![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
92 Cards in this Set
- Front
- Back
|
General Rule:
It is easier to rule out _______, so do this first unless your history or clinical suspicion dictates otherwise! |
pre- or post- renal failure
|
|
|
These are epithelial cells on the basement membrane
|
Podocytes
|
|
|
These cells support the capillary wall
|
Mesangial Cells
|
|
|
Typically Non-inflammatory
Damage to basement membrane/epithelium=↑permeability -↑ permeability= protein leakage >3.5g/day in urine |
Nephrotic Syndrome
|
|
|
-↓ albumin
-↓ oncotic pressure --> 3rd spacing -↓ effective circulating volume = activation of RAA -loss of Antithrombin III -->hypercoaguable -->clots/emboli -liver stimulated to make cholesterol |
Nephrotic Syndrome
|
|
|
Characterized by:
proteinuria, edema, hyperlipidemia, hypercoaguability |
Nephrotic Syndrome
|
|
|
Typically Inflammatory Process
Immune-mediated Damage Infiltrates of neutrophils and phagocytes and/or proliferation of mesangium |
Nephritic Syndrome
|
|
|
Infiltrates of neutrophils and phagocytes and/or proliferation of mesangium cause:
– Crescentic lesions – Plugging up of Bowman‟s space – Necrosis/Thinning of Glomerular Basement Membrane – Rupture of GBM |
Nephritic Syndrome
|
|
|
CLINICAL = hematuria, oliguria, HTN
LABS: urinalysis usually with (+) blood, RBC casts, and/or protein <3.5 g/day |
Nephritic Syndrome
|
|
|
Proteinuria: >3.5 g/day
This is usually indicative of |
Nephrotic Syndrome
|
|
|
Proteinuria: <3.5 g/day
This can be associated with _______ |
Nephritic Syndrome
|
|
|
You're looking at a urinalysis report and see: (+) blood, RBC casts,
and/or protein <3.5 g/day |
Nephritic Syndrome
|
|
|
What are some typical symptoms of Glomerular Dz?
|
Edema*
weight gain malaise oliguria* hematuria* worsening HTN* |
|
|
A Family Hx of kidney disease, DM, autoimmune diseases might make you think a patient's symptoms are due to _________
|
Glomerular Dz
|
|
|
Physical Exam Findings for Glomerular Dz?
|
– Signs of fluid overload
(edema, JVD, crackles) – Hypertension – Conjunctival pallor (anemia) – Signs of Autoimmune Diseases –Xanthomas |
|
|
What are some physical exam findings
suggestive of autoimmune diseases? |
**SLE**- malar rash, alopecia, apthous ulcers, peripheral edema, pallor
**RA**- nodules, joint effusions, ulnar deviation of fingers |
|
|
What tests are used to help rule out
pre- and post-renal ARF? |
PRE- FeNa, sp gravity, Una, Uosm
POST- bladder scan, Foley, renal US |
|
|
Characterized by:
• Proteinuria > 3.5 g/day (>50mg/kg/day for kids) -Cholesterol in 300-400 mg/dL range • Serum Albumin < 3.5 g/dL |
Nephrotic Syndrome
**Low Sr Albumin b/c we're losing protein in urine** |
|
|
If you see fatty casts (oval fat bodies) in urinalysis what are you thinking?
|
Nephrotic Syndrome
**high cholesterol in plasma** |
|
|
Can see:
↓calcium due to ↓albumin, but also due to loss of proteins which bind vitamin D • Anemia due to loss of transferrin and erythropoietin • Hypercoaguability due to loss of Antithrombin III (AT III) |
Nephrotic Syndrome
|
|
|
BUZZWORDS FOR BOARDS:
Proteinuria Hypoalbuminemia Edema Hyperlipidemia |
Nephrotic Syndrome
|
|
|
Treatment usually always includes:
Statins, ACEI/ARBs, fluid and salt restriction |
Nephrotic Syndrome
|
|
|
T/F
Nephrotic Syndrome is associated with 24-hr urine protein >3.5 g/day |
True
|
|
|
Damage due to effacement/flattening of
podocytes |
Minimal Change Disease
|
|
|
Minimal Change Disease is a subtype of __________
|
Nephrotic Syndrome
|
|
|
Minimal Change Disease can be associated with what 2 things?
|
Can be associated with:
– Medications (lithium, NSAIDs) – *Lymphomas* |
|
|
Most common type of nephrotic
syndrome in kids, accounting for 90% of nephrotic cases < 10 years old |
Minimal Change Dz
|
|
|
Why do you get nephrotic range
proteinuria with minimal change disease? **EXAM** |
Effacement of podocytes
↓ Disruption of filtration slits ↓ proteins leak through "big holes" |
|
|
Si/Sx: edema, massive proteinuria (Pr/Cr up to 9)
Dx: kidney biopsy shows effacement of podocytes |
Mimimal Change Dz
|
|
|
Rx for Minimal Change Dz?
|
Steroids for 8 weeks
|
|
|
A previously healthy 32 year old female presents to your office after having swollen legs for the last 3 weeks.
