needs to be at least 1 cm. |
|
|
What is the first step of clinical dx when a small pulmonary nodules (SPN) is found on CXR?
|
Find old CXRs. If SPN has not changed over 2 years, no further eval needed.
|
|
|
What is the most malignant primary lung cancer? least?
|
most maligant: small cell
least maligant: bronchopulmonary carcinoid |
|
|
Mutation of which family of oncogenes is seen almost exclusively in primary lung adenocarcinoma?
|
ras family of oncogenes
K-ras has poor prognosis |
|
|
What is the most common malignant tumor in the lung?
|
metastatic tumors
|
|
|
What primary lung tumor is most associated with paraneoplastic syndrome?
|
small cell lung carcinoma
|
|
|
what two primary lung tumors originate from Kulchistsky cells?
|
bronchopulmonary carcinoid tumor and small cell lung carcinoma
|
|
|
What is preferred treatment of small cell lung carcinoma?
|
chemo and radiation therapy
most cases are not managed surgically |
|
|
What 2 tumor suppressor genes are most frequently mutated with small cell carcinoma?
|
RB and p53
|
|
|
What family of oncogenes are amplified in small cell lung carcinoma?
|
myc family
|
|
|
what is the most frequent site of extra-nodal metastasis in primary lung cancer?
|
adrenal glands
|
|
|
An alcoholic presents with night sweats, fever, and lost 15% of body weight. He had TB 15 years ago. CXR shows cavitations. What TB category is this pt in?
|
post-primary/reactivation TB
|
|
|
What is Ghon complex?
|
calcified focus on parenchyma and lymph node invovlement
|
|
|
What is the most common site of extra-pulmonary involvement in TB?
|
kidney
|
|
|
What major laboratory test will differentiate MTB from other mycobacteria?
|
niacin test
|
|
|
What cell wall component of mycobacteria is responsible for the property of acid-fast stain?
What are 2 other acid fast bacteria? |
mycolic acid
corynebacteria and nocardia |
|
|
What 2 proteins are required for initiation of granuloma formaiton?
What is the source of each? |
ESAT-6 from Mtb and MMP-9 from macrophages
|
|
|
Name 3 drugs that are exclusively anti-TB.
|
INH (isoniazid)
ethambutol pyrazinamide |
|
|
What is the most common adverse of TB drugs?
Which 2 drugs interact synergistically to cause this toxicity? |
hepatotoxicity in INH, rifampin, and pyrazinamide.
INH and Rifampin work sygernistically. |
|
|
What metabolites of INH cause major toxicity?
|
Hydrazones
|
|
|
Name 2 anti-TBs that are eliminated almost exclusively by hepato-biliary excretion.
|
Rifampin and Rifabutin
|
|
|
Rifabutin is often substituted for Rifampin in treating TB in HIV pts, why?
|
lesser potent inducer of p450 enzymes in the liver
|
|
|
What anti-TB drug uses RBC as a depot site, and its common side effect is gout?
|
ethambutol
|
|
|
Rank the primary TB drugs based on their ability to enter CSF in the absence of inflammation.
|
excellent: INH, pyrazinamide
fair/poor: rifampin, ethambutol none: streptomycin |
|
|
What is the major side effect of streptomycin? route of administration?
|
route of administration: IM
ototoxicity --> permanent deafness |
|
|
What are MDR-MtB and XDR-Mtb?
|
MDR-Mtb: mycobacterium TB resistant to INH and rifampin
XDR-Mtb: mycobacterium TB resistance to INH, rifampin + any mmeber of quinolone family and at least one of the anti-TB injectable drugs (kanamycin, capreomycin, amikacin) |
|
|
The following findings indicate what type of pneumonia:
sudden onset, high fever, purulet sputum, pleuritic chest pain, consolidation on CXR, increased WBC |
typical, community acquired pneumonia
|
|
|
The following findings indicate what type of pneumonia:
prodormal sx 4-5 days, low fever, non-purulent cough, interstitial CXR, normal or mild elevation |
atypical, community acquired, pneumonia
|
|
|
What is the common agent that causes lobar pneumonia?
