![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
135 Cards in this Set
- Front
- Back
|
What are the functions of the kidney? |
-regulate water, electrolytes, blood pressure and acid-base balance -metabolism of endogenous and exogenous compounds -excretion of chemicals, waster products -endocrine functions |
|
|
Define xenobiotic |
a foreign chemical substance that is NOT normally/naturally produced or expected to be present within an organism |
|
|
Define nephrology |
the study of normal kidney function, kidney problems, the treatment of kidney problems, and renal replacement therapy |
|
|
Define Urology |
focuses on the surgical and medical diseases of the male and female urinary tract system and the male repro. |
|
|
What are the 3 main sections of a kidney? |
The cortex, inner medulla, and outer medulla |
|
|
What is the functional unit of the kidney? |
the nephron |
|
|
What makes up the nephron? |
vessels into the glomerulus, the glomerulus, PCT, DCT, loop of Henle, and the collecting tubules |
|
|
What is the relationship between animal size and the number of nephrons? |
As the animal gets bigger, they have more nephrons. ex: cow has 4 million, cat has 200,000 |
|
|
What makes up the proximal tubule? |
the proximal convoluted tubule and the Pars Recta |
|
|
What part of the nephron has a brush border? |
the proximal tubule |
|
|
What part of the nephron has a lot of metabolic activity and why? |
the proximal tubule to help transport substances across the cell membrane from the lumen of the tubule. |
|
|
What are the segments to the loop of Henle? |
thin descending, thin ascending, thick ascending (in this order) |
|
|
What are the segments of the distal convoluted tubule? |
early and late segments |
|
|
What are the segments of the collecting tubules? |
cortical, outer medullary, and inner medullary |
|
|
Formula for Urinary Excretion |
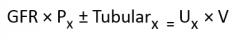
Urinary Excretion= Filtered load + tubular processing |
|
|
What is the renal clearance formula? |
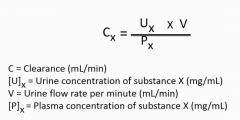
|
|
|
What is the "gold standard" substance used to measure for glomerular filtration rate (GFR)? why? |
Inulin. It is NOT secreted or absorbed just filtered in the kidney. |
|
|
What should the clearance of Albumin be? |
close to zero. Plasma proteins should NOT make it into the urine unless there is a major problem. |
|
|
What is PAH clearance measurements used to determine? |
Renal plasma flow (RPF) because it is filtered and secreted. |
|
|
How can you tell if a substance was secreted or absorbed in the kidney? |
You compare it to the clearance of inulin. (clearance of substance/C of inulin) -If it=1, there is no net secretion or reabsorption -If it is >1, net secretion -<1, net reabsorption |
|
|
Where is most of the blood flow to the kidney going? |
to the cortex (about 93%) -6% to the outer medulla -1% to the inner medulla |
|
|
What type of arteriole delivers blood to the glomerulus? |
the afferent arteriole |
|
|
What type of arteriole takes blood away from the glomerulus? |
the efferent arteriole |
|
|
What happens to blood flow when alpha-1 receptors are stimulated? |
-vasoconstriction by releasing NE -decreases renal blood flow and glomerular flow rate |
|
|
What are more alpha-1 receptors located: efferent or afferent arterioles? |
afferent arterioles |
|
|
What happens at low levels of Angiotensin II? |
glomerular flow rate will increase because you are mostly causing vasoconstriction in the efferent arterioles |
|
|
What happens at high levels of Angiotensin II? |
Glomerular flow rate will decrease because it is then affecting the afferent arterioles as well. |
|
|
What are the effects of Atrial Natriuretic Peptide on the kidney? |
-dilate afferent arterioles -constricts efferent arterioles -Net decrease in vascular resistance -Increases renal blood flow and GFR |
|
|
What vasodilator is produced by the kidney in response to increased Angiotensin II and Catecholamine levels? |
Prostaglandins (E2 and I1) as a protective response |
|
|
What is the effect of prostaglandins on the kidney? |
-vasodilation of efferent and afferent arterioles -increases RBF |
|
|
