![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
Describe the clinical presentation of the nephrotic syndrome
|
-Heavy proteinuria
-Low serum albumin -Edema -High serum lipids |
|
|
Describe the clinical presentation of nephritis/nephritic syndrome
|
-Renal failure
-Hypertension -Hematuria -Acute -Chronic -Rapidly progressive |
|
|
What are the three categories of renal parenchymal disease?
|
-Nephritis syndrome
-Nephrotic syndrome -Asymptomatic urinary abnormalities |
|
|
Describe asymptomatic urinary abnormalities
|
A patient will present with isolated hematuria of glomerular origin or proteinuria
|
|
|
Describe the results of urine analysis in a patient with nephritic syndrome
|
-Urinary RBCs, sometimes deformed
-RBC casts -Large amounts of albuminuria (>3g/day) |
|
|
What are RBC casts?
|
RBC casts are outlines of red cells with tubules and protein matrix. If you see these you are usually dealing with a glomerular disease.
|
|
|
Describe why the glomerulus is vulnerable to immune complex injury
|
1. Receives 20-25% of CO
2. High glomerular capillary pressure 3. Fenestrated endothelium 4. Concentration (sieving effect) |
|
|
What are the mechanisms of immunologic injury to the glomerulus?
|
1. Glomerular deposition of circulating Ag-Ab complexes. The antigen-antibody complexes can get trapped in the glomerulus because of charge interactions, size, and affinity for the capillary walls.
2. Binding of circulating Ab to fixed glomerular Ag (ie, anti-GBM Ab) 3. In situ immune complex formation. In situ immune complex formation is either due to an antigen being produced by the visceral epithelial cell or because it gets planted first and then antibody binds. |
|
|
Describe the appearance under immunofluorescence with glomerular deposition of circulating Ag-Ab complexes
|
Granular appearance
|
|
|
Describe the appearance under immunofluorescence with in situ immune complex formation
|
Granular appearance
|
|
|
Describe the appearance under immunofluorescence with binding of circulating Ab to fixed glomerular Ag (ie anti-GBM Ab)
|
Linear
|
|
|
How does antigen-antibody deposition lead to disease?
|
-Antigen-antibody complexes form in the glomerular capillary wall
-There is activation of complement through the classical pathway -C3a and C5a are produced which are chemotaxins and attract neutrophils and sometimes monocytes to the glomerular capillary lumen -Leukocytes undergo respiratory burst, releasing ROS, lysosomes, and proteases -This causes damage to the capillary wall and leads to a proliferative response -Hagemen factors activates leading to the formation of fibrin, plasmin, and kinins -Platelets come in to plug these areas and release factors that cause mesangial proliferation -This can lead to glomerulonephritis and eventually glomerulosclerosis |
|
|
Describe the different types of glomerular proliferation
|
-Proliferation of the mesangium (mildest form)
-Endocapillary-proliferation in the glomerular capillary lumen which occludes the lumen. These areboth mesangial and endothelial cells. The indigenous cells of glomerulus as well as infiltrating leukocytes that cause all the hypercellularity in the glomerular tuft. -Extracapillary (cresentic)-(most severe) The proliferating cells are the cells that normally line Bowman's capsule - the parietal epithelial cells. Sometimes there are some infiltrating leukocytes. This is synonymous with the syndrome of rapidly progressing glomerulonephritis. |
|
|
Describe the different patterns of proliferation of sclerosis
|
-Focal (<50% of glomeruli) vs Diffuse (>50% of glomeruli)
-Segmental (Part of the glomerulus) vs Global (The whole glomerulus) |
|
|
Describe the significance of red cell casts or deformed red cells in urine
|
Indicates glomerular disease
|
|
|
Describe urine in proteinemia
|
Bubbly
|
|
|
Describe urine in hematuria
|
Coca-cola, Tea colored
|
|
|
Describe the presentation of acute nephritic syndrome
|
-Decreased GFR
-Oliguria -Edema -Hypertension -Active urine sediment |
|
|
Describe Post-streptococcal glomerulonephritis/acute post infectious glomerulonephritis
|
-Usually follows pharyngitis but can also follow impetigo
-Involves the glomuli quite uniformly (diffuse) -Glomeruli are extremely hypercellular -Endocapillary proliferation present -Leukocytes infiltrate |
|
|
Describe how Post-streptococcal glomerulonephritis/acute post infectious glomerulonephritis leads to decreased GFR
|
