![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
115 Cards in this Set
- Front
- Back
|
Asthma is thought to occur partly due to the over-activity of sensory nerves. By what mechanism does this happen? |
Sensory nerves normally interact with irritants to vasoconstrict the lungs. Over-activity of these nerves may helps explain asthma's symptoms |
|
|
You have 5x more alveoli than needed for sitting in class. Why is there such an abundance? |
The extra alveoli are used mainly during exercise and the fight/flight response |
|
|
What is the limiting factor to delivering oxygen to the body during exercise?
Respiration rate Alveoli amount Pressure in the pulmonary arteries Heart rate There is no limiting factor |
Heart rate |
|
|
Starting from the smallest airways (the alveoli) and moving out, where can you first find cartilage in the lungs? |
Bronchi |
|
|
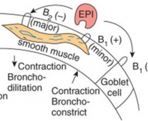
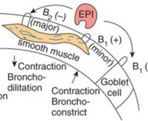
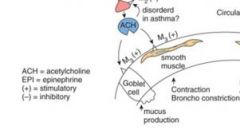
ACh/acetylcholine causes the lungs to perform what functions? |
ACh makes smooth muscles constrict in the lungs and the large airways release mucous |
|
|
ACh acts on what receptor subtype in the lungs to produce smooth muscle contraction? |
M3 receptor (also found on goblet cells to release mucous) |
|
|
If patient X is given a potent beta-1 selective drug, what will happen to X's breathing? |
Nothing is expected to occur. Beta-1 has minimal effects on smooth muscle contraction. |
|
|
Epinephrine is given to a non-asthmatic patient. What is expected to occur regarding their breathing? |
"Easier" breathing via smooth muscle relaxation in the lungs
Even a healthy individual has some tone at rest, thus beta-2 agonists relax smooth muscles and open the airways allowing for easier breathing |
|
|
If a patient is given an anti-cholinergic drug, what is expected to happen to their breathing? |
Easier breathing via blocking M3 receptors and less mucous via blocking of M3 receptors |
|
|
What molecule(s) found in air is/are responsible for increased respiration rates? |
CO2 is the main molecule O2 only increases respiration rates when oxygenated blood levels fall below 50% |
|
|
A healthy individual is moderately exercising. How much will CO2 levels accumulate in this person's blood? |
CO2 is not expected to increase (normally)
A slight increase in CO2 will be countered by increased respiration rates, thus lowering CO2 levels back down to normal |
|
|
---PLEASE IGNORE THIS QUESTION FOR NOW AS THE ANSWER MAY BE WRONG---
The surrounding air has a pressure of 760mmHg. Your lungs happen to produce a force of 753mmHg at this time. Over the next few seconds, will your lungs inflate or deflate? |
---PLEASE IGNORE THIS ANSWER FOR NOW AS IT MAY HAVE BEEN REVERSED---
Inflate (760 - 753 = +7)
Since the force in the surrounding air is greater, it "forces" itself into the area of lower pressure, aka the lungs |
|
|
T/F: Surfactant molecules increase surface tension of the lungs. |
False
They decrease surface tension |
|
|
T/F: Surfactant molecules leave and return to the surface area of the lungs at the same rate. |
False They have different rates during inhalation vs. expiration |
|
|
From the trachea down to the alveoli: where is the movement of air the fastest? |
Trachea |
|
|
Doubling the resistance in the airway has what relationship to the flow rate? (Linear, ^2, ^3, ^4, ^5) |
Linear If you double the resistance, you double the flow rate |
|
|
Decreasing the diameter in the airway has what relationship to the flow rate? (Linear, ^2, ^3, ^4, ^5) |
^4 |
|
|
Which gas exchange occurs quicker in alveoli: O2 or CO2? |
CO2 exchanges quickly in the alveoli while O2 is slower. Under normal conditions, there is enough time for both to exchange effectively. |
|
|
Decreased oxygenated RBC counts can often be traced back to the lungs. What pathophysiological changes in the lung can cause this to happen? |
Could be: Obstruction: air isn't getting to alveoli Lowered gas exchange efficiency: scarring and/or edema can decrease the exchange rate of CO2 and O2 Increased respiration rate: gases don't stay in alveoli long enough for O2 to effectively exchange |
|
|
