![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
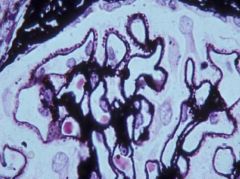
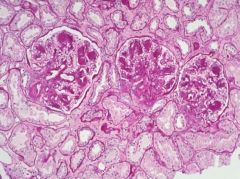
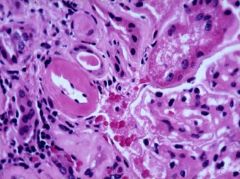
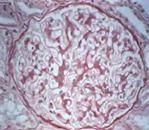
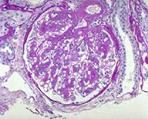
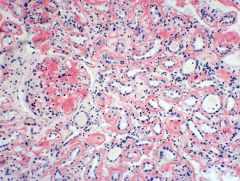
-Membranous nephropathy
-There is thickening of the capillary wall due to the basement membrane developing spikes |
|
|
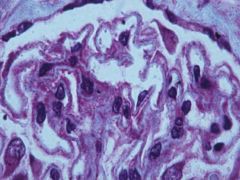
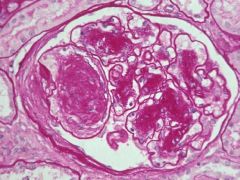
-Membranous nephropathy
-These are spikes reacting to the presence of deposits that stain red on the outside of the glomerular capillary walls -These are immune deposits in the glomerulus on the outer aspect of the glomerular wall and the spikes form between them |
|
|
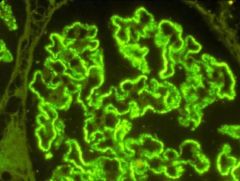
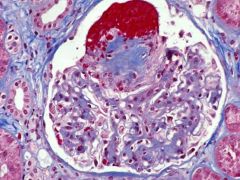
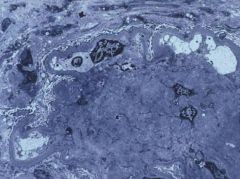
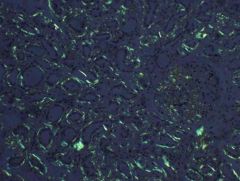
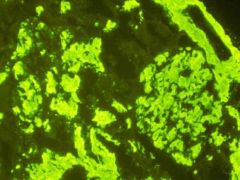
-Immunofluorescence of membranous nephropathy
-IgG and C3 present all over the capillary walls of the glomerulus -There is a finely granular pattern represents the deposits we saw with the trichrome stain |
|
|
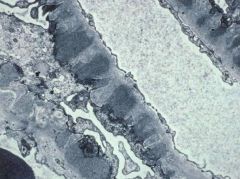
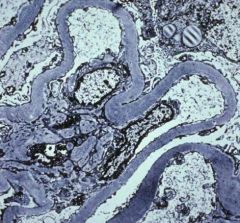
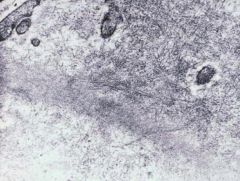
-EM of membranous nephropathy
-Electron dense deposits along the outer aspect -You can see subepithelial deposits and they are seperated by projections of basement membrane material which form in reaction to the deposits |
|
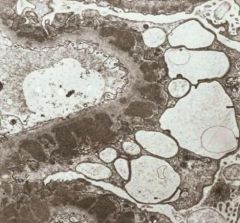
|
-Membranous nephropathy
-Lumen is patent -No proliferative response, but there are many subendothelial electron deposits seperated by basement membrane spikes -Podocyte is severely injured, foot processes effaced and podocyte hypertrophy in response to immune deposition in the capillary wall in this subepithelial distribution |
|
|
What conditions are associated with membranous glomerulopathy
|
-Primary 40%
-Secondary (60%): -Infections -Hep B, Hep C, secondary and congenital syphilis, malaria, schistosomiasis -Drugs -Gold, penicillamine, captopril -Collagen vascular disease -SLE, Hashimoto's thyroiditis, Rheumatoid Arthritis |
|
|
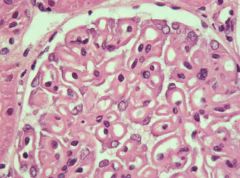
-Membranous glomerulopathy
-There are thick basement membranes -The glomerulus and every capillary loop looks thickened -Not a proliferative process |
|
|
Describe the formation of immune complexes in membranous glomerulopathy
|
-Happens in situ
-There is first an antigen that forms and then an antibody binds to it at the level of the capillary wall -These patients dont have circulating immune complexes and dont have low serum complements -The antigen is one produced normally by the visceral epithelial cell -The antibody binds to it in situ leading to immune complex formation, capping, and shedding off the soles of the foot processes |
|
|
Describe the consequences of immune deposit formation in membranous glomerulopathy
|
-Antigen-antibody complex formed
-Binding of complement -Formation of C5b-9 complex -Activation of Glomerular visceral epithelial cell -Scavenging of C5b-9 -Increased expression of cytochrome b -Formation of ROS -Deposition of ROS in GBM -Protienuria |
|
|
What is the target antigen in human membranous glomerulopathy?
|
-Phospholipase A2 receptor
-The phospholoipase A2 receptor is a receptor present on the clathrin coated pits at the soles of the foot processes. |
|
|
Describe membranous nephropathy
|
-Most common etiology of nephrotic syndrome in white adults
-Course variable -Renal survival at 10yr: 65-85% -Renal survival at 15yr: 60% -Spontaneous remission rate: 20-30% |
|
|
What is the most common cause of idiopathic nephrotic syndrome in whites?
|
Membranous Nephropathy
|
|
|
What is the most common cause of idiopathic nephrotic syndrome in blacks?
|
Focal segmental glomerulosclerosis
|
|
|
Describe the Treatment of Membranous Nephropathy
|
-Conservative Therapy