All the leukocyte infiltrate reduced GFR. The more and more capillary loops that are occluded by cell proliferation the lower the creatinine clearance
|
|
|
What antigen is responsible for the humps in post-streptococcal glomerulunephritis?
|
Pyrogenic exotoxin B
|
|
|
Describe the disruption of the glomerular basement membrane from leukocytes
|
-As the leukocytes come in they release their proteases and ROS
-These can rupture the glomerular basement membrane -These ruptures allow RBCs to enter the urinary space -Certain proteins such as albumin solidify blocks of RBCs in the tubuls and lead to red cell cast formation |
|
|
Describe the outcomes of Post-streptococcal glomerulonephritis/acute post infectious glomerulonephritis
|
-In most patients the glomerular architecture is restored
-In some patients (<3%) the glomerular nephritis does not resolve in 6 weeks. If these patients excerise hard or develop a fever they can become symptomatic. This can eventually lead to renal failure -In some patients (<1%) the immune response is so exuberant that they develop endocapillary and extracapillary proliferaction (crescents). These have a rapidly progressive course leading to renal failure over a period of weeks |
|
|
Describe the etiology of post-streptococcal glomerulunephritis
|
-Follows infection with certain "nephritogenic" streptococcal strains (pharyngitic, dermal, etc)
-More common in children than adults -Time lag from infection to onset of GN (~2 weeks) -Nephritic picture common (oliguria, edema, hypertension, active urinary sediment, a rise in BUN and creatinine) -Low complement and C3 -Positive serologic tests for recept strep infection |
|
|
Describe the prognosis of post-streptococcal GN
|
-Excellent in children
-Good in adults |
|
|
In what diseases are there low levels of serum complement
|
-Acute post-infectious GN
-Lupus nephritis -Idiopathic MPGN -Cryoglobulinemic GN |
|
|
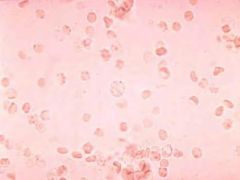
-Urinary sediment with normal RBCs
-Could come from anywhere - urethra, bladder, ureters, pelvis of the kidney -Can be from stones, tumor, stricture, or urinary infection |
|
|
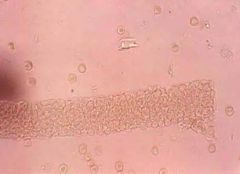
-Red cell casts
-Indicative of glomerulunephritis -Red cells are packed together in the shape of the tubule |
|
|
-Deformed red cells
-Indicative of glomerulonephritis -The red cells deform because they are passing through the medulla - a hypertonic and acidic environment |
|
|
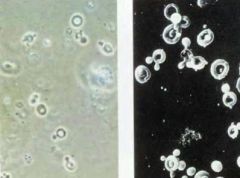
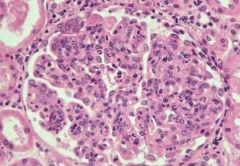
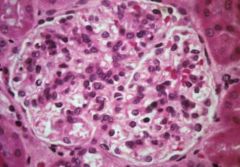
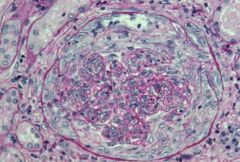
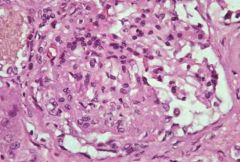
-Post streptococcal GN/acute post infectious GN
-Usually follows pharyngitis but can also follow impetigo -Involves glomeruli diffusely -Glomeruli are hypercellular |
|
|
-Post-streptococcal GN/acute post infectious GN
-Usually follows pharyngitis or impetigo -Endocapillary proliferation -Endothelial cells and mesangial cells proliferate within the confines of the glomerular basement membrane -Leukocyte infiltrate present due to release of C3a and C5a |
|
|
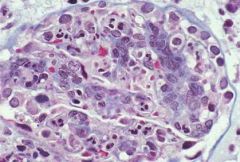
-Post streptococcal GN/Acute post infectious GN
-Cells are responding to deposits/immune complexes -Deposits are in red -Some are large enough to be seen on LM |
|
|
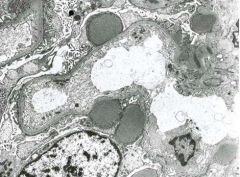
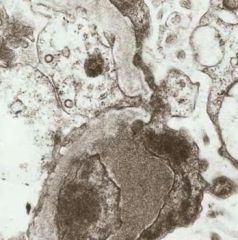
-EM of post streptococcal GN/acute postinfectious GN
-Classic hump shaped deposits of post infectious GN -They are large and sit on the outer aspect of the glomerular basement membrane |
|
|
-EM of post streptococcal GN/acute postinfectious GN
-Proteinuria occurs through here because the overlying foot processes are effaced -Different than membranous glomerulopathy because there are no intervening spikes and these deposits tend to be larger and fewer in number |
|
|
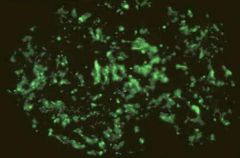
-Immunofluorescence of post streptococcal GN/acute postinfectious GN
-Granular pattern of IgG and C3 corresponding to the humps |
|
|
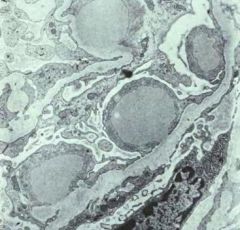
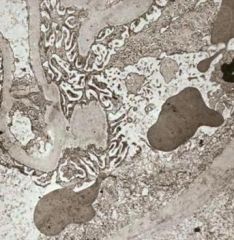
-EM of Post streptococcal GN/acute postinfectious GN
-Rupture of glomerular basement membrane from proteases and ROS from leukocytes |
|
|
-EM of Post streptococcal GN/acute postinfectious GN
-Ruptured glomerular basement membrane -Through these rupture sites RBCs can enter the urinary space where they normally couldnt |
|

