![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
453 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Hyperpigmentation, Hyponatremia, Hyperkalemia, lymphocytosis, eosinophilia, hypoglycemia.
|
Addison's Disease/Acute adrenal crisis
|
|
|
|
High levels of VLCFA, behavior problems emotional lability, visual and gait disturbances, adrenal insufficiency.
|
Adrenoleukodystrophy
|
|
|
|
Causes of adrenal insufficiency (12)
|
ketoconazole, suramin, metastatic tumor, fungal infection, adrenal hemorrhage, tuberculosis, adrenoleukodystrophy, Familial glucocorticoid deficiency, Addison's disease, HIV, CAH
|
|
|
|
Glucocorticoid Receptor Agonists
|
Cortisol, synthetic glucocorticoids, aldosterone
|
|
|
|
Glucocorticoid Receptor Antagonists/partial agonists
|
11-deoxycortisol, DOC, testosterone, and 17-beta-estradiol, MIFEPRISTONE (RU486)
|
|
|
|
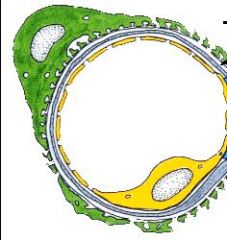
Hormones synthesized in the zona glomerulosa of the adrenal gland
|
Aldosterone. NOT cortisol or androgens (lacks 17-alpha-hydroxylase)
|
|
|
|
Hormones synthesized in the zona fasciculata of the adrenal gland
|
Cortisol and androgens. NOT aldosterone (lacks CYP11B2)
|
|
|
|
Hormones synthesized in the zona reticularis of the adrenal gland
|
Cortisol and androgens. NOT aldosterone. (lacks CYP11B2)
|
|
|
|
Androgen hormones
|
DHEA, DHEA sulfate, androstenedione
|
|
|
|
Mechanism of ACTH action on cells
|
Binds PM receptor - activates Gs - Adenylate cyclase - cAMP - pKA - phosphorylates cholesterol ester hydrolase
|
|
|
|
Rate-limiting step of cholesterol conversion to steroid hormones
|
Cholesterol - pregnenolone. Occurs in the mitochondria, and is increased by ACTH. Enzyme is cholesterol desmolase (CYP11A1). Through StAR.
|
|
|
|
Key enzyme in making Aldosterone
|
CYP11B2 (P450aldo/aldosterone synthase)
|
|
|
|
Symptoms of Glucocorticoid deficiency
|
weakness, fatigue, anorexia, nausea, vomiting, hypotension, hyponatremia, hypoglycemia, hyperpigmentation
|
|
|
|
Symptoms of Mineralcorticoid deficiency
|
Hyponatremia, hyperkalemia, dehydration, hypotension, acidosis, hyperpigmentation, weakness, fatigue. Lab: normocytic, normochromic anemia, neutropenia, eosinophilia, lymphocytosis, azotemia with increased BUN and serum creatinine.
|
|
|
|
Tumors causing ectopic ACTH syndrome
|
small cell lung carcinoma, pancreatic islet cell tumor, carcinoid tumor, medullary carcinoma of thyroid, pheochromocytoma
|
|
|
|
Clinical features of Cushing's syndrome
|
obesity, HTN, plethora, hirsutism, striae, acne, osteopenia, emotional lability, depression, amenorrhea, impotence, glucose intolerance, hyperlipidemia.
|
|
|
|
hypertension and hypokalemia
|
Adrenal Adenoma
|
|
|
|
Causes of secondary hypertension
|
OSA, aldosteronism, renal artery stenosis, renal parenchymal disease, Cushing's syndrome, coarctation of the aorta, high catecholamines, pheochromocytoma, estrogens, MAOI, erythropoietin, hyperparathyroidism, high growth hormone, hyper- or hypothyroidism, high salt intake, alcohol, obesity.
|
|
|
|
symptoms of hypokalemia
|
myalgia, muscle weakness, polyuria, dysrhythmia, rhabdomyolysis
|
|
|
|
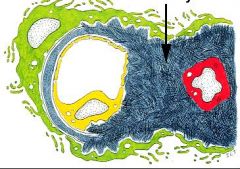
Path of circulation through the kidney
|
aorta - renal artery - segmental (lobar) artery - interlobar - arcuate - interlobular - afferent arteriole - glomerulus - efferent arteriole - peritubular cap and vasa recta - interlobular vein - arcuate vein - interlobar - segmental - renal ven - IVC
|
|
|
|
cell types of the anterior pituitary
|
acidophils (pale pink) = somatotropes, lactotropes.