-Corticosteroids -Alternating Steroids-Cytotoxics -Cyclosporine -Mycophenolate -Anti-C5 Ab, Rituximab -Different people respond to different modulating drugs |
|
|
Describe Thrombotic abnormalities in the nephrotic syndrome
|
-Lots of anti-clotting factors are lost in the urine
-Liver turns on -Increased coagulation tendency (platelet hyperaggregability, high fibrinogen and fibrinogen-fibrin transfer, decreased fibrinolysis, low anti-thrombin III) -DVT, RVT, pulmonary emboli -Membranous NS greatest risk (up to 35%), associated with RVT -Most RVT asymptomatic, but flank pain, microhematuria, low GFR |
|
|
Describe the opthalologic exam results of diabetes
|
-Retinopathy
-Exudate, hemorrahges, and microaneurysms present |
|
|
Describe the types of Diabetes Mellitus
|
-Type I - Insulin Dependent (hypoinsulinemic, ketotic, juvenile onset)
-Rare, 5-10% of patients -Type II - Non-Insulin Dependent (Normoinsulinemic, non-ketotic, maturity onset) -Adult onset -May have end organ resistance to insulin -Closely linked to obesity |
|
|
Describe diabetic nephropathy
|
-40-50% of diabetic patients develop it
-Just as likely with both types of diabetes |
|
|
Why is there basement membrane thickening in diabetes mellitus?
|
Hyperglycemia leads to non-enzymatic glycosilization of basement membranes throughout the body
|
|
|
Describe where the basement membrane thickening in diabetes mellitus occurs
|
-Vascular basement membrane
-Glomerular capillaries -Muscle capillaries -Retinal capilaries -Arterioles -Other basement membrane -Renal tubules -Mammary ducts -Schwann Cells |
|
|
How do we measure the amount of glycosilization taking place throughout the body in diabetic nephropathy?
|
Hemaglobin a1c
|
|
|
Describe how glycosolization of the glomerular basement membrane leads to nephropathy
|
-The basement membranes thicken and there is an accumulation of circulating plasma proteins
-This causes defective mesangial clearing which leads to mesangial sclerosis -There is decreased sialic acid content content and increase cationic charge -This decreases GBM degradation, increase GBM synthesis and leads to proteinuria -There is increased disulfide bonding GBM collagen -This further decreases GBM degradation and increases GBM synthesis |
|
|
Describe the progression of diabetic nephropathy
|
-Early Stage: Microalbuminuria
-Late Stage: Proteinuria -End Stage: ESRD -Intervene in the early stages. The end stages require dialysis and transplant. |
|
|
What are the current strategies to limit renal injury in diabetic nephropathy?
|
-Blood pressure reduction
-Inhibition of the renin-angiotensin-aldosterone axis -Blood sugar control -Metabolic manipulation |
|
|
Describe the pathology of amyloid
|
-LM: A homogenous, hyaline eosinophilic, proteinaceous substance
-Special stains: -Congo red -Methyl violet -Thioflavin t -EM -Fibrillar constituent -Random arays of non-branching fibrils, 80-100A in width, beading with 55A periodicity -Non-fibrillar constituents -Pentameric discs (AP protein) -X-ray diffraction: beta pleated sheet conformation |
|
|
Describe Primary "AL" amyloid
|
-Cause: Dysproteinemias
-Precursor Protein: Light chains -The AL type are patients with a neoplasm of plasma cells of B lymphocytes that produces an abnormal immunoglobulin and free light chain that can be deposited in the kidney as amyloid. |
|
|
Describe Secondary "AA" amyloid
|
-Cause: Longstanding inflamatory or infectious states
-Precursor protein: SAA-protein (acute phase protein) -The SAA protein is made by the liver. Some patients may be predisposed to this because they have the ability to catabolize this SAA protein to intermediate proteins that resist further degradation and undergo fibrinogenesis in the tissues. |
|
|
What chronic diseases are associated with "AA" amyloidosis?
|
-Rheymatoid arthritis
-TB -Leprosy -Chronic osteomyelitis -Paraplegia -Chronic bronchiectasis -Cystic Fibrosis -Chronic heroin addiction -Psoriasis -Familial Mediteranean Fever |
|