What drugs inhibit the protective vasodilation activity of Prostaglandins? |
NSAIDS |
|
|
What is autoregulation? |
It means the kidney is able to maintain a stable RBF at a range of different pressures -ANS is NOT involved in this -relies on renal resistance |
|
|
Below what renal artery pressure do we see a decrease in Renal blood flow? |
below 80 mmHg |
|
|
Describe the Myogenic Autoregulation Theory |
As pressure in the kidney goes up, there is a stretch blood vessel detects it and constriction reflex occurs. -Stretch opens up Ca2+ channels that increases smooth muscle contraction leading to more resistance in the blood vessels. |
|
|
Describe the Tubulo-Glomerulo feedback theory of kidney autoregulation |
As GFR increases, so does solute delivery to the Macula densa. This is senses causes vasoconstrictors to be released. -Vasoconstrictors cause constriction of afferent arterioles through autocrine system. -prevents excessive loss of solute |
|
|
What substance is measure to determine renal plasma flow (RPF)? Why? |
Para-Aminohippuric Acid (PAH) because it is filtered and secreted but does NOT alter RPF |
|
|
Describe the main idea behind the Fick principle? |
The amount of PAH going into the renal artery has to equal the amount that is coming out (either through renal vein or urine) |
|
|
Formula for RPF |
RPF= ([urine PAH times V)/[P PAH] |
|
|
How do you convert renal plasma flow to renal blood flow? |
RBF= RPF/(1-hematocrit) |
|
|
What happens to renal blood flow as hematocrit increases? |
It increases as well. |
|
|
What is the first step in producing urine? |
glomerular filtration |
|
|
What is glomerular ultrafiltrate similar to? |
plasma except ultrafiltrate does not have proteins in it |
|
|
What are the layers to the glomerular capillary and what is contained in each? |
1. Endothelium with pores 2. Basement membrane with lamina interna, lamina densa, and lamina externa 3. Epithelium with podocytes, foot processes, and filtration slits |
|
|
What is the main mechanism to keep proteins from being filtered through the glomerulus? |
The glomerulus has a fixed negative charge. this stops larger negative charged things (like proteins) from crossing its membranes |
|
|
Rank negatively charged, positively charge, and neutral things by how easily they are filtered through the glomerular membrane. |
Negatively charged (hardest time), neutral, positively charged (easiest time) |
|
|
What happens to filtration when oncotic pressure increases? |
Filtration goes down.
|
|
|
What happens to oncotic pressure as you get closer to the end of the glomerulus? |
It increases. --Water is leaving the glomerulus but proteins are not so their concentration is going up and up |
|
|
What is the net filtration at the end of the glomerulus? Why? |
It is zero because the oncotic pressure keeps rising. This is causing water to reenter the glomerular capillary instead of being filtered out. |
|
|
Describe the effects of an increase of SNS or high levels of Angiotensin II on the GFR and RPF |
Decrease GFR and RPF. EX: increase in SNS and high levels of AG-II |
|
|
Describe the effects of constricting efferent arterioles on GFR and RPF. |
decrease RPF but increase GFR Ex: low levels of AG-II |
|
|
What are the requirements for a marker that best measures GFR? |
-need something that is filtered but not secreted or absorbed -should not be handled at all by the tubules -little protein binding -does not alter GFR itself -good size/charge to be freely filtered across the glomerulus |
|
|
What is the ideal substance used to measure GFR? |
Inulin |
|
|
Formula for GFR of Inulin |
GFR= ([urine inulin]/[plasma inulin] times urine flow rate |
|
|
Why do we measure GFR? |
it is a measure of the functional renal mass. -Are kidney's healthy or not? -Changes way before blood levels change to indicate a problem |
|
|
Define Filtration fraction |
GFR divided by RPF -used more in research than in clinics |
|
|
What does the filtration fraction show? |
How much blood is taken out in the glomerulus (answer to fraction) -remaining blood is going to the peritubular capillaries |
|
|
What is an easier way to measure GFR than collecting urine? |