What is the purpose of measuring FVC, FEV1, etc in a patient? |
Measuring those rates are a diagnostic tool to distingish between different lung diseases |
|
|
T/F: Flow rate while exhaling is "effort-independent" |
Trick question. Flow rate while exhaling is effort dependent when you measure flow rate peaks and FEV1 (aka the initial exhale), but ultimately is independent when considering the AUC and FVC |
|
|
Someone who has low elasticity in their lungs and/or high resistance will have his/her FEV1/FVC increase or decrease compared to baseline? |
Decrease |
|
|
FVC values can be predicted upon what measurements? |
Height and weight |
|
|
Normal and healthy individuals have approximately what FEV1 value/percentage? |
Normal people can exhale approximately 80% of their lung volume in one second |
|
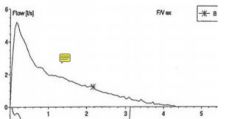
What force determines the peak in this spirometry graph? |
The force of the alveoli contracting |
|

The right graph depicts lung obstruction. According to the graph, where is the obstruction in the lungs? How can you tell? |
The obstruction lies in the small airways. You can tell this by noticing how the graph has a less steep slope, meaning it's taking longer for air to be exhaled during the effort-independent part. And what is the force behind exhaling? The contraction of alveoli |
|
|
Patient X has a FEV1/FVC ratio of 50%. What does this imply? |
Patient X has a lung obstruction of some kind as the normal ratio is 80% If FEV1/FVC is down, you can infer obstruction in the lungs as resistance is up and/or force is down |
|

What can you infer about the lungs according to this graph? |
The shape is normal, but the AUC is reduced. This infers restriction in the lungs - something is stopping your lungs from fully inflating Restriction often is the result of scar tissue in the lungs |
|

Why does someone with restriction in the lungs have a higher FEV1% than a normal person? |
Since FEV1 is the amount of air exhaled in one second, someone with restriction in the lungs can exhale a greater percentage since he/she has less air in his/her lungs to begin with |
|
|
Patient X has a high FEV1/FVC% but a low FVC. What type of lung disease is this? (Obstructive or restrictive) |
Restrictive Something is reducing the lung's ability to fully expand, meaning less air in the lungs |
|
|
What is dyspnea and what lung diseases can it be a symptom of? |
Dyspnea = shortness of breath It is a symptom for many if not all lung diseases |
|
|
What is hypoxia and what lung diseases can it be a symptom of? |
Hypoxia = low oxygenated blood levels It is a symptom for many if not all lung diseases It often is the result of alveoli not effectively absorbing oxygen (V/Q mismatch) |
|
|
What is hypercapnia? Why is this symptom more rare than dyspnea and hypoxia? |
Hypercapnia = elevated CO2 blood levels It is rarer as CO2 is normally easily and quickly exchanged in the alveoli Barbiturates and other sedatives can increase blood CO2 levels |
|
|
CHF has what side of the heart failing? Why does CHF matter in relation to the lungs? |
The left side of the heart It matters as CHF causes increased pressure in the lungs often leading to pressure edema |
|
|
CHF can cause edema due to increased pressure in the lungs. Where in the lungs is this most pronounced? |
The bottom of the lungs More blood flow occurs in the bottom due to gravity |
|
|
Both CHF and pneumonia can cause edema in the lungs. How do these two differ in the production of edema? |
CHF has increased pressure in the lungs causing edema while pneumonia is an inflammatory response. The first step in inflammation is leaky capillaries which cause edema CHF = pressure edema Pneumona = permeability edema |
|
|
Where does most of the edema from pneumonia occur? |
Where the bacterial infection is, since it is an inflammatory response |
|
|
ALI/ARDS can cause edema by what mechanism? (Permeability or pressure) |
Permeability as it is an inflammatory response |
|
|
If someone poorly exchanges oxygen in their alveoli, we may use 100% oxygen. Why is this only a temporary solution? |
100% oxygen is toxic over extended periods of time. Don't give 100% oxygen for more than 5 days |
|
|
What measurement determines if ALI has progressed to ARDS? |