She denies any recent illnesses, history of HIV or Hepatitis B or C, and does not endorse any symptoms of autoimmune diseases. LABS: Urinalysis: 3+ protein, no WBCs, RBCs or casts Serum Albumin: 3.0 g/dL (normal 4.0 g/dL) Serum Creatinine: 1.0 mg/dL (normal) You decide to get a kidney biopsy. What would you expect to see? A.Linear IgG deposition B. Positive immunofloresence for GBM antibodies C. Effacement of podocytes D. No pathologic changes |
C. Effacement of Podocytes
**Minimal Change Dz** |
|
|
#1 cause of nephrotic syndrome in
African Americans |
Focal Segmental Glomerulosclerosis
(FSGS) |
|
|
HTN at level of glomerulus causes
hyperfiltration, which leads to accumulation of extracellular matrix and eventual scarring and tamponade of glomerulus. EPITHELIAL cells are damaged. |
Focal Segmental Glomerulosclerosis
(FSGS) **Epithelial Cell (podocyte) damage d/t HTN** |
|
|
What cells are damaged in FSGS?
|
Epithelial Cells are damaged due to HTN
(podocytes) |
|
|
Associated with:
- HIV** -Ureteral reflux (kids with posterior bladder valves -Massive obesity -Obstructive Sleep Apnea -Chronic pyelonephritis -Interstitial kidney disease -IV Heroin** |
Focal Segmental Glomerulosclerosis
(FSGS) |
|
|
CLINICAL:
-indolent course; usually asymptomatic in early disease -microscopic hematuria initially |
Focal Segmental Glomerulosclerosis
(FSGS) |
|
|
Prognosis: *50% progress to ESRD in 5 years*
|
Focal Segmental Glomerulosclerosis
(FSGS) |
|
|
This is the exception to the rule that NEPHROTIC syndromes are not due to antibody problems, but is in keeping with the fact that NEPHROTIC is usually NONINFLAMMATORY
|
Membranous Glomerulonephropathy
**Results from antibody/IC deposition** |
|
|
-Damage to mesangial matrix
• Although there are immune complexes associated with this disease, they can't cross basement membrane and, therefore, DO NOT cause inflammatory changes |
Membranous Glomerulonephropathy
|
|
|
Associated with:
– ***Hepatitis B/C *** – Syphilis – Diabetes Mellitus – **SLE, RA ** – ***Malignancies*** • Breast, colon, stomach, kidney, lung |
Membranous Glomerulonephropathy
|
|
|
Workup:
-exclude SLE, RA -Hepatitis serologies ***age appropriate cancer screenings*** Rx: steroids and cytotoxic agents |
Membranous Glomerulonephropathy
|
|
|
A 45 year old male presents to the ED
because he has noted foamy urine for the last several months. He also has gained about 20 pounds in the last 3 months, which he says “must be water weight” because he has noted that his shoes are too tight from being swollen. Pertinent past medical history is significant for only osteoarthritis of his lower back. Family history is significant for coronary artery disease, diabetes, and colon cancer in his father and paternal uncle at ages 50 and 48, respectively. Patient is a nonsmoker, and results of a recent HIV test were negative. LABS -Serum creatinine: 1.2 mg/dL -Serum Albumin: 3.2 g/dL -Urinalysis: 3+ protein; oval bodies, no RBCs -Serum Cholesterol: 355 mg/dL -Random Glucose: 126 Before proceeding to a kidney biopsy,what other tests would you like to order? |
**Membranous Glomerulonephropathy**
ANA --> SLE, RA Hepatitis B and C **colonoscopy** RPR --> Syphilis |
|
|
Increased Prevalence in smokers, nonwhites, those with poor glycemic and/or BP control
|
Diabetic Glomerulosclerosis
|
|
|
Dx:
-urine microalbumin test: microalb/cr >30 -nodular sclerosis on biopsy (Kimmelstiel-Wilson nodules) |
Diabetic Glomerulosclerosis
|
|
|
You are looking at a kidney biopsy and see nodular sclerosis.
