![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
Describe nephrotic syndrome
|
-Glomerular disease associated with heavy albuminuria (>3-3.5 g/day)
-You have: -Hypoalbuminemia -Edema -Hyperlipidemia -Thrombotic tendency |
|
|
Describe the genesis of hypoalbuminemia
|
-Glomeular disease leads to proteinuria
-Much of the albumin that gets filtered gets past the glomerular capillary wall and can be reabsorbed by the proximal tubule -The proximal tubule can reabsorb some of it and catabolize it -The rest comes out in urine -The catabolism and the proteinuria lead to hypoalbuminemia |
|
|
Describe the edema of the nephrotic patient
|
-Periorbital edema in the morning
-Leg and pedal edema at the end of the day |
|
|
Describe the first theory of pathogenesis of nephrotic edema
|
-Hypoalbuminemia
-Low plasma oncotic pressure -Increased capillary filtration -Decreased plasma volume -Secondary renal Na rention -Na and water retention -High hydrostatic pressure |
|
|
Describe the second theory of pathogenesis of nephrotic edema
|
-Glomerular disease
-Proteinuria -Causes hypoalbuminemia and primary renal sodium retention -Increases plasma volume -Increases capillary filtration -Leads to edema |
|
|
Describe the therapy of edema in nephrotic syndrome
|
-Put the patient on a low Na+ diet
-Use oral loop diuretics -Start with low dose - double doses -Add zaroxolyn -+/- high BID doses -IV diuretics and colloid rarely needed -Goal is 1-2 lbs edema loss/day -Fluid comes from intravascular space -If you remove too fast the patient goes into shock |
|
|
Describe lipiduria
|
-Manifestation of nephrotic syndrome
-Cholesterol and cholesterol esters and other lipoportiens enter urine -Oval fat bodies/Maltese crosses in urine |
|
|
Describe cholesterol levels in patients with nephrotic syndrome
|
High
-87% have >200 mg/dl -53% have >300 mg/dl -25% have >400 mg/dl -LDL is high as well |
|
|
What are the most common causes of nephrotic syndrome?
|
-Idiopathic
-Membranous nephropathy (most common in white americans) -Focal sclerosis (most common in black americans) |
|
|
Describe treatment of hyperlipidemia of the nephrotic syndrome
|
-Select high risk patient (high LDL, low HDL, unlikely to rapidly remit)
-Attempt to induce a remission of the proteinuria (ACEi/ARBs, specific immunosuppressives, etc) -Dietary therapy -Medical therapy (statins +) |
|
|
Describe treatment principles of nephrotic syndrome
|
-Treatment of primary disease - often immune modulating medications
-Syptomatic treatment - diuretics, statins, diet, in some anticoagulation -Reduction of proteinuria/slowing progression -Makes it easier to treat the edema, hyperlipidemia, etc |
|
|
What are the goals of treating nephrotic patient?
|
1) Decrease the proteinuria, correct the edmea, hyperlipidemia
2) Try to prevent eventual scarring of the glomerular filters |
|
|
Describe how to reduce proteinuria and slow progression
|
-Blood pressure reduction
-Inhibition of the renin-angiotensin-aldosterone axis |
|
|
What is the relationship between blood pressure and the decline in GFR?
|
The lower the BP the slower the loss of kidney function
|
|
|
Which BP medications are better for the kidney?
|
-Diuretics, ACEi, AII receptor blockers are the treatment of choice in anyone with proteinuria
-These lower proteinuria -The ACE inhibitor lowers proteinuria because you opened up the efferent arteriole coming out of the glomerulus, resulting in less pressure in the glomerular capillaries, less proteinuria and less glomerular scarring over time. |
|
|
What is the most common cause of nephrotic syndrome in young children?
|
Minimal change disease
|
|
|
Describe Minimal Change Disease
|
-Also called Lipoid nephrosis
-Proximal tubules become stuffed with reabsorbed lipid -Patients lose protein and become hypoalbuminemic -Liver starts synthesis of proteins and cholesterol -Kidney filters lipid and the tubules reabsorb it and get stuffed |
|
|
What are the synonyms of Minimal change disease?
