![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back
|
What is the leading cause of renal failure in children |
CAKUT --> congenital abnormalities of kidney and UT |
|
|
what is renal agenesis |
Where nephrons fail to develop or the uteric bud metanephros interaction fails to occur. if single kidney, other hypertrophies to compensate, if bilateral = death |
|
|
what is polycystic kidney disease |
large bubbly appearance of kidney, due to it being filled with multiple fluid filled cysts that grow and compress the renal parenchyma --> kidney grows as the cysts grow renal failure in childhood if recessive, in adult hood if dominant |
|
|
what are horse shoe kidneys |
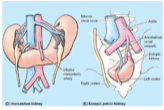
inferior poles of kidneys fuse and form a horseshoe, cannot ascend due to root of IMA and cannot rotate generally not too bad, but can rupture in trauma |
|
|
what causes duplex kidney/bifid renal pelvis and ureters and what is its significance |
premature division of ureteric bud. extent of division depends on the completeness of embryonic division. incomplete division = bifid renal pelvises and ureters. complete division = supernumerary kidney causes twists and kinks |
|
|
what is: retrocaval ureter posterior urethral valve hydroureter hydronephrosis |
ureter passes behind IVC valve in neck of bladder = common bladder outlet obstruction in males dilated ureter dilation of renal pelvis due to urine reflux because of obstruction, loss of peristalsis |
|
|
what is: ureteropelvic junction obstruction vesicoureteric junction obstruction |
obstruction where ureter meets pelvis --> nephron destruction due to bak pressure back flow or urine into the kidney (possibly) due to blockage where the ureter enters the bladder |
|
|
why are UTIs more common in women |
shorter anatomy, proximity to anus, easy to transfer bacteria to urethra in sexual intercourse (direct correlation with increased intercourse) |
|
|
What are the most common pathogenic causes of community acquired and nosocomial acquired UTIs |
community: 80-85% E. coli (from anus) and 5-10% staph saprophyticus nosocomial: 40% E. coli and other 60% = klebsiella, staph, pseudomonas |
|
|
What are the risk factors for UTIs |
Female, prostatic hyperplasia (urinary stasis), abnormal UT (obstruction, reflux, neurogenic i.e. doesnt empty), pregnancy (dilated ureters) |
|
|
How does a UTI occur |
bacteria --> urethra (commonly from anus) --> ascends --> forms biofilm on bladder (resists immune system) --> |
|
|
What do the bacteria (mainly E. Coli posses) |
Fimbriae (adhesion), capsule (down phagocytosis), haemolysins (renal cell damage), urease (in proteus bacterium --> catalyses urea into ammonia and carbon dioxide (increasing pH, can lead to calculi) |
|
|
how is a UTI diagnosed |
mainly on history however - may be useful toconduct dipstick MSU urinalysis (leukocytes, nitrites, microscopichaematuria), send half for urine culture and dipstick half. However need to consider trauma,contaminated sample, renal stones, UT carcinomas, glomerulonephritis also |
|
|
when should an ultrasound be performed in a person with a UTI |
if they are male, child or a patient with pyelonephritis |
|
|
what can sterile polyuria, squamous epithelial cells, mixed growth and a positive culture with no WBC count in investigations mean |
they're on antibiotics = kills bacteria but not fully treated (or TB) contamination contamination contamination (unless immunosuppressed) |
|
|
what are the treatments for a UTI |
Ural for alkalising the urine to stop burning Generally best guess treatment for antimicrobial, however nitrofurantoin, co-trimoxazole, cephalosporins cranberry juice |
|
|
what is cystitis |
bladder infection |
|
|
what is the treatment for pyelonephritis |
10-14 days PO with initial IV therapy |
|
|
what is haemolytic uremic syndrome and what causes it |
pyelonephritis can uncommonly lead to it thombotic microangiopathy --> can block glomeruli --> shows schistocytes |
|
|
what is nephrogenic and neurogenic diabetes insipidus and how can they be distinguished and how is DI diagnosed itself |
