![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
15 Cards in this Set
- Front
- Back
|
List the causes of toxic and ischemic AKI/ATN
|
AKI (Acute Kidney Injury) / ATN (Acute Tubular Necrosis)
Ischemic: BP drop, severe trauma, acute pancreatitis Toxic: Drugs (ABX), contrast dyes, poisons (heavy metal), organic solvents Combined: mismatched blood transfusion/other hemolytic crisis (hemoglinuria), skeletal muscle injury (myoglobinuria) |
|
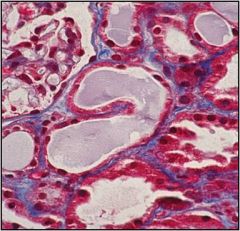
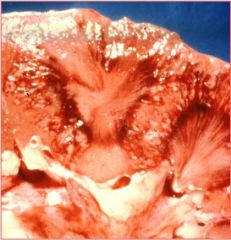
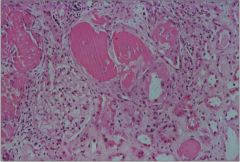
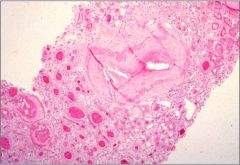
Name the problem, describe how it affects the tubules and describe the changes seen in this image
|
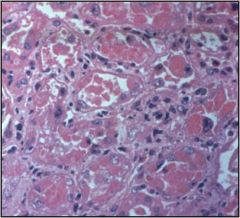
Acute Kidney Injury occurs as a result of either ischemic or toxic injury. Ischemic injury will occur at random locations throughout the tubules whereas toxic injury will occur in a more diffuse pattern.
In the slide there are fewer nuclei and the surviving cells are stretching out to try and cover the exposed basement membrane. In the second image there are cells that are beginning to slough off |
|
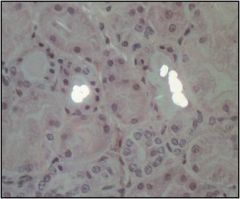
What causes this injury? What are the bright white things?
|
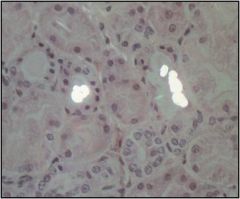
Antifreeze poisoning, under polarized light the calcium oxalate crystals light up
|
|
|
Is AKI/ATN reversible?
Why or why not? |
With supportive care, the tubular epithelium can regenerate and renal function can be restored. During the recovery phase there is polyuria because the glomerular filtrate cannot be adequately reabsorbed by the damaged tubular epithelium
|
|
|
Describe vesico-ureteral reflux and its significance
|

Vesicoureteric reflux can occur in kids who have a short intravesicular portion of the ureter (it is normally smaller and longer than in this image and gets compressed when the bladder contracts during micturation). In people iwth short intravesicular ureters the bladder does not completely close the ureter and there is reflux of urine into the kidney... this can cause TUBULO-INTERSTITIAL NEPHRITIS
|
|
Describe Acute pyelonephritis both grossly and histologically
|
Little abscesses on cross section and morphologically there are PMNs and various degrees of necrosis involving mainly tubules and interstitium. In general, the glomerulus is relatively spared.
|
|
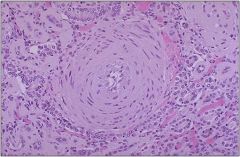
Name the disease that causes this and explain what can cause it
|
Chronic Pyelonephritis has an insidious onset that causes scarring of the kidney and gradual renal insufficiency. The first signs are loss of concentrating ability (polyuria & nocturia). It is usually associated with Chronic obstructive pyelonephritis and reflux nephropathy.
Histologically we see sclerosed glomeruli, dilated tubules "thyroidization", and interstitial lymphocytes |
|
|
What is Xanthogranulomatous pyelonephritis? What causes it?
|

It is typically caused by infection with Proteus spp or obstruction with stones. This infection tends to extend beyond the renal capsule and form a mass that may mimic cancer
|
|
|
Describe what causes acute drug-induced interstitial nephritis and the clinical signs and symptoms
|
Acute drug induced interstitial nephritis is caused by IgE and T cell mediated reaction to a drug with abundant EOSINOPHILS. It is caused most commonly by synthetic ABX, diretics and NSAIDs. Pt will present with a maculopapular rash, proteinuria, hematuria and urine sediment will show EOSINOPHILS
|
|
|
Name three diseases that can be caused by NSAIDs that effect the kidney
|
Hemodynamic effect by inhibition of prostaglandin synthesis
Acute hypersensitivity interstitial nephritis Interstitial Nephritis associated with Minimal Change Disease (nephrotic syndrome) |
|
|
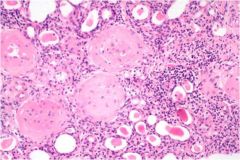
Understand causes of tubulointerstitial nephritis associated “myeloma kidney”
|
Multiple myeloma (plasma cell cancer) can secrete tons of monoclonal Ig light chains that circulate in the blood that lodge and precipitate and obstruct the distal tubules of the kidney.
Note that multiple myeloma is a lytic bone lesion (hypercalemia), and causes increased cell turnover (hyperuremia) |
|
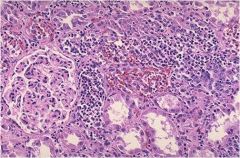
What is causing this? Describe the
|
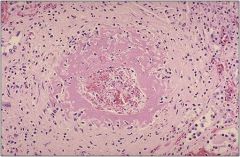
Malignant hypertension with necrotizing arteriolitis (this slide) and hyperplastic arteriosclerosis (previous slide)
It is associated with malignant HTN (BP>200/100) |
|
|
Describe HUS
|
Hemolytic Uremic Syndrome is caused by E. coli. Shiga toxins produced by the bacteria cause endothelial injury and can cause renal failure, thrombocytopenia and form shistocytes. Patients will have normal coagulation times (vs someone with vWF deficiency)
|
|

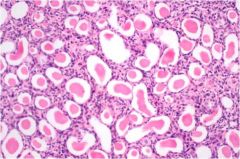
Describe what is going on here.
|
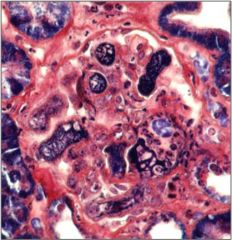
HUS
Some normal capillaries, but others are DISTENDED.. The mesangium ballooned and dissappeared. The red stuff are RBCs and the pink is FIBRIN. There are fibrin thrombi in glomeruli and extraglomeular small vessels caused by injury to endothelial cells (previous slide). On this slide a PTAH stain was done which turns fibrin navy blue |
|
Understand the renal and systemic impact of atherosclerosis
|

Atheroemboli can form in interlobar arteries causing wedge shaped infarcts.
Livido reticularis (vascular rash) caused by secondary cholesterol emboli loding in the legs |