Iohexol can be injected and tested in the serum at 1,2 and 3 hours. Iohexol is ONLY filtered by the kidneys so its concentration in serum shows how quickly the kidneys are filtering it out. |
|
|
What happens to serum creatinine levels in the blood as GFR (function nephrons) goes from 100% to 50% |
NOTHING |
|
|
What percentage of the kidney nephrons are still functional when serum Creatinine levels start to change? |
25% After this point, creatinine levels change very quickly |
|
|
Where does s-Creatinine come from? |
the muscles. It is a product of phophocreatine break down -produced at a constant rate |
|
|
How is BUN produced in the body? |
It is the end product of protein and AA break down. -not produced at a constant rate |
|
|
What is s-creatinine a better measure of GFR than BUN? |
BUN is NOT produced at a constant rate. It varies on the diet, when you ate last etc. Creatinine is produced at a constant rate |
|
|
When you get high levels of BUN or s-creatinine in a blood work up, what should you be worried about? |
kidney function or GFR |
|
|
What are some advantages to testing SDMA instead of Creatinine to detect kidney function? |
-It changes earlier (at about 25% kidney loss) -It is only filtered by the kidney like s-creatinine -it does not appear to be affected by animals muscle mass |
|
|
How are s-creatinine levels altered by muscle mass? |
When an animal loses muscle mass, creatinine levels go down. This means s-creatinine could show at a normal level even though the animal has a kidney problem. |
|
|
What is most renal work related to? |
Na+ reabsorption |
|
|
Formula to determine if something is secreted or absorbed |
Filtered load-excretion rate 0= no net tubular effect + = reabsorbed - = secreted |
|
|
What is usually also reabsorbed with sodium in the kidney? |
glucose through secondary active cotransport |
|
|
How is Na+ usually pumped out of the cell into the blood? |
Na+/K+ ATPase |
|
|
What is the renal threshold? |
The blood sugar level when glucose starts showing up in the urine -around 200 mg/dL |
|
|
What is T max? |
the max number of mG of glucose the tubules are capable of reabsorbing -all glucose carriers are saturated |
|
|
What is tubular splay? |
the different between the threshold and the T max -caused by some low affinity transporters that allow glucose to attach/detach, attach/detach |
|
|
What is occurring during hyperglycemia? |
the amount of glucose has exceed the renal threshold and glucose is seen in the urine -Ex of causes: diabetes mellitus and stress |
|
|
What can occur to glucose transport during pregnancy? |
During pregnancy, GFR is increased. This increases the filtered load of glucose. The higher load of glucose exceeds transporter capacity. |
|
|
Where is glucose primarily reaborbed at in the kidneys? |
proximal tubules |
|
|
Describe urea handling in the kidney. |
-filtered and reabsorbed. can be secreted -free flowing -generally follows water reabsorption (same direction) |
|
|
Where are urea concentrations usually the highest in the nephron? Why? |
in the thick ascending limb and distal convoluted tubule because it can not follow water movement in these areas. -water can get out but urea canNOT |
|
|
What parts of the nephron are NOT permeable to urea? |
ascending loop, DCT, Cortical convoluted collecting tubule, outer medullary collecting tubule |
|
|
Define isosmotic reabsorption |
Water went along in the same proportion as the substance so the concentration remains the same |
|
|
What part of the nephron contributes to most of the Na+ reabsorption? |
the proximal convoluted tubule (67%) and the thick ascending limb (25%) |
|
|
How are Na+ and H2O reabsorption linked in the proximal tubule? |
-water follows the movement of Na+ -They are reabsorbed in proportion (isosmotic reabsorption) |
|
|
What is the key transporter that favors the movement of Na+ into the cell across a permeable membrane? |
The Na+/K+ ATPase moves Na+ keeps a low concentration of Na+ in the cell (moves it into the blood) so Na+ wants to cross the permeable membrane from the lumen |
|
|
What cotransporter is predominantly used to reabsorb Na+ in the early proximal tubule? |
with HCO3- |