|
-Nil disease
-Lipoid nephrosis -Childhood nephrosis |
|

|
-Nephrotic disease
-Left: Periorbital edema -Right: Leg and pedal edema |
|

|
-Child with periorbital, leg, and pedal edema indicating nephrotic disease
-Likely minimal change disease |
|

|
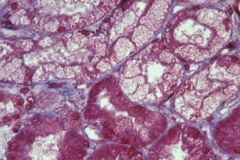
-Minimal change disease
-Kidney looks as if it is filled iwth lipid -Yellow instead of brown |
|
|
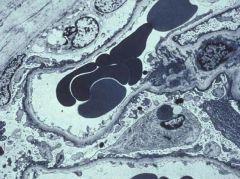
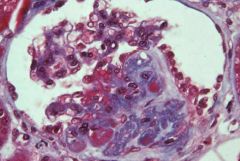
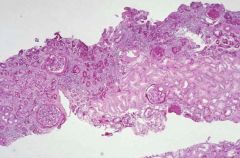
-Minimal change disease
-Proximal tubules are stuffed with reabsorbed lipid -Liver has ramped up production of cholesterol and the kidney is filling up trying to reabsorb it |
|
|
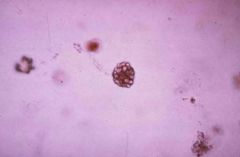
-Urine sediment for a patient with minimal change disease
-Oval fat bodies present |
|
|
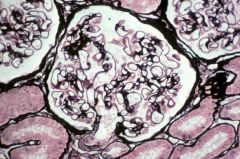
-Glomeruli in minimal change disease
-No obvious abnormalities |
|
|
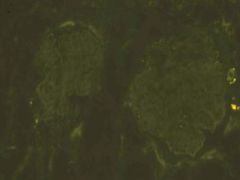
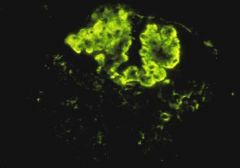
-Immunofluorescence in minimal change disease
-No immune deposits |
|
|
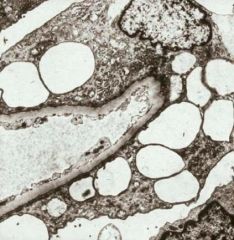
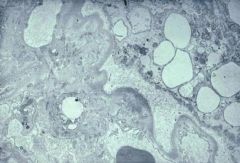
-EM of minimal change disease
-Podocyte foot processes have been effaced |
|
|
-EM of minimal change disease
-Podocyte foot processes have been effaced -Podocyte has filled with transport vesicles |
|
|
Describe the evidence for immunologic derangements in Nil Disease
|
-Viral infections may precede onset or recrudescences
-May follow recent immunizations -Altered in vitro response to mitogens -Circulating lymphocytotoxins -Association of Hodgkin's Disease and other lymphoproliferative disease -There may be a circulating factor produced by the lymphocyte that is acting at a distance to cause some injury to the podocyte. |
|
|
Describe Minimal Change Disease
|
-5-10% of adults with idiopathic nephrotic syndrome, >85% of children
-Usually sudden onset, heavy proteinuria, and edema -High BP 30%, Microhematuria 30%, +/- low GFR -Course: Responds to steroids, relapse, no renal failure as long as you get rid of the proteinuria |
|
|
What is the most common cause of nephrotic syndrome?
|
Diabetes
|
|
|
Describe the pathology of Minimal change disease
|
-Normal under light microscopy
-Immunofluorescence negative -EM shows fused podocyte feet |
|
|
-Focal segment glomerulosclerosis
-Involves some glomeruli and not others -Affects glomeruli segmentally |
|
|
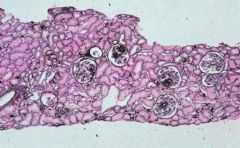
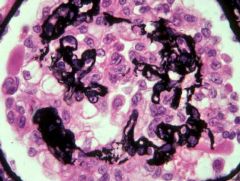
-Focal segmental glomerulosclerosis
-Increase laying down of ECM segmentally -Neighboring capillaries look normal, but have effaced foot processes |
|
|
-Focal segmental glomerulosclerosis
-Areas of scarring have entrapment of hyaline (red staining) -There are plasma proteins such in areas of sclerosis |
|
|
Describe the laying down of new basement membrane in focal segmental glomerulosclerosis
|
-This shows the segmental nature of the laying down of this basement membrane material which obliterates the glomerular capillaries.