(Kimmelstiel-Wilson nodules) |
Diabetic Glomerulosclerosis
|
|
|
A urine microalbumin test reveals:
microalbumin/Cr > 30 |
Diabetic Glomerulosclerosis
**microalbuminuria** |
|
|
Rx for Diabetic Glomerulosclerosis?
|
-Glycemic Control
-***ACEi/ARBs*** (even if there's no HTN) -Intensive Cholesterol Control (LDL<100) |
|
|
BUZZWORDS:
CLINICAL: Hematuria Oliguria HTN LAB: Urinalysis: (+) blood, RBC casts Urine protein < 3.5 g/day |
Nephritic Syndrome
|
|
|
T/F
Protein on UA rules out nephritic glomerular diseases. |
False
|
|
|
Which Immunoglobulin plays a critical role in mucosal immunity? (i.e. More is produced in mucosal linings than all other type of antibody combined)
|
IgA
|
|
|
#1 cause of glomerulonephropathy
worldwide • 2-3 days post infection (URI, GI) • IgA Deposition associated with –Henoch-Schönlein Purpura |
IgA Nephropathy
|
|
|
Upper respiratory tract or GI infection
↓ Defective mucosal immunity ↓ Overproduction and hence increased serum levels of partially degalactosylated polymeric IgA1 and IgA-immune complexes (Pathogenic IgA) |
IgA Nephropathy
|
|
|
IgA Symptoms due to inflammation:
-Focal, mesangial proliferative glomerular inflammation |
Asymptomatic, MICROSCOPIC hematuria
|
|
|
IgA Symptoms due to inflammation:
-Diffuse, mesangial proliferative glomerular inflammation |
More acute nephritis with MACROSCOPIC hematuria
|
|
|
What type of hematuria is associated with IgA nephropathy in patients with a recent GI or UR infection?
|
Macroscopic hematuria (bloody urine)
|
|
|
Dx:
history, microscopic/macroscopic hematuria, normal C3, normal C4 Dx: ACEi/ARB2, steroids if pr/cr ratio >1 |
IgA Nephropathy
|
|
|
What are the levels of C3 and C4 like in IgA nephropathy?
|
Normal
|
|
|
Disease of Children
• Usually follows URI • Abnormal IgA deposition in: – Skin – GI tract – Kidney – Joints |
Henoch-Schönlein Purpura
|
|
|
CLINICAL FINDINGS:
• Lower extremity bruising (“palpable purpura”) • Bloody diarrhea • Hematuria and Hypertension • Arthralgias (bleeding into joints) Rx: Supportive |
Henoch-Schönlein Purpura
|
|
|
You see a patient with:
Subendothelial antigen deposition • 2-3 weeks post infection (strep pharyngitis or cellulitis) • Low C3, Low C4 |
Post-Infectious GN
|
|
|
T/F
Prompt treatment of strep infection does not guarantee that post-infectious GN will not develop |
True
|
|
|
A 32 year old female with no PMH
presents to your office due to general malaise, runny nose and sore throat. She is also concerned because her urine has been dark. Her symptoms have been going on for about 3 days. She has a slightly elevated BP at 146/88. The result of her rapid strep test is positive, urine pregancy test is negative, and moderate blood is noted on urine dipstick. Based on what you know, what is the most likely diagnosis? A. IgA Nephropathy B. Post-Infectious GN |
IgA Nephropathy
|
|
|
T/F
Prompt treatment of strep infection does not guarantee that post-infectious GN will not develop |
True
|
|
|
A 32 year old female with no PMH
presents to your office due to general malaise, runny nose and sore throat. She is also concerned because her urine has been dark. Her symptoms have been going on for about 3 days. She has a slightly elevated BP at 146/88. The result of her rapid strep test is positive, urine pregancy test is negative, and moderate blood is noted on urine dipstick. Based on what you know, what is the most likely diagnosis? A. IgA Nephropathy B. Post-Infectious GN |
IgA Nephropathy
**Timeframe is 2-3 days here.. Not 2-3 weeks which would make you think Post-Infectious GN** |
|
|
What pattern of complement would you expect for IgA nephropathy?
A. Low C3, low C4 B. Low C3, normal C4 C. Normal C3, normal C4 D. Normal C3, low C4 |
Normal C3, Normal C4
|
|
|
Usually secondary to other diseases
• Associated with: – Sjogren‟s Syndrome – Systemic Lupus Erythematosis – Hep B/C with cryoglobulinemia – Infective endocarditis |
Membranoproliferative GN
|
|
|
What are the two characteristic complaints in Sjogren's Disease?