|
strep pnemonia
|
|
|
List 2 ways of preventing community acquired pneumonia.
|
1. influenza vaccine: to prevent secondary bacterial infection
2. pneumococcal vaccine |
|
|
What is the Mantoux test?
|
tuberculin skin test. it can diagnose TB infection in the absence of the active disease
|
|
|
A 20 YO college student walks into the clinic complaining of dry cough, which he had for 3 weeks. You suspect pneumonia. What etiologic is the most likely etiologic agent?
|
mycoplasma pneumoniae
|
|
|
A group of pts complain of high fever, vomiting, diarrhea and dry cough. They all stayed at an old motel for a conference. The motel's condition was very moist. You suspect pneumonia.
What type of pneumonia do you suspect? causative organism? |
atypical, community acquired pneumonia.
Legionella pneumophilia |
|
|
What is the strongest risk factor for nocosomial pneumonia?
|
intubation
|
|
|
What agent causes pneumonia in cystic fibrosis patient?
|
pseudomona aeruginosa
|
|
|
What type of pneumonia is most likely with following associations:
alcoholics, mentally retarded, dysphagia, poor oral hygiene, gingivitis. |
aspiration pneumonia
|
|
|
What normal flora of the tonsils and adenoids produce sulfur-containing pus and can cause aspiration pneumonia?
|
actinomycosis pneumonia
|
|
|
SARS (severe acute respiratory syndrome) is caused by?
|
corona virus
|
|
|
What is the most common systemic fungal agent that can cause chronic pneumonia?
|
histoplasmosis
|
|
|
What fungal agent is associated with following findings:
caseating granuloma, pigeon droppings, chronic pneumonia, seen with India ink stain |
cryptococcosis neoformans
|
|
|
What 2 fungal agents can cause pneumonia in immunocompromised patients?
|
pneumocytis jirveci and mucor species
|
|
|
What fungal agent can cause development of fungus ball in a preexisting cavity?
What is a distinguishing histological feature of this fungus? |
aspergillosis fumigatus
acute branching angle with septae |
|
|
Describe the pleural fluid movement.
Secretion is highest in what region of the lung? how about absorption? |
secreted by parietal pleura (visceral pleural secretion is insignificant) --> pleural space --> parietal lymphatics --> medialstinal lymph nodes
highest secretion in the apex highest absorption at the diaphragm |
|
|
Most common cause of transduative effusion in the lung is? how about exudative effusion (2)?
|
transudative: congestive heart failure
exudative: pneumonia and cancer |
|
|
If you see blunting of the unilateral costopherenic angle on CXR, what are 2 general disorders should you think of? what is the angle is bilateral?
|
unilateral: pneumonia and cancer
bilateral: congestive heart failure |
|
|
What is the criteria for indication for the pleural tab?
|
if the fluid level is more than 10mm on the lateral decubitus view on CXR, then the pleural tab is indicated.
|
|
|
Name the first dx you should think of when you see the following in the pleural tab:
1. 90-100% MNCs 2. 50-60% MNCs 3. PMNs 4. RBCs (name 3) |
1. TB
2. cancer 3. bacterial pneumonia 4. trauma, PE, pulmonary infarction |
|
|
Name the first dx you should think of when you see the following in the pleural tab:
1. <10mg/dl glucose 2. chylous fluid |
1. rheumatoid arthritis
2. lymphomas or obstruction of the lymphatic system |
|
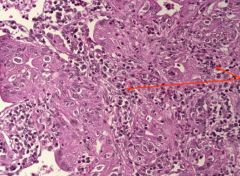
This is a slide of bronchoalveolar carcinoma. What cells are indicated by the arrows? Why are they present?