-Over time more and more of the tuft is replaced by this matrix material until the sclerosis goes from segmental to global. |
|
|
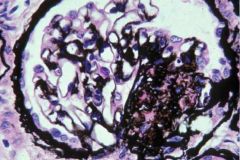
-Immunofluorescence panel for focal segmental glomerulosclerosis
-IgM present -Large MW cause in areas of sclerosis (byproduct of sclerosis) -IgM not pathogenic, but helps identify disease |
|
|
-EM of Focal segmental glomerulosclerosis
-Podocytes have fused foot processes (more severe than minimal change disease) -Produces non-selective proteinuria -Podocyte has lifted off the sclerosing glomerular basement membrane |
|
|
Describe the progression of focal segmental glomerulosclerosis
|
-Over time disease progresses to end stage renal failure
-Along the way segmentally sclerotic glomeruli become globally sclerotic -Entire tuft replaced by matrix material (collagen IV) -There is dependent atrophy for the more distal portions of the nephron because glomeruli sclerose and cant pass filtrate |
|
|
-Focal segmental glomerulosclerosis
-End stage, more global |
|
|
-Focal segmental glomerulosclerosis
-From a patient with a single kidney |
|
|
Describe the cause of primary focal segmental glomerulosclerosis
|
Circulating factors
|
|
|
Secondary FSGS can be due to adaptive responses of what?
|
-Reflux nephropath: urine reflux to kidney can cause repeated injury
-Renal agenesis (solitary functioning kidney) -Any chronic renal disease: Once you have lost a certain number of nephrons you get progressive hyperfiltration in the remnant nephrons driving increased segmental and global sclerosis in the remaining filtering nephrons. -Obesity |
|
|
How does obesity lead to focal segmental glomerulosclerosis?
|
In obesity the glomerulus becomes stressed. The kidney has an increased need in filtration to service this whole body and the strain on the glomerulus leads to adaptive responses that over the long term become maladaptive, leading to sclerosis.
|
|
|
Describe the mechanism of how obesity or a solitary kidney leads to focal segmental glomerulosclerosis
|
-Decrease in resistant of both afferent (more) and efferent (less) arteriole leading to increased capillary flow
-Elevated glomerular hydrostatic pressures develop -Leads to glomerular hypertension -Tension on capillary wall increases radius -Large hypertrophies glomeruli leads to microaneurysmal dilations -Podocytes stretch, become detached, and then are lost -Over time there is progression to segmental sclerosis |
|
|
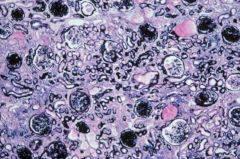
-HIV associated nephropathy
-Severe form of focal segmental glomerulosclerosis -Has a collapsing pattern of focal sclerosis where the whole tuft retracts and the podocytes undergo a peculiar hypertrophy and hyperplasia -Very progressive form -Renal failure in weeks if no antiretrovirals |
|
|
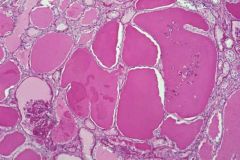
-Focal segmental glomerulosclerosis
-There is dilation of many of the tubules which increases the total kidney volume |
|
|
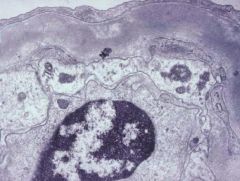
-EM of Focal segmental glomerulosclerosis
-There are tubuloreticular inclusions -There are inclusions in the endothelial cells of the glomerular capillary -These are induced by interferon -Seen in many viral infections |
|
|
Describe the pathogenic factors (known and hypothetical) in FSGS
|
-Hemodynamic: Glomerular Hyperfiltration
-Genetic: Glomerular Hyperfiltration -Immunological: Permeability factors -Toxic -Viral: HIV |
|
|
Describe focal segmental glomerulosclerosis
|
-Increased frequency >20% nephrotic syndrome
-Especially in blacks -In adults onset 2/3 NS, 1/3 proteinuria -HBP>30%, Microhematuria>30%, Renal dysfunction 50% -Predictors of ESRD: heavy proteinuria, blacks, high creatinine -On biopsy there is intimal fibrosis and collapse -Steroids >50% respond, cytoxan, cyA, MMF -Recurs 1/3 post-transplant -There is some circulating factor which is causing the permeability of those glomerular basement membranes and capillary loops to change so they are leaking albumin into the urine. |