What antibodies are positive in Sjogren's Disease? |
Dry Mouth, Dry Eyes
Positive Anti-Ro, Anti-La (Membranoproliferative GN) |
|
|
LABS: UA with dysmorphic RBCs,
erythrocyte casts, LOW C3, NORMAL C4 • Rx: treat underlying cause, steroids, antiplatelets |
Membranoproliferative GN
|
|
|
C3 and C4 levels in Membranoproliferative GN?
|
C3=LOW
C4=NORMAL |
|
|
• 10-20% of cases of Rapidly
Progressive GN • Can be ANCA + • Antibodies to type IV collagen |
Anti-GBM/Goodpasture's Syndrome
|
|
|
CLINICAL
• Rapid Onset of HTN, oliguria • Fatal if not treated promptly Kidney only: more common in older women (anti-GBM syndrome) – Kidney/Lung: more common in young men (Goodpasture‟s syndrome); 70% will have alveolar hemorrhage |
Anti-GBM/Goodpasture's Syndrome
|
|
|
Can have isolated kidney involvement or kidney and lung involvement
|
Anti-GBM/Goodpasture's Syndrome
– Kidney only: more common in older women (anti-GBM syndrome) – Kidney/Lung: more common in young men (Goodpasture‟s syndrome); 70% will have alveolar hemorrhage |
|
|
Dx: anti-GBM antibodies, biopsy
• Rx: cyclophosphamide + steroids; plasmapheresis if pulmonary hemorrhage |
Anti-GBM/Goodpasture's Syndrome
|
|
|
Tx for Goodpasture's patient with pulmonary hemorrhage?
|
PLASMAPHERESIS
|
|
|
• Prognosis depends on:
–promptness of diagnosis and treatment –Degree of kidney involvement (if Cr > 5 or dialysis required, prognosis poor) |
Anti-GBM/Goodpasture's
|
|
|
2 Types of Small Vessel Vasculitis?
|
1. Wegener's Granulomatosis
-lung, kidney and sinus involvement 2. Microscopic Polyangiitis |
|
|
Patient has a Small vessel vasculitis with:
-lung, kidney and sinus involvement |
Wegener's Granulomatosis
|
|
|
CLINICAL: (non-specific)
-decreased appetite -weight loss -hematuria and/or proteinuria -polymyalgia |
Small Vessel Vasculitis
|
|
|
c-ANCA +
anti-PR3– Wegener's anti-MPO– Microscopic Polyangiitis |
Small Vessel Vasculitis
|
|
|
anti-PR3– ?
|
Wegener's
|
|
|
anti-MPO– ?
|
Microscopic Polyangiitis
|
|
|
A 50 year old female presents to the office with a chief complaint of coughing up blood. She has no significant past medical history and has not had any recent respiratory illnesses. A PPD placed 6 months ago was negative. She is a lifelong nonsmoker. Routine labs reveal an increase in serum creatinine from 0.8 to 3.2 mg/dL in 3 months.
Vital Signs are unremarkable except for a BP of 150/80. You are concerned that the hemoptysis may be part of a pulmonary-renal syndrome like Goodpasture‟s or Wegener‟s. What one question about associatedsymptoms could help you differentiate between Goodpasture‟s Syndrome and Wegener‟s Granulomatosis? |
History of recurrent sinusitis = Wegener's
***** |
|
|
What labs could you order to help you differentiate between Goodpasture's Syndrome and Wegener's Granulomatosis?
|
c-ANCA (positive in Wegener's)
anti-PR3 (Wegener's) anti-GBM (Goodpastures) |
|
|
What is the treatment for pulmonary
hemorrhage in either Wegener's or Goodpasture's? |
Plasmapheresis
|
|
|
CLINICAL:
acute onset of hematuria, proteinuria and edema; can also see pancytopenia • Diagnosis: anti-Sm, anti-DS DNA** |
Lupus Nephritis
|
|
|
– III focal nephritis
– IV diffuse nephritis – V membrane formation, nephrotic range proteinuria – VI >90% of glomeruli sclerotic, chronic |
Lupus Nephritis
|
|
|
This disease is *associated with both membranous and membranoproliferative GNs*
|
Lupus Nephritis
Nephrotic/Nephritic Syndrome |
|
|
Rx: Class III and above: cyclophosphamide +/- steroids
• Px: Depends on – Kidney function on presentation – Histologic type – Crescents (aggressive disease) |
Lupus Nephritis
|
|
|
Know this summary slide
|
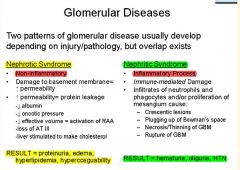
|
|
|
Know this algorithim
|
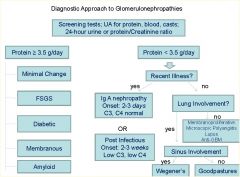
|
|
|
Nephritic or Nephrotic Diseases? :
-IgA Nephropathy • Henoch Schönlein Purpura • Post-Infectious Glomerulonephritis • Membranoproliferative GN • Anti-GBM/Goodpasture‟s Syndrome • Small Vessel Vasculitis • Lupus Nephritis |
Nephritic
|
|
|
Nephritic or Nephrotic Diseases? :
-Minimal Change Disease • Focal Segmental Glomerulosclerosis • Membranous Glomerulonephropathy • Diabetic Glomerulosclerosis (aka Diabetic Nephropathy) • Amyloid |
Nephrotic
|