Severity is classified by hypoxemia Also upon the ratio of oxygen inhaled to oxygen in the blood determines disease state. Normal oxygen in air is 21% PaO2/FlO2 - Just know that above 200mmHg is ALI and under 200mmHg is ARDS |
|
|
What are the treatment options for someone with ALI/ARDS? |
Ventilate, treat underlying issues, and restrict fluids to lower edema Since ALI/ARDS is often a symptom of another underlying problem, treat the underlying problem such as pneumonia |
|
|
What physical changes happen to the lung in restrictive diseases? |
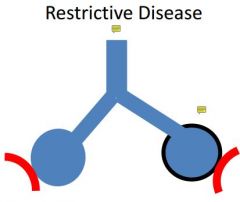
Often fibrosis/connective tissue forms around the alveoli and restrict them from expanding fully |
|
|
Fibrosis is the end result of chronic inflammatory diseases. What happens to the lungs? |
The lungs have connective tissue/scars form around the alveoli and other sites where damage has occurred. |
|
|
Normal breathing has air flow through the bottom portion of the nose/nasal cavity. Where does sniffing send air? |
Sniffing sends air upwards and to the back where the olfactory tissue is |
|
|
Sinuses have little function today. What is/was thought to be the evolutionary purpose behind sinus cavities? |
They may reduce weight in the skull or act has a defensive mechanism (if someone hit that area, nothing was damaged) Nowadays they just get infected a lot |
|
|
There is a lot of blood supply to the nose/nasal cavity. What are the advantages and disadvantages to this? |
Advantages: it heats and humidifies the incoming air Disadvantages: easy to get a bloody nose, if blood vessels expand it reduces the room for air to flow through |
|
|
Does ACh cause the nose to increase, decrease, or do nothing to mucous output? |
Increase mucous output |
|
|
What role do alpha-1 agonists have in reducing sinus congestion? |

Alpha-1 agonists act directly on the sinus itself to reduce blood flow and shrink the sinus |
|
|
What role do alpha-2 agonists have in reducing sinus congestion? |

Alpha-2 agonists decrease the blood flow to the sinus, as well as the entire nose. Thus alpha-2 agonists have many side effects |
|
|
Rhinorhea involves increased mucous production (often watery). Stimulation of what glands may cause this to happen? |
Cholinergic stimulation to the submucosa glands causes increased mucous production as well as plasma being pushed out of the blood. |
|
|
Nasal congestion, over-production of mucous and tissue swelling all lead to obstructive air flow. Decongestants work in which of these causes? |
Nasal congestion and possibly tissue swelling depending on location and severity |
|
|
Despite its name, the rhinovirus isn't typical of most viral infections. What makes the rhinovirus unique compared to most viruses? |
It isn't cytotoxic and doesn't damage cells like many viruses do. You still get the inflammatory response however. The rhinovirus likes to chill in the epithelium |
|
|
How many days will a typical cold take to resolve? When are symptoms most severe? |
Shouldn't take longer than about 10 days to resolve Symptom severity occurs around day 3 and brings coughing and constant throat clearing |
|
|
What mechanisms cause cough during a cold? |
Mechanical stimulation (mucous production/weight) Chemical stimulation (often by inflammatory mediators) The sensory nerves also may be more easily excited |
|
|
How effective is cough-suppressant therapy on the prevention of cough? |
Minimally effective to no effect at all. |
|
|
For someone with a common cold, how does an anti-histamine relieve symptoms? |
Histamine does not play a major role in colds, thus anti-histamines won't have much effect. They may stop a runny nose, but won't relieve many other symptoms Expectorants and cough suppressants are equally ineffective |
|
|
If you buy a decongestant, what receptor sub-types might it act upon? (Such as mu opioid receptors, which is obviously wrong) |
They act as alpha agonists. Depending upon the drug it may act upon alpha-1 and/or alpha-2 receptors Both alpha 1 & 2 agonists shrink/constrict vessels, while alpha-2 agonists also shrink the sinus tissue |
|
|
How long should one use a local decongestant (like nasal sprays) maximally?