|
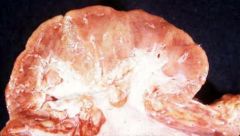
-Flea bitten kidney
-The red dots are all red cell casts -In acute nephritic syndrome the kidney is often swollen |
|
|
Describe the pathogenesis of post-streptococcal GN/acute postinfectious GN in the animal model
|
-Foreign antigen enters
-Over a period of days antigen-antibody complexes form -Once these reach a critical level complement activates -Production of a critical level of antigen-antibody complex leads to deposition of circulating immune complexes within the glomerular capillary walls leading to nephritis-Usually self limited and resolves when antigen is depleted -Response depends on immune response (too weak and not enough complexes, too strong and complexes are too big) |
|

|
-EM of Post streptococcal GN/acute postinfectious GN
-Shows the fate of humps over time -They become more electron lucent and begin to resolve |
|
|
-Restoration of glomerular capillary after post streptococcal GN
|
|
|
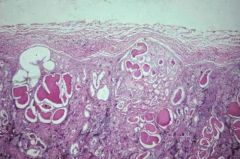
-Rare outcome of post streptococcal GN/acute postinfectious GN
-Immune response so exuberant that there is endocapillary and extracapillary (Crescent) proliferation -Can rapidly progress to renal failure in a matter of weeks |
|
|
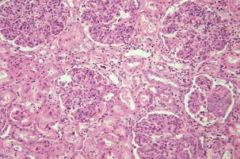
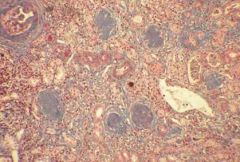
-Rare outcome of post streptococcal GN/acute postinfectious GN
-End stage renal failure in a patient that never recovered -We can see that the glomeruli have gone onto sclerosis. They have become acellular balls of matrix material. These are functionally dead glomeruli. -We have atrophy of the dependent portions of the nephron with tubular atrophy and interstitial fibrosis. |
|

|
-Kidney with chronic glomerulonephritis
-Kidney is contracted -Granular leather grain appearance |
|
|
-Kidney with chronic glomerulonephritis
-The granular appearance is because we have many glomeruli in the areas of depression that have gone onto sclerosis. -Those nephrons have undergone irreversible atrophy and obsolescence. -There are a few nephrons that are still filtering and these undergo a compensatory hypertrophy. You see these large tubules. |
|
|
-Chronic glomerulonephritis kidney cut in cross section
-The cortex is normally 1.2-1.5cm in thickness is not atrophies because so many of the nephrons have become scarred. |
|

|
1) Flea-bitten kidney
2) Lipoid nephrosis kidney 3) End stage kidney 4) Normal kidney |
|

|
-Heart valve in a patient with endocarditis
-Can lead to post infectious GN |
|
|
-Post infectious GN from endocarditis
-Glomerular proliferation is more segmental in distribution -Same pathogenesis |

