![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
104 Cards in this Set
- Front
- Back
|
What are the different types of classification of pneumonia
|
CAP - community acquired
HAP - hospital acquired PCP - pneumocystis pneumonia (immunosuppressed) Aspiration |
|
|
is pneumonia an upper or lower airway infection?
|
lower
|
|
|
What are the core measures for pneumonia
|
PN 1-7
1-O2 assessment 2 - screening for pna and/or vaccination 3 - blood culture w/in 24 hr PRIOR to antibiotics 4 - smoking cessation 5 - antibiotic w/in 4-8 hrs on arrival 6 - immoCompetent pts antibiotics withing first 24 hrs. 7-Flu vaccine |
|
|
Tx for pneumonia
|
supportive tx: fluids, O2 for hypoxia, antipyretics, antitussives, decongestants and antihistamines
adm of antibiotics if etiologic agent is not identified - use empiric (observation/experiment) antibiotic therapy antibiotics are only for 2ndary bacterial infections |
|
|
s/s of bacterial infection (pneumonia)
|
productive cough (green, yellow, mucous) and increased fever
SOB, chills |
|
|
s/s of viral infection (pneumonia)
|
non productive cough and low fever
|
|
|
onset of HAP is usually....
|
greater than 48 hrs after admission
|
|
|
symptoms of pleural effusion
|
increased fever
tachycardia are common |
|
|
what are nsg diagnosis for pneumonia
******* |
ineffective airway clearance RT
activity intolerance RT risk for deficient fluid volume imbalanced nutrition: less than body requirements deficit knowledge |
|
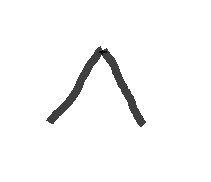
what is this Breath Sound, what is the intensity, pitch and location where heard normally
|

Broncho-vesicular, the inspiration and expiratory sounds are about equal
intensity = intermediate Pitch = intermediate found - between 1st and 2nd inter spaces anterior and between the scapulae over the main bronchus |
|

what is this Breath Sound, what is the intensity, pitch and location where heard normally
|
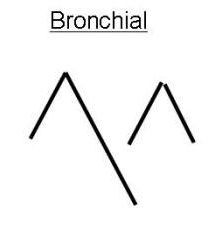
Bronchial
exp last longer than insp. ones intensity - loud pitch - relatively high found- over the manubrium if hear at all |
|

what is this Breath Sound, what is the intensity, pitch and location where heard normally
|

Tracheal
duration- insp and exp are about equal intensity - Very loud pitch - Relatively high Location - over the trachea in the neck |
|

what is this Breath Sound, what is the intensity, pitch and location where heard normally
|