|
inflammatory cells (lymphocytes and neutrophils) due to a reactive pneumonitis.
|
|
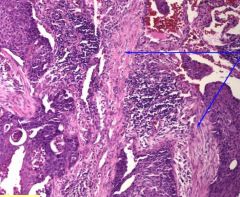
this is a picture of squamous cell carcinoma of the lung. What are they arrows pointing at?
|
Desmoplastic reaction (benign fibrotic tissue) in response to malignant tumor
|
|
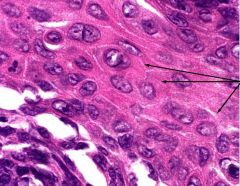
This picture is a lung biopsy from a long time smoker. What type of tumor do you suspect? What are the arrows pointing at?
|
Squamous cell carcinoma of the lung due to presence of intercellular bridges
arrows are pointing at intercellular bridges. |
|
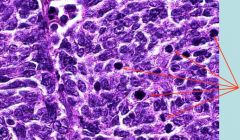
A biopsy from hilar lymph nodes is shown in the picture. This biopsy obtained from a long-time smoker's lung.
What tumor do you suspect? arrows are indicating? |
Small cell lung carcinoma (these are small, blue pleomorphic cells that metastasized to the hilar lymph nodes)
arrows are pointing at mitotic figures. |
|
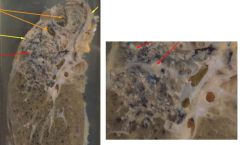
This lung is from a pt died of TB. What are the orange arrows pointing at? red arrows?
|
Orange: central cavitation
red: foci of central caseous necrosis |
|
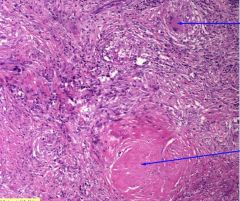
This is a bx of TB lung. What is the upper arrow pointing at? lower arrow?
What part of the lung do you expect to find such lesions? |
Upper arrow: Multinucleated giant cell
lower arrow: caseating granuloma find in the upper zone |
|
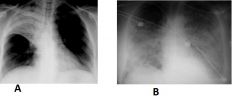
What type of pneumonia is A? B?
Common etiology of A? B? |
A: lobar pneumonia commonly due to strep pneumonia
B: bronchopneumonia classicaly due to nocosomial infection due to virus and secondarily infected with bacteria |
|
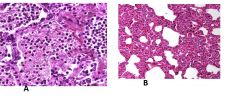
What type of pneumonia is A? how do you know? common etiologic agent?
What type of pneumonia is B? how do you know? common etiologic agent? |
A: bacterial due to pneumonia; presence PMNs, edema; commonly associated with strep pneumoniae
B: insterstitial (atypical) pneumonia; no edema, MNCs, interstitial cellular infiltrates; commonly associated with legionella and mycoplasma pneumoniae |
|
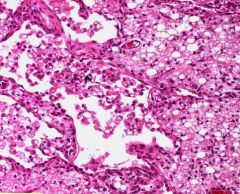
What type of pneumonia is this?
|
Lipid pneumonia
|
|
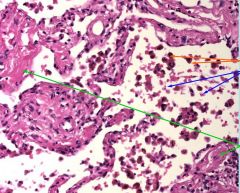
This is a bx of the lung from a pt suffering from dyspnea, orthopnea, and chest pain. CXR shows LVH.
What are orange arrows? blue arrows? Diagnosis? |
Orange arrow: macrophages with hemosiderin
blue arrow: RBC dx: chronic passive congestion |
|
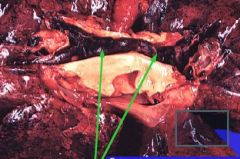
The green arrows are pointing at?
Why is it so fatal? |
Saddle embolus
can cause sudden death |
|

What type of emphysema is shown in A? B?
|
A: centrilobular emphysema due to smoking
B: panlobular emphysema due to AAT deficiency |