nephrogenic: kidneys fail to respond to ADH --> problem in kidneys Neurogenic = insufficient ADH secretion diagnosed by water deprivation test --> if no increase in osmorlarity of urine = DI Give desmopressin, if urine osmorlarity increases = neurogenic, if nothing = nephrogenic |
|
|
what are 3 common releases of ADH and a common inhibitor of ADH release |
Nausea, nicotine, morphine Alcohol |
|
|
what is nephrotic syndrome and nephritic syndrome |
A list of symptoms characterised by proteinuria and thus hypoalbumaemia and oedema. The lost of protein causes the liver to become highly active and mistakenly produce a lot of lipids = hyperlipidaemia Nephritic syndrome, a list of symptoms characterised by small pores in the podocytes large enough for proteins and RBCs = haematuria (dysmorphic due to stress of going through membrane), proteinuria and possible hypoalbumaemia Difference = blood in urine |
|
|
What is glomerulonephritis (GN) |
a collection of bilateral renal diseases, which are due to autoimmunity pathology, not pathogens. It can be both primary and secondary (systemic such as lupus/diabetes) |
|
|
what is a common hallmark of GN |
tubulointerstitial inflammation (space between nephron and peritubular capillaries) |
|
|
What are the common presentations of GN (6) |
Macro/microscopic haematuria, proteinuria and hypoalbumaemia, oedema, acute/chronic renal failure, high BP and salt and water retention |
|
|
What are the common causing of blockages within the nephron associated with GN |
antigens (both auto and foreign) depositing in the kidney complement complexes IgG and IgA lymphocytes (T cells, macrophages and neutrophils) due to infiltrating and clogging the nephron, releasing cytotoxic chemicals and damaging it Non-immune causes --> diabetes causes damage due to long term hyperglycaemia, hypertension, ischaemia, amyloidosis, lupus --> attack nephron damaging it |
|
|
How is GN diagnosed |
History Examination BP examination Urinalysis and microscopy: dysmorphic RBC, protein, RBC casts, light microscopy (stains), immunofluorescence (for Ab) and electron microcopy Renal function Imaging renal ultrasound should always be done Serum autoantibodies and FWT Renal biopsy (only used when therapy is hinged on it, information on prognosis or defining a systemic illness --> sticking needle in highly perfused area) |
|
|
What is minimal change GN (minimal change nephropathy), who it is prevalent in, its treatment and complications and prognosis |
It is the loss of the negative charges on the basement membrane, allowing protein to leak through. It also involves loss of podocyte foot processes, vacuolation, growth of microvilli on podocytes and fusion of the foot proceses very prevalent in children (78% of nephrotic syndrome) serve oedema (due to protein loss) Treated with prednisolone with a good prognosis in 6-8 weeks. |
|
|
What is focal and segmental glomerulosclerosis, its complications, prognosis and treatment |
Glomerular scarring (sclerotic lesion) that affect some glomeruli in only some parts of the glomerulus can be due to infections, toxins (heroin), or familiar Tends to be the dark side of minimal change GN, which tends to get worse and does not respond to prenisolone often causes progressive renal failure |
|
|
what are the GN classifications |
Central (inmesangium) or peripheral (capillary loops/GBM) Affect allglomeruli (diffuse) or some (focal) Occur in only partof a glomerulus (segmental) or the whole glomerulus Cells and fibrin canclog up the urinary space of the capsule – cresenteric (RPGN) Be proliferative(mesangial cells and immune cells) or not |
|
|
what is membranous GN, its causes, prognosis and treatment |
Thickened GBM, with diffuse granular uptake of IgG (type III hypersensitivity). Primary causes: autoimmunity Secondary: SLE. drugs (gold, mercury), cancers of lung and bowel, infections (hepatitis, malaria) 1/3 rule --> 1/3 remain with MGN, 1/3 continue, 1/3 progress Treated with prednisolone, cyclophosphamide for as risk subgroups |
|
|
What is acute streptococcal GN, cause, complications, presentation, prognosis |