Vesicular
insp last longer than exp intensity - soft pitch - low location - entire lung field except over the upper sternum and between the scapulae |
|
|
during an assessment of a pt with pneumonia what would you be looking for?
|
changes in temperature and pulse
secretions cough tachypnea and SOB changes in physical assessment, CXR and other things elderly pts. |
|
|
What are the assessment items you would look for in an elderly patient with pneumonia
|
fatigue, dehydration and concomitant (Naturally accompanying or associated) heart failure
|
|
|
ABGs on a pt with pneumonia would show
|
hypoxemia
(decreased partial pressure of oxygen in blood, sometimes specifically as less than 60 mmHg, or causing hemoglobin oxygen saturation of less than 90% ) |
|
|
Why are fluids important for pts with pneumonia
|
enables liquidation of mucous trapped in the bronchioles and alveoli, facilitating expectoration. for fever; and non-sensible loss.
|
|
|
why does high fowlers position facilitate cough and comfort.
|
lessens pressure on diaphragm by abdominal organs.
|
|
|
what is a pink puffer
|
barrel chest, emphysema, 02 adequate to oxygenate
but must use accessory muscles to breathe. |
|
|
what is a blue bloater
|
insufficient o2 occurs with chronic bronchitis
and leads to generalized cyanosis and often right sided heart failure (cor pulmonale) |
|
|
Acute Pneumonia may lead to.....
|
Pleural effusion (fluid in pleural space, 40% will get)
Atelectasis super-infection |
|
|
What are 6 different ways to improve airway clearance
|
encourage hydration
humidification by face mask or w/02 Coughing techniques chest physiotherapy O2 therapy administered as pt needs |
|
|
what is pleurisy
|
inflammation of both layers of the pleurae
causes pain and SOB in large effusion |
|
|
what is pleural effusion
|
collection of fluid in the pleural space, usually secondary to another disease process
|
|
|
What is empyema
|
accumulation of thick, purulent fluid in the pleural space.
|
|
|
what are the clinical findings of pleural effusion
|
decreased or absent breath sounds
decrease fremitus (vibratory tremors) dull/flat percussion. Large effusion - Acute Resp. Distress and Tracheal deviation away from affected side |
|
|
What is the nsg mgt for pleural effusion
|
record thoracentesis fluid amount
drain from chest tube pain management positioning on AFFECTED side, splinting |
|
|
what is pulmonary edema
|
accumulation of fluid in lung tissue, alveolar space or both
|
|
|
pathophysiology of pulmonary edema
|
results from increased microvascular pressure from abnormal cardiac function.
(back up into pulmonary system) |
|
|
what are clinical manifestations of pulmonary edema
|
respiratory distress
dyspnea air hunger central cyanosis anxious or agitated fluid in alveoli - FOAM (pt coughs up frothy foamy blood tinged secretions) confusion or stupor crackles in bases progressing to apices of lungs tachycardia O2 falls ABG continue worsening to hypoxemia. |
|
|
mgmt for pulmonary edema
|
correct underlying disorder
if cardiac - L ventricular function is goal vasodilators, inotropic meds, afterload/preload meds or contractility (digoxin), O2, intubation mechanical ventilation. Extremely anxious = morphine to relax and control pain |
|
|
what is afterload
|
the "load" that the heart must eject blood against -
peripheral vascular resistance |
|
|
what is the preload
|
end-diastolic stretch of myofibers
|
|
|
what is VAP
|
Ventilator - associated pneumonia
bacterial pneumonia that develops in pts with acute respiratory failure who have been receiving mechanical ventilation for at least 48 hr. |
|
|
What is the most common form of aspiration pneumonia
|
bacterial infection from aspiration of bacteria from upper airways. S. pneumonia, H. influenzae S. aureus.
|
|
|
what is thoracentesis for
|
it is to remove fluid, to obtain a specimen and to relieve dyspnea and respiratory compromise.
|
|
|
pain on inspiration may be:
pleurisy pleural effusion pulmonary hypertension |
pleurisy
|
|
|
decreased or no breath sounds:
pleurisy pleural effusion pulmonary hypertension |
pleural effusion
|
|
|
dyspnea upon exertion, rest and substernal chest pain may be:
pleurisy pleural effusion pulmonary hypertension |
pulmonary hypertension
|
|
|
normal plueral fluid is ___ to ___ ml
|
5 to 15 mL
|
|
|
What is empyema
|
a pus pocket. accumulation of thick, purulent fluid within the pleural space, often with fibrin development and a walled off area where infection is located.
|
|
|
why does empyema occur
|
complication of bacterial pneumonia or lung abscess
chest trauma hematogenous infection of pleural space nonbacterial infections iatrogenic causes (after thoracic surgery or thoracentesis) |
|
|
Loculated empyema
|
fluid in the pelural space starts thin with low WBC but becomes fibro-purulent and last stage where the lung is enclosed in a thick exudative membrane. loculated empyema.
|
|
|
tx empyema
|
drainage of fluid by needle aspiration
tube thoracostomy with fibrinolytic (clot busters) instilled through chest tube open chest drainage via thoractomy to remove pus |
|
|
mgmt for pulmonary edema if the problem is cardiac in origin would be
|
improvement in left ventricular function
by vasodilators, inotropic meds afterload or preload meds, contractility meds. |
|
|
mgmt for pulmonary edema if the problem is fluid overload in origin would be...
|
diuretics and fluids are restricted.
O2 for hypoxemia, intubation and mechanical vent if necessary. morphine may be prescribed to reduce anxiety and control pain |
|
|
what is MAP stand for
|
mean arterial pressure
|
|
|
What is mean arterial pressure?
|
usually the average. should be over 60 to sustain body organs. normal is 70-110
|
|
|
When you have high pulmonary artery pressure you get hypertrophy and risk of....
|
backing up - then edema. Leads to R HF and death.
|
|
|