|
|
By the late proximal tubule, what ion is left to be absorbed? |
Chloride. -Glucose, AAs and HCO3 have all been reabsorbed by now. |
|
|
What cotransporter is used with Na+ reabsorption in the late proximal tubule? |
Chloride |
|
|
What would you expect to happen to tubular reabsorption if GFR goes up? |
It would increase too. |
|
|
What happens to the reabsorption of water and solutes when you give IV fluids? (explain in detail) |
-Reabsorption decreases because the fluids dilute the protein concentration (oncotic pressure) and increase the pressure in the capillaries. Expanding the Extracellular fluid volume These conditions do NOT favor solute/water movement into the capillaries |
|
|
What type of permeability occurs in the thin ascending and thin descending loops of Henle? |
Passive permeability...little to no energy is being used |
|
|
Describe the cellular mechanism for Na+ reabsorption in the thick ascending limb of the loop of Henle. |
-3 ion transport system -1 Na+, 2 Cl-, and 1 K+ must bind for transporter to work. -Cl- and K+ diffuse into blood down concentration gradient -Na+ uses Na+/K+ ATPase to get into blood |
|
|
What hormone enhances the function of the Na+K+Cl- cotransporter in the thick ascending limb? |
ADH (antidiuretic hormone) |
|
|
What part of the loop of Henle is NOT permeable to water? |
the entire ascending limb (thin and thick portions) and the early distal tubule |
|
|
Describe the diluting segment of the nephron |
-from the hair pin turn to the distal convoluted tubule -Na+ is able to enter the cell from the tubule lumen but water canNOT -this causes dilution of the urine because ion concentration decreases |
|
|
Where is the first location for a Na+/Cl- transporter in the nephron? |
the early distal convoluted tubule
|
|
|
What group of drugs can block the Na+/Cl- transporter? |
Thiazide diuretics (used in heart failure patients to get more Na+ out of the body) |
|
|
How does Na+ enter the cell from the lumen in the late distal tubule and collecting ducts? |
Through an electrical channel -NO cotransporters in the principal cells here |
|
|
What happens to K+ in the late distal tubules? |
It is favored to leave the cell and enter the urine. |
|
|
Describe the function of Aldosterone. Where does its action occur? |
It increases the number of Na+ channels in the late distal tubule so that more Na+ can be reabsorbed. This also increases the transport of K+ out of the cell into the urine |
|
|
Describe the function of principal cells in the late distal tubule |
Favor Na+ reabsorption, K+ secretion and are permeable to water if Aldosterone is present |
|
|
What is the function of the alpha-intercalated cells in the late distule tubule? |
K+ reabsorption and H+ secretion |
|
|
What is the effect of ADH on the late distal tubule? |
It changes the permeability of water in this location |
|
|
What drugs can be used to inhibit the effect of Aldosterone in the late distal tubule? |
K+ sparing diuretics (triamterene, amiloride, and spironolactone) -used to increase Na+ secretion |
|
|
What is going to happen in the kidney if the animal increases Na+ intake? |
-increase in ECF and EABV -Decrease in SNS (dilate afferent arterioles to increase GFR) -Increase ANP -Decrease osmotic pressure and aldosterone -NET EFFECT: increase Na+ excretion
|
|
|
What is going to happen in the kidney if the animal decreases its Na+ intake? |
-NET EFFECT: increase Na+ reabsorption -Increase SNS (vasoconstriction) -decrease ANP -increase osmotic pressure and Aldosterone |
|
|
Where is most of the K+ in the body located at? |
inside cells (98%) |
|
|
What can insulin cause in terms of K+? How? |
Hypokalemia (K+ deficiency) by increasing Na+/K+ ATPase. It can cause more K+ to be pushed in to cell |
|
|
What are some things that cause K+ to leave cells? |
-extreme dehydration (K+ flows with H2O out of the cell -exercise -cell lysis -metabolic acidosis: H+ going into the cell pushes K+ out |
|
|
Where is most of K+ reabsorbed at? |
the proximal tubule (67%) and the thick ascending limb (20%) |
|
|
What is unique about K+ secretion? |
It varies greatly. It can be 1% or up to 110% depending on your dietary amounts of K+ and the body's need for it |