|
-Membranous Glomerulopathy
-Subepithelial deposits -Antigen is one produced normally by visceral epithelial cells -Antibody binds to it in situ leading to immune complex formation, capping, and shedding off the soles of the foot processes |
|
|
-Abdominal angiogram
-There is a clot in the right kidney -Renal vein thrombosis -Coagulation tendency from membranous nephropathy |
|
|
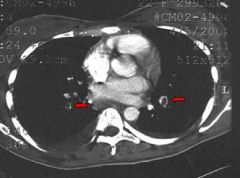
-Chest angiogram
-Clots present int he pulmonaru arteries -Coagulation tendency from membranous nephropathy -This peson has a renal vein thrombosis and spun off clots through the venous system that landed in the pulmonary system causing acute SOB |
|

|
-Clot in the renal vein
-Associated with membranous nephropathy |
|

|
-IVCogram
-Upper pole of kidney is not seen -There is a filling defect: clot in the renal vein -Membranous nephropathy |
|

|
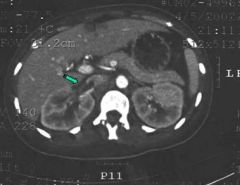
-CT angiogram
-One normal kidney and one swollen one -Can see a clot going from the renal vein right into the IVC -Associated with membranous nephropathy |
|

|
-Membranous nephropathy
-Was admitted for SOB and chest pain -Developed dilated veins from the hypogastic all the way to the axillary vein -Had partial IVC occlusion and total renal vein thrombosis |
|