After pulmonary artery pressure increases you get a ______ in pulmonary vascular resistance
|
increase
|
|
|
pulmonary resistance affects the ____ ventricular function
|
right
|
|
|
what is idiopathic pulmonary arterial hypertension
|
this is primary hypertension of unknown cause.
rare but most often in women 20-40. usually fatal with 5 years. |
|
|
is pulmonary arterial hypertension primary or secondary
|
secondary. It is due to a known cause either existing cardiac or pulmonary diseases.
|
|
|
what is the prognosis of Pulmonary HTN
|
depends on the severity of the underlying disorder
and the changes in the pulmonary vascular bed. |
|
|
what are common cause of pulmonary artery constriction due to hypoxemia
|
COPD or Cor Pulmonale
|
|
|
what are the symptoms of Pulmonary hypertension
|
hypoxemia
signs of right heart failure (vein distension, edema Tall peaked P waves in inferior leads II, III, AVF) |
|
|
Tx of pulmonary HTN
|
supplemental O2
Fluid limit Diuretics Cardiac glycosides CCB, Prostaglandins, Anticoagulants |
|
|
what is ARDS
|
Acute Respiratory Distress Syndrome a severe form of acute lung injury.
|
|
|
ARDS and aspiration is to Silent as Pulmonary Embolism is to...
|
dead space VQ imbalance
increase V (ventilation) decrease Q (perfusion) |
|
|
pulmonary embolism is to dead space as pneumonia is to...
(also atelectasis, tumor or mucus plug) |
shunting VQ imbalance
decreased V (ventilation) decrease Q (perfusion) |
|
|
Pneumonia is to shunting, as ARDS and aspiration is to...
|
dead space VQ imbalance
decrease V (ventilation) increase Q (perfusion) |
|
|
shunting is a ___________ in ventilation and a ____________ in perfusion ratios
|
decrease in ventilation and increase in perfusion ratios
|
|
|
dead space is a ___________ in ventilation and a ____________ in perfusion ratios
|
increase in ventilation and a decrease in perfusion ratios
|
|
|
silent is a ___________ in ventilation and a ____________ in perfusion ratios
|
decrease in ventilation
decrease in perfusion |
|
|
if the V is equal to Q then it is....
|
normal
|
|
|
if V is > than Q then it is ....
|
dead space
|
|
|
if V is < Q then it is....
|
shunting
|
|
|
if V and Q are both decreased then it is....
|
silent
|
|
|
ventilation is better in zone_________
|
zone 1 or apices
|
|
|
perfusion is better in zone______
|
zone 3 the bases
|
|
|
what is diffusion
|
gas exchanges
|
|
|
what is perfusion
|
blood moving through carrying air
|
|
|
what is ventilation and perfusion.
|
movement of air related to the blood moving through to carry the air
|
|
|
what are examples of airway resistance related to ventilation
|
obstructive diseases COPD and Asthma
|
|
|
if the pt has poor ventilation what would be clinical symptoms
|
lung sounds, movement of chest
|
|
|
if pt has poor perfusion, what would be clinical symptoms to look for
|
capillary refill, cyanosis, skin temperature
|
|
|
which is more serious, ventilation or perfusion failure
|
ventilation
|
|
|
acute respiratory acidosis deteriorates into
|
systemic acidosis
|
|
|
What are complications of V/Q imbalance
|
Organ hypoxia
ventilation failure Acute respiratory acidosis into systemic acidosis result is impaired cellular function |
|
|
what is the resulting complication of V/Q imbalance
|
impaired cellular function
|
|
|
what is ARF
|
acute respiratory Failure
|
|
|
what is acture respiratory failure
|
sudden life threatening deterioration of the gas exchange function of the lung. (not cardiac)
|
|
|
If PaO2 is < 50mmhg you have
|
hypoxemia
|
|
|
PaCO2 > 50 mmhg you have
|
hypercapnia
|
|
|
Someone with Acute Respiratory Failure will have a PaO2 of _____ and a PaCo2 of ____ and a pH of ______-
|
< 50 mm Hg
> 50 mm Hg < 7.35 |
|
|
with acute respiratory failure what is the 1st intervention, then 2nd
|
1st Oxygen
2nd Id underlying cause |
|
|
What is the pathophysiolgy of ARF
|
injury that interferes with the VQ . increased O2 demands
Progressive increase in CO2 and decrease O2 Work of breathing increases with resultant muscle fatigue |
|
|
describe what work of breathing looks like
|
how fast, retractions, positioning, shoulders going up/
|
|
|
What are four categories of ARF
|
Decreased respiratory drive
dysfuntion of the chest wall dysfunction of the lung parenchyma complication of major thoracic, ABD surgeries |
|
|
When most people have a respiratory drive driven by high CO2, COPD is driven by
|
hypoxic drive or low O2
|
|
|
what are the signs and symptoms of ARF
|
Dyspnea - tachypnea
restless (due to low O2 to brain) cyanosis (late sign) dysrhythmia (due to low O2 for heart muscle) altered LOC (brain) |
|
|
What is ventilation failure
|
inability to move air adequately in and out of alveoli = increased CO2 (alveolar hypoventilation)
|
|
|
What is hypoventilation
|
increased CO2
|
|
|
what are causes of Alveolar Hypoventilation
|
Neuromuscular D/O
Respiratory muscle fatigue COPD |
|
|
If you have a problem with ventilation failure, do you have respiratory alkalosis, acidosis, metabolic....
|
acute respiratory acidosis
|
|
|
What is the paco2 and ph of acute respiratory acidosis
|
paco2 of 50mm Hg or greater with pH < 7.3
|
|
|
What are the 2 different failures of ARF
|
ventilation failure and oxygenation failure
|
|
|
what is oxygenation failure
|
impairment in diffusion across alveolar capillary membrane
|
|
|
What are the causes of Oxygenation Failure
|
ARDS
PE Acute Asthma Attack Pneumonia |
|
|
hypoxemia is a PaO2 of
|
< 60 mmHg on room air
|
|
|
if your PaOx is > 80, do you have severe, moderate, mild or normal O2 in blood gasses
|
normal
|
|
|
if your PaOx is < 80, do you have severe, moderate, mild or normal O2 in blood gasses
|
< 80 > 60 is mild
at 60 it is a SatO2 of 90% |
|
|
if your PaOx is < 60, do you have severe, moderate, mild or normal O2 in blood gasses
|
< 60 and > 40 is moderate
|
|
|
if your PaOx is < 40 , do you have severe, moderate, mild or normal O2 in blood gasses
|
< 40 is severe
|