What is the reasoning behind this max time useage? |
No more than 3 to 5 days
Using longer than 5 days can result in rebound congestion and nasal toxicity |
|
|
Which is more likely to cause nasal toxicity: an alpha-1 selective agonist or an alpha-2 selective agonist? |

Alpha-2 drugs are more likely due to constricting all blood vessels, rather than just the sinus area |
|
|
In theory dextromethorphan may help suppress a cough (even though at the usual dosages it isn't effective). How does DXM stop coughing mechanistically? |
It increases the threshold for induction of coughing via the CNS |
|
|
How effective are expectorants in the common cold? |
At the indicated dosages, guanfenesin has not been shown to greatly decrease the viscosity of mucus |
|
|
Anti-histamines are generally ineffective for cold symptoms.
Why are first generation anti-histamines like diphenhydramine more likely to suppress coughing than second generation anti-histamines? |
First generation anti-histamines can cross the BBB and have CNS effects like sedation.
Sedatives like whiskey also may help reduce coughing via similar mechanisms. |
|
|
How do sinuses become congested if they are isolated air-filled cavities? |
There are tiny ducts that if they become blocked, form a vacuum in the sinus.
Using a decongestant can help open the duct back up and release the vacuum |
|
|
The rhinovirus causes about what % of common colds? |
50% |
|
|
Why isn't there a vaccine for the common cold when there is one for the flu? |
Way too many viruses (over 200) can cause common colds
Common cold symptoms aren't severe either |
|
|
What is the difference between primary and secondary transmissions of the common cold?
What age group accounts for 75% of these viral infections? |
Primary - direct contact with virus and self-inoculation
Secondary - inhalation of aerosols that contain the virus
Children account for the majority of infections |
|
|
Why are flu shots given in the fall? |
The majority of flu cases happen from December to March, thus fall vaccinations provide the most protection |
|
|
Each question should be answered separately for both the cold and the flu:
When do infections occur mostly in the calendar year?
How is daily functioning impacted?
What are the symptoms? |
Cold - Sept, Oct and early spring Flu - Dec-March
Cold - no impact on daily function Flu - impaired daily function
Cold - sore throat, runny nose, congestion, cough, sneezing Flu - All of the cold symptoms + myalgia, fatigue, fever, sweating and chills |
|
|
How can you distinguish a cold from allergic rhinitis? From sinusitis? |
Allergic rhinitis often has clear post-nasal drip and red/itchy eyes
Sinusitis often has impaired taste/smell, facial pain in a specific area, and don't respond to decongestants |
|
|
How can you distinguish the cold from: Otitis media? Asthma symptoms/ Pneumonia or bronchitis? A bacterial throat infection? |
Otitis media - ear symptoms such as popping, loss of hearing, dizziness, etc
Asthma symptoms - dyspnea
Pneumonia or bronchitis - chest tightness, dyspnea, productive coughing and a persistent fever
Bacterial throat infection - swelling of lymph nodes |
|
|
T/F: Common colds are a self-care contraindication in pregnancy. |
Tricky question. It may be contraindicated depending upon trimester. If in doubt, contact PCP
For all intensive purposes: True |
|
|
What are non-drug "therapies" to help with common cold symptoms? |
Adequate rest Eating well Increase fluid intake Increase humidification Nasal irrigation products
The two most important are adequate sleep and increasing fluid intake |
|
|
T/F: Common colds are caused by a virus and thus do not cause the release of inflammation chemical mediators. |
False
The inflammation caused by the virus leads to a runny nose (via vasodilation, increased permeability and increased mucus activity) and nasal obstruction (inflammed mucus membranes) |
|
|
The topical/local nasal decongestants propylhexedrine and levmetamfetamine need to be reapplied how often? |
Every 2 hours (short-acting) |
|
|
The topical/local nasal decongestant xylometazoline needs to be reapplied how often?
