![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
18 Cards in this Set
- Front
- Back
|
How long does it take to create a mature sperm?
When does sperm production begin and end? |
∼64 days
|
|
|
What are the 2 compartments of testes parenchyme? |
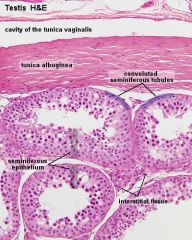
Tubules and interstitium |
|
|
What are the 2 cell types found in the tubules? |
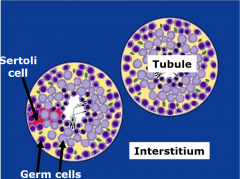
Germ cells Sertoli cells (somatic; provide physical and nutritional support for the GCs) |
|
|
What cell type is found in the interstitium? |
Leydig cells (makes testosterone) |
|
|
Give an overview process of spermatogenesis. |
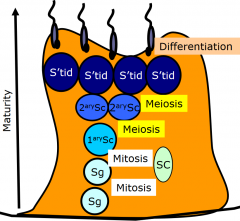
4 cell types: > spermatogonia > spermatocyte > spermatid > spermatozoa 3 processes: > mitosis > meiosis (I&II) > spermiogenesis (differentiation) |
|
|
Describe where each of the cells involved in spermatogenesis/spermiogenesis are found in the tubulues. |
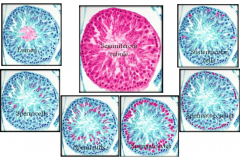
sustenacular = sertoli |
|
|
Describe the development of spermatogonia in the basal compartment of the tubules. |
2 forms of spermatogonia - type A & B
2 forms of type A spermatogonia - pale A & dark A
Dark A divide → 1x dark A + 1x pale A (like asymmetric division in stem cells) Pale A →type B → primary spermatocyte |
|
|
Spermatogonia development diagram. |
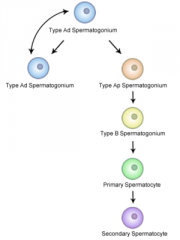
|
|
|
Describe the development of the spermatocytes and spermatids. |
1⁰ Sc→ Meiosis I → 2⁰ Sc
2⁰ Sc→ Meiosis II → S'tid
S'tid → Spermiogenesis → S'zoa |
|
|
Describe the process of spermiogenesis. |
Differentiation of spermatids - round to elongate > No more cell divisions > Tail - propulsion > Midpiece forms – contains lots of mitochondria > Acrosome forms - tip of the head, enzymes for penetration of ovum > Cytoplasmic remodelling - excess removed and left as residual body (phagocytosed by sertoli cells) > Nucleus compacts |
|
|
Spermiogenesis diagram. |
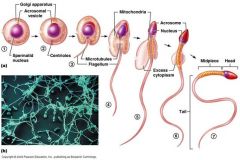
|
|
|
Spermatozoa diagram. |

|
|
|
What regulates spermatogenesis? |
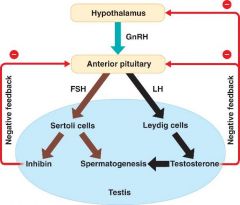
Sertoli cells also produce androgen binding globulin (binds to testosterone & keeps it within the seminiferous tubules) and AMH |
|
|
What is an endocrine disruptor? |
An exogenous substance that disrupts normal endocrine function |
|
|
Describe the different sources of endocrine disruptors. |
Natural hormones
Natural chemicals e.g. phytooestrogens Synthetic pharmaceuticals e.g. hormonal contraceptives Synthetic chemicals e.g. DDT, PCBs |
|
|
Give an example of a synthetic chemical that is an endocrine disruptor. |
Phthalates e.g. DBP - used in the production of PVC
May pose a risk for normal male fetal development: > ↓↓↓ in testosterone & Insl3 production by Leydig cells > Abnormal testis development > ↓ germ cell numbers & delayed differentiation leading to cryptorchidism, hypospadias, infertility, germ cell cancer |
|
|
What is the testicular dysgenesis syndrome (TDS) hypothesis? |
TDS - 4 conditions cryptorchidism, hypospadias, impaired spermatogenesis and testis cancer may all be manifestations of disturbed prenatal testicular development All disorders are risk factors for each other |
|
|
Describe how anabolic steroids can be an endocrine disruptor? |
Synthetic androgens → ↑ -ve fb of HPG axis → hypogonadotrophic hypogonadism → testis atrophy and impaired spermatogenesis → infertility |