|
|
What brings K+ into the cell in the thick ascending limb? |
The 3 ion (Na+/Cl-/K+ cotransporter) transporter |
|
|
What drug can cause hypokalemia by disrupting the 3 ion transporter in the thick ascending limb? |
Furosemide (Lasiks) or diuretics |
|
|
Where does the fine tuning of K+ levels occur in the nephron? |
the late distal tubule and collecting ducts |
|
|
Describe what happens to K+ in alpha-intercalated cells of the late distal tubules? |
K+ and H+ are pumped in from the lumen using ATP (primary active transport) K+ is pumped out of the cell through Na+/K+ ATPase and a K+ ion channel |
|
|
Describe what happens to K+ in the principal cells of the late distal tubules |
Na+ comes in through an electrical channel and K+ is secreted into the lumen through an electrical channel |
|
|
What is the main determining factor on how much K+ is reabsorbed or secreted? |
the concentration of K+ inside the cells (size of the electrochemical gradient) |
|
|
What is aldosterone's effect on Na+ reabsorption? |
It increases K+ secretion by principal cells by causing insertion of K+ channels in the luminal membrane |
|
|
What happens to K+ if the animal has acidosis? |
H+ ions are going to be pushed out of the cells into the urine. This will decrease K+ secretion. |
|
|
What happens to K+ if an animal is alkalotic? |
K+ secretion will be increased. H+ ions will be pushed into the cells which pushes K+ out of the cells |
|
|
Explain how Loop diuretics and thiazides increase K+ secretion. |
They block Na+ reabsorption upstream. This causes more Na+ to be delivered to the principal cells of the distal tubules. These cells will secrete more K+ so they can absorb more Na+. They also increase flow rate which dilutes K+ causing more to be lost |
|
|
What is the group of hormones that help regulate phosphate homeostasis? |
Phosphatonins. Tend to lower Phosphorous in the body |
|
|
Where is most phosphorous reabsorbed at? |
the proximal tubule |
|
|
What is there such a high amount of phosphorous in the urine? |
It acts as a buffer for acid secretion. 15% is excreted |
|
|
What is the only substance that is "fine tuned" in the proximal tubule? |
phosphorous |
|
|
Describe PTH's affect on Phosphorous reabsorption. |
It blocks the Na+ phosphate luminal cotransporter in the PCT by making it internalized ("hiding it"). This causes excess Phosphorous in the urine (a.k.a. phosphaturia) |
|
|
What is the most important phosphatonin? |
Fibroblast Growth Factor 23 (FGF-23) |
|
|
What are the effects of FGF-23? |
It decreases activity of Na+/phosphate cotransporter in the PT and decreases the production of calcitriol. Overall, increases Phosphorous in the urine and decreases phosphorous absorption in the SI |
|
|
What is ultrafilterable calcium? |
It is the calcium that CAN go through the glomerulus. It contains the complexed to anions and ionized forms. (do not include protein-bound calcium) |
|
|
What happens to ionized Ca2+ levels during acidemia? Why? |
Ionized Ca2+ levels increase. This is because more H+ ions bind to albumin and less Ca2+ are able to bind. |
|
|
What is PTH's effect on Ca2+ reabsorption? Where does this happen? |
It increases Ca2+ reabsorption in the late distal tubule |
|
|
Why is Calcium reabsorbed in the mTAL? |
because the lumen becomes charged due to Ma+/Cl-/K+ pump. This drives some positive ions (like Calcium) into paracellularly into the blood |
|
|
What ions are lost due to loop diuretic drugs? |
Na+, K+, Cl- and Calcium |
|
|
What is the only location in the nephron where Calcium absorption is NOT paired with Na+ absorption? |
the distal convoluted tubule |
|
|
Why would you give thiazide diuretics to a patient with chronic urinary calcium stones? |
They increase Ca2+ reabsorption and decrease excretion in the urine. |
|
|
What is the protective protein that transports Ca2+ across the cell? |
Calbindin |
|
|
Where is the major site of Magnesium reabsorption in the nephron? |
the medullary thick ascending limb |
|
|
What drives Magnesium reabsorption in the mTAL? |
a positive charge in the lumen from the 3 ion cotransporter drives Magnesium paracellularly |