|
-Diabetic retinopathy
-There is exudate, hemorrhages, and microaneurysms |
|
|
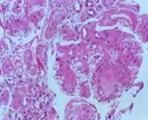
-Diabetic nephropathy
-Thickening of basement membrane components throughout the kidney -Increased matrix within the mesangium of the glomerulus, mesangial sclerosis -Thickening of glomerular basement membrane -Very diffuse -Called diabetic glomerular sclerosis |
|
|
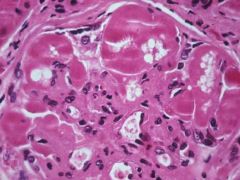
-Diabetic nephropathy
-Mesangial sclerosis can become more accentuated forming large nodules -Nodule form of diabetic glomerular sclerosis -Nodules are Wilson nodules -Basement membrane thickened throughout the glomerular tuft |
|
|
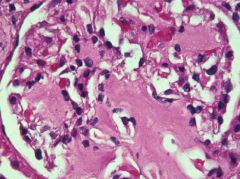
-Diabetic nephropathy
-We can develop aneurysms filled with RBCs in the glomerulus -Dont often develop the renal manifestations of diabetes unless we also have the retinal manifestations -Retinopathy and nephropathy both may have aneurysmal formation in these specialized capillary beds |
|
|
-Diabetic nephropathy
-Partial sclerosis leads to entrapment of circualting plasma protien causing hyalinosis -Often lipid that is admixed with these plasma proteins -The presence of IgM indicated the entrapement of circulating plasma material -There is hyalinosis of the glomerulus together with the sclerosis |
|
|
-Diabetic nephropathy
-All the basement membranes in the kidney are affected -Arteriole sclerosis and arterioloscleros develop -Glassy eosinophilic material (hyalin) present -It is pushed into the sclerotic basement membrane of the vessel walls |
|
|
-EM of diabetic nephropathy
-No immune deposits, defect is metabolic -Glycosilization of basement membranes leads to sclerosis of the mesangium and thickening of all the basement membranes -Thickened basement membranes abnormally leaky to proteins due to icnreased cationiic charges |
|
|
-EM of diabetic nephropathy
-In the nodular form you can see that the mesangial scelrosis is so exuberant that it really does for a nodular aggregate of extracellular material that can compromise the capillary loops |
|
|
-Diabetic nephropathy
-Stained for advanced glycosilization end products -Deposition of nodules as well as thickened glomerular basement membranes, Bowman's capsule, and the tubular basement membrane |
|

|
-Diabetic nephropathy
-As kidney goes into end stage renal failure it maintains a relatively large size due to basement membrane material that has been deposited -Kidney not functioning but close to normal size |
|
|
-Diabetic nephropathy
-Mesangial expansion -Hyperfiltration |
|
|
-Diabetic nephropathy
-GBM thickening -Microalbuminuria |
|
|
-Diabetic nephropathy
-Glomerulosclerosis -Proteinuria |
|
|
What is the BP goal in hypertension with no diabetes or renal disease?
|
<140/90
|
|
|
What is the BP goal in diabetes mellitus?
|
<130/80
|
|
|
What is the BP goal in renal disease with proteinuria>1gm/day or diabetic kidney disease
|
<130/80
<125/75 |
|

|
Rheumatoid hands
|
|
|
-Amyloidosis
-Replaced portions of the mesangium and has extended out and compromised some of the capillary loops -In the advanced stages the glomulus can be completely replaced by amyloid material -Looks eosinophilic can be hard to differentiate from basement membrane material |
|
|
-Amyloidosis
-Congo red stain makes amyloid orange -Amyloid has deposited in every compartment of the kidney |
|
|
-Amyloidosis
-On polarization we get apple green birefringence |
|
|
-EM of amyloidosis
-No immune deposits -Many fibrils that range from 8-12nm -Glomerular BM is overrun by fibrillar material (amyloid) -Disruption of the GBM by amyloid alters the selectivity of the capillary wall leading to albuminuria and in the worst cases nephrotic syndrome |
|
|
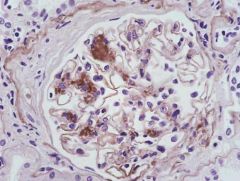
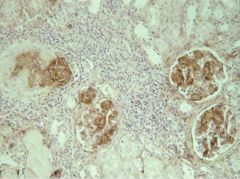
-Amyloidosis
-Precursor protein in rheumatoid arthritis is amyloid A -Immunostain of these glomeruli will be positive for serum amyloid A protein telling us that the cause is RA |
|
|
-Amyloidosis
-Patient has myoloma -Stained with lambda light chain -Distribution of the glomerular tubular and vascular basement membrane |
|

|
-Amyloidosis
-Deposits in all compartments can lead to end stage kidney disease -Kidney stays large |