How often for oxymetazoline? |
Xylometazoline - every 8-10 hours (intermediate acting)
Oxymetazoline - every 12 hours (long acting) |
|
|
Topical nasal decongestants shouldn't be used for children under what age? |
6 years old
Phenylephrine however can be used in children as young as 4 years old |
|
|
What is pseudoephedrine's dosing and max daily dose for:
12+ years old? 6-11 years old? 4-5 years old? |
Below is all IR dosing
12+ years old - 60mg QID and a max daily dose of 240mg
6-11 years old - 30mg q 4-6 hours PRN and 4 doses maximum per day (so 120mg)
4-5 years old - 15mg q 4-6 hours PRN and 4 doses maximum per day (so 60mg) |
|
|
What is pseudoephedrine's max daily dose for 12+ years old? For 6 to 11 years old? 4 to 5 years old? |
12+ - 240mg
6 to 11 - 120mg
4 to 5 - 60mg |
|
|
Which is more effective in nasal decongestion: phenylephrine or pseudoephedrine? |
Pseudoephedrine |
|
|
What is the bioavailability of oral phenylephrine? Of oral pseudoephedrine? |
Phenylephrine - 40%
Pseudoephedrine - 90% |
|
|
What is phenylephrine's dosing and max daily dose for:
12+ years old? 6-11 years old? 4-5 years old? |
12+ - 10mg q 4 hours (OTC dosing) - max dose was not stated, hwoever under supervision or by Rx dosing can be as high as 20mg q 4 hours, making the max dose 120mg per day
6-11 - 5mg q 4 hours PRN and maximum of 6 doses per day (so 30mg)
4-5 - 2.5mg q 4 hours PRN and a maximum of 6 doses per day (so 15mg) |
|
|
Why shouldn't oral nasal decongestants be taken near bedtime?
What age group(s) are most susceptible to the side effects? |
They cause CNS and CV stimulation giving increased BP, restlessness, insomnia, anxiety, etc
Children and the elderly are more susceptible to side effects |
|
|
What drugs may interact with decongestants and cause possible complications? |
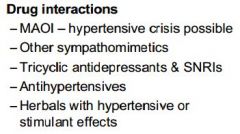
|
|
|
Why are decongestants contraindicated with:
MAOIs? How long should you wait to take a decongestant after stopping MAOIs?
Breastfeeding? |
MAOIs - increased sympathomimetic activity. Wait 14 days.