it is GN precipitated by a previous group-A beta-haemolytic strep infection. It is a type III hypersensitivity, whereby the Ab to the strept are just the right size and shape to clog and get stuck in the glomerulus. After the deposition, mesangial cells and WBC proliferate in the glomeruli and becoem trapped = blocked and inflammed. The ones that are left become excessively permebale (allowing protein and RBCs) into filtrate Presents with a history of infection, with macroscopic haematuria and proteinuria, HT and oedema Usually subsides in 2 weeks and function normally returns. However glomeruli can be damaged beyond repair = progressive deterioration and chronic renal failure |
|
|
what is IgA GN, its presentation, who it usually affects, treatments and prognosis |
Mesangial IgA deposits with mesangial and matrix proliferation. it often presents with haematuria and proteinuria or asymptomatic Often affects young males after GIT/resp. infection Treated with ACEi or no treatment 33% progress |
|
|
what is Lupus nephritis, its presentations, who it usually affects, prognosis and treatments |
Its is systemic lupus with painless haematuria/proteinuria, with the immune complexes depositing in GBM Common in young women (90%) mild to severe --> 5% progress to end stage renal failure (50% of SLE cases get lupus nephritis) requires immunomodulation |
|
|
What is rapidly progressive cresenteric GN --> Its causes, prognosis, different forms and treatments |
SLE – lupus nephritis ANCA (anti-neutrophilcytoplasmic antibody) -associatedvasculitis: Anti-neutrophilcytoplasmic antibodies to myeloperoxidase – causes vasculitis. Bind to neutrophils causingthem to degranulate with ROS and sticky – and lodge in glomeruli, stimulatingimmune reaction - Necrosis, glomerularcrescent formation- Requires immunemodulation Wegener’s granulomatosis Microscopic polyangitis Polyarteritis nodosa(medium vessel vasculitis). Goodpasture’s syndrome AKA anti-glomerularbasement antibody disease glomerulonephritis --> anitbodies against structural collagen component in renal/pulmonary basement membranes- IgG → bleeding in both of thesesystems (i.e. haemoptysis).Renal failure occurs over days, months time frame Prednisolone,cyclophosphamide for the vasculitis' Immunosuppresion, plasma exchange for goodpastures. |
|
|
What does renal failure cause |
azotaemia (build up of nitrogenous waste in the blood) |
|
|
What is uraemia and what loss of renal function causes it to happen |
When renal failure is accompnaied by noticeable symptoms and requires a 80-85% function reduction |
|
|
What are the symptoms of uraemia |
anorexia, lethargy, seizures, sexual dysfunction, HT hypocalcaemia, fatigue, nausea, anaemia, acidosis, vomiting, cold, oedema, itch, shortness of breath, coma, decreased mental acuity |
|
|
what is renal failure |
a decline in the GFR, either acutely or chronically or oligouria |
|
|
what two groups of people should a normal serum creatinine be bad |
children and pregnant owmen --> children = low muscle mass and creatinine levels, pregnancy = kidneys hyperfilter the blood |
|
|
after what percentage of renal function loss does creatinine rise and why |
50% --> as function is lost, the other nephrons pick up the lost nephrons work rate |
|
|
what is classified as end stage renal failure |
less than 15% of function and dependance on replacement therapy |
|
|
what are the three classifications of acute renal failure |
pre-renal, intra-renal/renal and post-renal |
|
|
What is pre-renal failure and its prognosis |
where not enough blood gets to the kidney, generally reversible unless the blood flow is less than 25% of normal and re-perfusion does not take long |
|
|
What are the hallmarks of pre-renal failure |
low sodium in urine (trying to bolster blood pressure), highly concentrated urine, no dysomorphic cells in urine |
|
|
What are the main causes of pre-renal failure (6) |
