![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
27 Cards in this Set
- Front
- Back
|
What is the osmotic pressure produced by dissolved proteins called?
|
The osmotic pressure produced by dissolved proteins is called “colloid osmotic pressure” or “oncotic pressure”.
|
|
|
What happens when smooth muscle is stretched?
|
When stretched, smooth muscles will reflexly contract. Therefore, a sudden local increase in blood pressure entering the metarteriole will tend to cause the metarteriole to constrict and maintain a constant blood flow into the capillary bed.
|
|
|
What does sympathetic innervation do to metarterioles?
|
causes them to constrict resulting in widespread vasoconstriction and an increase in systemic blood pressure
|
|
|
What locally released compounds can inhibit metarteriolar contraction and the resulting vasodilation will increase local blood flow (sometimes producing hyperemia and flushing of the area).
|
Bradykinin or Histamine
|
|
|
T/F
A potent vasoconstrictor is tissue oxygen? |
True
While this might seem contrary, look at the reverse situation: If tissue oxygen levels fall, such as happens when the local cells become metabolically active (i.e. contracting muscle), then the constriction is lost and there is a marked vasodilation. This vasodilation results in locally increased blood flow to capillaries perfusing active cells. |
|
|
If endothelial cells of the capillary represent little or no barrier to diffusion of gases like oxygen or carbon dioxide, what are the presence of pores necessary for?
|
Effective movement of small non-lipid soluble molecules like ions, glucose and amino acids. The pores are NOT LARGE ENOUGH to allow movement of plasma proteins out of the plasma and into the interstitium. **in the healthly state**
|
|
|
What is water accumulation in body tissues known as?
|
Edema
|
|
|
What is CHP (capillary hydrostatic pressure at the beginning of a capillary?
|
30 mmHg
|
|
|
What is CHP (capillary hydrostatic pressure at the end of a capillary?
|
10 mmHg
|
|
|
What is the THP (tissue hydrostatic pressure)?
|
-3
due to the presence of lymphatics sucking water from the interstitium |
|
|
What is the net hydrostatic force at the arterial end of a capillary?
|
33 mmHg
(30-(-3)=33mmHg) |
|
|
What is the net hydrostatic force at the venous end of a capillary?
|
13 mmHg
(10-(-3)=13mmHg) |
|
|
What is the total amount of stuff dissolved in water referred to as (for blood)?
|
Osmolarity
Osmotic Pressure Sucks |
|
What is the COP inside the capillary?
|
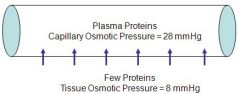
COP = 28 mmHg
(doesn't change from one end to the other) Net total COP-TOP= 20 mmHg |
|
What is the TOP (tissue osmotic pressure) outside a capillary?
|
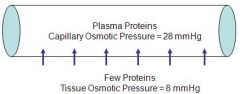
TOP = 8 mmHg
because interstitium also has some dissolved proteins, just not as much. Net difference is COP-TOP=20mmHG sucking back into the capillary |
|
|
What situations will promote edema?
|
1. Anything that increases net loss of fluid from a capillary
a. Increased CHP b. Decreased COP c. Increased TOP d. Decreased THP 2. Something blocking the lymphatic drainage from the area (parasites invading the lymph nodes in elephantiasis or radical masectomy) |
|
|
Sometimes we want to produce edema, such as Bowman's capsule during urine formation.
How do we regulate this process? |
By regulating the CHP
This is done through the presence of a secondary metarteriole associated with each capillary bed. |
|
|
How do we get increased CHP and filtration pressure in a glomerulus?
|
Constriction of the Efferent arteriole
Dilation of the Afferent arteriole |
|
|
What is the renal blood flow for an average male?
|
1.2 L/min (25% of the total cardiac output)
|
|
|
What is the rate of plasma flow through the kidneys?
|
650 mL/min (based on a hematocrit of 40%)
|
|
|
What is the Glomerular Filtration Rate GFR?
|
An average of 20% of the renal plasma flow (RPF) is filtered at the glomerulus
|
|
|
What is the flow rate of plasma entering Bowman's Capsule and proceeding into the proximal convoluted tubule?
|
125 mL/min
|
|
|
What is the flow rate of fluid entering the collecting duct and leaving the body as urine?
|
2-3 mL/min
|
|
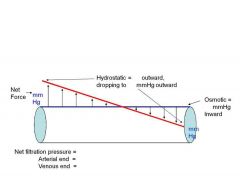
What is the formula for NFP (Net Filtration Pressure)?
|
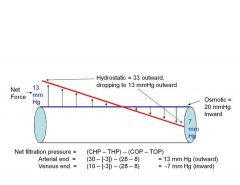
NFP=(CHP-THP)-(COP-TOP)
|
|
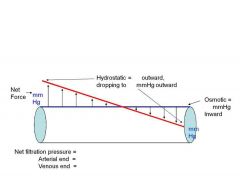
What is the NFP at the arterial and venous ends of the capillary?
|
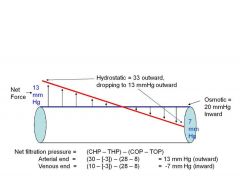
Arterial = 13 mmHg outward
Venous = -7 mmHg inward |
|
|
How much fluid is collected by the lymphatics per day?
|
2-3 liters per day
|
|
|
At what pressure is there no net movement of fluids in or out of the capillary?
|
20 mmHg
|