Breastfeeding - enters breast milk, and decongestants are contraindicated for those younger than 4 years old |
|
|
Can a hypertensive patient take decongestants? |
They can only if his/her HTN is under control and the doctor is aware |
|
|
Why are decongestants to be used very carefully in diabetic patients? |
For severe diabetes, blood flow to the extremities is cut. Decongestants cause vasoconstriction and may worsen this. They rarely also affect glucose levels. |
|
|
Why are decongestants to be used carefully (if not even contraindicated) in patients with BPH? |
BPH patients have trouble urinating, and decongestants will not help this. |
|
|
For topical/local nasal decongestants, about how soon should you start to notice the effects after applying? |
About 5 minutes |
|
|
How can you differ a diagnosis of a sore throat from strep throat? |
Swollen lymph nodes point towards a diagnosis of strep throat |
|
|
How many days maximum can you use a topical/local anesthetic for a sore throat? |
2 days |
|
|
Echinacea is a herbal supplement that MAY help reduce cold symptoms. It has unique properties than diminish its usefulness. What CYP does it induce/inhibit in the liver? In the intestines? |
Induces hepatic 3A4 Inhibits intestinal 3A4 Moderately inhibits 1A2 (not specified whether hepatic or intestinal; I'm assuming hepatic) |
|
|
Why can't Echinacea be taken with immunosuppressants? |
They have opposite MOAs
Echinacea supposedly increases the immune response |
|
|
Which of the following can Echinacea be safely used in: Breastfeeding mothers Pregnant women Children |
None. It's suggested not to use in these groups as there is little to no data on herbal supplements in these populations |
|
|
How effective is vitamin C in fighting common colds? |
Studies are inconclusive. Super doses (above 1g daily) started at the onset of symptoms MAY decrease cold duration by 1 day and severeity by 20% |
|
|
What are vitamin C's dose-dependent side effects? |

|
|
|
How does zinc supposedly fight the common cold? |
By blocking the rhinovirus from attaching to nasal epithelium |
|
|
What are some unique adverse reactions that zinc may cause when used to treat colds? |
Metallic taste Loss of sense of smell Copper deficiency and anemia (at high doses)
Avoid citrus juices within 1 hour of a zinc lozenge (as it may cause zinc chelation) |
|
|
Define the following in terms of duration of time: Acute cough Subacute cough Chronic cough |
Acute - 3 weeks or less Subacute - 3-8 weeks Chronic - 8+ weeks |
|
|
Why can an ACEi cause chronic coughing? |
Inhibiting ACE also affects bradykinin. The coughing can last up to 4 weeks after discontinuing the drug |
|
|
An ACEi drug would produce what "type" of cough? |
Non-productive cough (dry/hacking) |
|
|
Assuming they are effective, what type of cough(s) should antitussives be used for? Expectorants? |
Antitussives - non-productive cough Expectorants - productive cough |
|
|
What is a common mucokinetic agent used OTC? What does mucokinetic mean? |
Guaifenesin
Mucokinetic agents loosen sputum and thin bronchial secretions |
|
|
What are some significant drug-drug interactions with guaifenesin? |
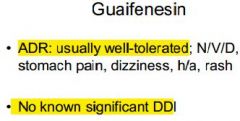
|
|
|
What is the minimum age for guaifenesin? What is its dosing? Its maximum daily amount? |
Must be at least 12 years old Dosing- 200-400mg q 4 hours Max daily dose - 2400mg
They do have pediatric versions for kids as young as 4 with different dosing, but if it barely works at the adult dosage it won't do anything at a lower dose |
|
|
T/F: Camphor, menthol and benzonatate all are peripherally-acting antitussives |
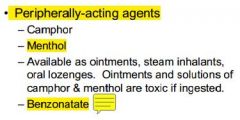
True |
|
|
Dextromethorphan is the D-isomer analogue of what opioid? |
Codeine |
|
|
Dextromethorphan is metabolized by what CYP enzyme? |
2D6 |
|
|
The use of dextromethorphan with an MAOI can cause what potential life-threatening condition? |
Serotonin syndrome
Don't take DXM with MAOIs, 2D6 inhibitors or SSRIs |
|
|
What is the maximum adult daily dosage for dextromethorphan? |
120mg |
|
|
What drug is considered the "gold standard" antitussive for non-productive cough? (According to Dr. Dang) |
Codeine |
|
|
Codeine is converted into morphine by what CYP enzyme? |
2D6 |
|
|
T/F: Genetic polymorphisms affect both the antitussive and analgesic properties of codeine. |
False.
Codeine itself is a good antitussive, but needs conversion via CYP2D6 into morphine for noticeable analgesic effects |
|
|
T/F: Diphenhydramine and brompheniramine (1st gen. antihistamines) have antitussive effects at lower doses than antihistamine effects |
True |
|
|
Benzonatate works by what MOA? |
It produces an anesthetic effect on stretch receptors in the lungs |
|
|
T/F: Patients with acute coughs from the common cold can be treated with both a first generation antihistamine and a decongestant |
True |