Hypovolaemia (dehydration, blood loss, diarrhoea/vomiting, polyuria) Cardiovascular (heart failure, negative inotropic drugs e.g. beta-blockers, CCBs) Septicaemia (generally gram negative bacterial endotoxins --> can also initiate disseminated intravascular coagulation = widespread clotting activation = fibrin and platelet deposition in renal arteries microangiopathic haemolysis = schistocytes = ischaemia with hallmark of schistocytes and decreased platelet count as they were consumed in the DIC) anaphylaxis --> shock Liver failure (hypoalbumaemia = oedema = less cirulating volume) Renal artery stenosis (acute occlusion of a stenotic vessel, NSAIDs and ACEi are also do it, as the afferent will no longer dilate, and the efferent no longer constricts = much lower GFR in stenotic vessels) |
|
|
What are the main causes of intrarenal failure |
GN: Glomerular damaged and blocked by multiple things = down GFR) Tubulointerstital injury: Acute tubular necrosis Interstitial nephritis: inflammation of nephrons affecting interstitium, caused by drugs (cillins, NSAIDs, analgesics, diuretics, systemic such as SLE, sarcoidosis) Vascular injury: HT, vasculities |
|
|
What is acute tubular necrosis, the two types of it and their causes |
Ischaemic ATN Toxic ATN Ischaemic ATN: inadequate supply blood, generally due to unresolved prerenal ARF --> the dead cells then slough off and plug the nephron = oligouria = bad prognosis --> diuretics to try and preserve Toxic ATN: noxious substances destroy the tubular epithelium --> cells slough off and plug nephron again and no blood enters (can be repaired if BM is not damaged) Caused by endogenous toxins: crush syndrome (myoglobin), calcium, haemoglobin (microangiopathy) and IgG light chains in myeloma and urate in GOUT Caused by exogenous toxins: mercury, lead, cisplatin, vancomycin, lithium, gentamicin, amphotericin, radiological contrast, recreational drugs, lipid lowering drugs, acyclovir/indinavir (crystals) and also drugs which mess with the perfusion such as ACEi, AIIRAs, NSAIDs |
|
|
what are the post-renal causes of acute renal failure and what is always needed to rule it out and what indicates it |
Obstruction (which leads to hydronephrosis) --> bilateral (always unless pre-exisiting lost renal function as blockage in one = 50% of function still remaining) An ultrasound should always be done to ensure no hydronephrosis Generally auria will indicate as cannot get past blockage |
|
|
what differentiates chronic from acute renal failure |
anaemia (in chronic), small kidneys (diminishes in CRF), renal bone disease (reduced vit D), peripheral polyneuropathy (ureaemic toxins = axonal degeneration) |
|
|
What are the 3 most common causes of chronic renal failure and their percentages |
GN (35-45%) Diabetes mellitus (15-30%) HT (5%) |
|
|
what is the diagnosis of chronic kidney disease |
less than 60mL/min of filtration for 3 months = more than half of renal function lost |
|
|
What effect does CRF have on the kidney's concentrating ability |
It reduces it --> the blood flow of the damage nephrons diverts to the remaining nephrons --> rapid flow of blood in remaining nephrons is isosthenuria– inability of the renal tubules to concentrate/dilute the urine by virtue of rapidflow → decreased water reabsorption and ↓countercurrent mechanismconcentration of medullary interstitium. |
|
|
What are the causes of chronic kidney failure |
Vascular: No collateral circulation in kidney = sclerotic vessel, atherosclerosis or fibromuscular hyperplasia = all supplied nephrons damaged Glomerular GN or amyloidosis Interstitial Infection --> long standing/recurrent pyelonephritis Pharmacological compound analgesic use (NSAIDs, aspirin), reduce GFR by reducing afferent vasodilation |
|
|
How does haemodialysis work |
AV fistula catheterised --> blood moves into machine which has a semi-permeable membrane that causes diffusion of particles into the fluid flowing the opposite direction past it, with the waste at very low levels in diaylsate = diffuse across or it is done with the peritoneum acting as the membrane, whereby it absorbs all the bad stuff out of the peritoneum and puts good stuff back |
|
|
Where is a transplanted kidney placed and what vessels is it connected to |
In the illiac fossa and it is connected to external/common illiac vessels |