basophils (deep pink) = corticotropes, thyrotropes, gonadotropes. Cromophobes (poor stain) = quiescent? |
|
|
|
Hormones released by the anterior pituitary
|
GH, FSH, LH, TSH, ACTH, PRL
|
|
|
|
Hormones released by the posterior pituitary
|
ADH, oxytocin
|
|
|
|
Cell type that produces calcitonin
|
parafollicular (clear) cells of the thyroid
|
|
|
|
2 cell types of the parathyroid
|
Chief cells (release PTH), and oxyphil cells
|
|
|
|
cell type derived from the ultimobranchial body of the 4th pharyngeal pouch
|
C cells of the thyroid
|
|
|
|
structures derived from the 3rd and 4th pharyngeal pouches
|
parathyroid glands
|
|
|
|
Structure derived from the 3rd pharyngeal pouch
|
thymus
|
|
|
|
structure derived from floor of pharynx between 1st and 2nd pharyngeal arches
|
thyroid
|
|
|
|
Muscles and nerves derived from 1st pharyngeal arch (mandibular)
|
CN V, muscles of mastication, mylohyoid, ant. belly of digastric, tensor typmpani, tensor veli palatini
|
|
|
|
Muscles and nerves derived from 2nd pharyngeal arch (hyoid)
|
CN VII, muscles of facial expression, stapedius, stylohyoid, post. belly of digastric
|
|
|
|
Muscles and nerves derived from the 3rd pharyngeal arch
|
CN IX, stylopharyngeus
|
|
|
|
Muscles and nerves derived from the 4th and 6th pharyngeal arch
|
CN X, cricothyroid, levator veli palatini, constrictors of pharynx, intrinsic muscles of larynx, striated muscles of esophagus
|
|
|
|
Hormones released from the adrenal medulla
|
epinephrine and NE
|
|
|
|
Hormones released from the zona glomerulosa of the adrenal cortex
|
mineralocorticoids (aldosterone)
|
|
|
|
Hormones released from the zona fasciculata of the adrenal cortex
|
Glucocorticoids (cortisol)
|
|
|
|
Hormones released from the zona reticularis of the adrenal cortex
|
Androgens (testosterone)
|
|
|
|
Hormone released by the pineal gland
|
melatonin (released by chief cells of pineal)
|
|
|
|
Venous drainage of adrenal glands
|
Right adrenal: directly to vena cava.
Left adrenal: Branch to Left Renal Vein. |
|
|
|
Enzyme deficient in Congenital Adrenal Hyperplasia
|
21-Hydroxylase Deficiency
|
|
|
|
Forms of adrenal insufficiency
|
1) primary - Addison's Dz
2) secondary - pituitary tumor 3) tertiary - exogenous glucocorticoids |
|
|
|
Symptoms of primary adrenal insufficiency (Addison's Dz)
|
fatigue, NVD, hypotension, hyponatremia, hyperkalemia, acidosis, hypoglycemia, azotemia, hypercalcemia, hyperpigmentation, salt craving, sexual dysfunction, menstrual abnormalities, arthralgia, myalgia
|
|
|
|
features of secondary or tertiary adrenal insufficiency
|
mineralcorticoid activity intact (renin-AgII), no hyperpigmentation.
Test with metyrapone or insulin tolerance test |
|
|
|
Test for primary adrenal insufficiency
|
cosyntropin stimulation
|
|
|
|
Test for secondary adrenal insufficiency
|
Metyrapone test
|
|
|
|
2 things required for diagnosis of Cushing's Syndrome
|
1) Clinical stigmata of hypercortisolism.
2) Biochemical hypercortisolism. |
|
|
|
Sreening tests for Cushing's syndrome
|
overnight low dose dexamethasone suppresion test, 24-hour urine free cortisol, midnight serum or salivary cortisol levels
|
|
|
|
Test to distinguish pituitary tumor vs. ectopic source of ACTH
|
petrosal sinus levels of ACTH
|
|
|
|
symptoms of pheochromocytoma
|
hypertension, tachycardia, palpitations, pallor, sweating, headaches, orthostatic hypotension, constipation, flushing, nervousness, tremor, weight loss.
|
|
|
|
Primary Hyperaldosteronism
|
hypertension, hypokalemia, metabolic alkalosis, feedback through RAS, inappropriate kaluresis, sensitive to salt intake, volume, posture, serum potassium
|
|
|
|
Substance used to measure total body water
|
tritium or deuterium
|
|
|
|
Substance used to measure extracellular water
|
inulin or mannitol
|
|
|
|
Measurement of intracellular water
|
calculated from TBW - ECW
|
|
|
|
Substance used to measure plasma water
|
Evan's blue or radioactive albumin
|
|
|
|
Measurement of interstitial water
|
Calculated from ECW - Plasma water
|
|
|
|
Hyperosmotic volume expansion
|
More salt than water is ingested. ECF volume increases. Osmolality increases.
|
|
|
|
Isoosmotic volume expansion
|
Intake of isoosmotic solution. Increases ECF volume. Osmolality remains the same.
|
|
|
|
Hypoosmotic volume expansion
|
Intake of pure water. Increased volume of both ICF and ECF, decreased osmolality.
|
|
|
|
Estimate of plasma osmolality
|
2 x Plasma Na+ concentration
|
|
|
|
Calculation of plasma osmolality
|
2 x P[Na+] + [glucose]/18 + BUN/3
|
|
|
|
Effect of renal sympathetic nerve activation (by fall in BP - sensed by baroreceptor)
|
Decreased Na+ excretion, Increased ECFV
|
|
|
|
Effect of activation of RAS (by fall in BP - sensed by baroreceptor)
|
Decreased Na+ excretion, Increased ECFV
|
|
|
|
Effect of activating ADH (sensed by osmoreceptor)
|
Decreased water excretion, decreased plasma osmolality, increased TBW.
|
|
|
|
Effect of activating atrial natriuretic peptide (atrial stretch - sensed by increased ECW)
|
Increased Na+ excretion, decreased ECFV
|
|
|
|
Control of renin release from juxtaglomerular cells (3 ways)
|
1) decreased NaCl sensed by macula densa.
2) Increased cAMP by activation of beta1-adrenoceptors or PGE2/PGI2 3) Increased Intracellular Ca2+ (stretch of arteriolar cells)inhibits renin secretion |
|
|
|
Actions of angiotensin II
|
increases sodium and water retention, constricts glomerular arterioles, constricts systemic arteries and increases BP, augments NE release/sympathetic activity, stimulates thirst in hypothalamus, simulates ADH (hypothalamus), stimulates zona glomerulosa release of aldosterone.
|
|
|
|
Action of aldosterone
|
Na+ resorption in distal tubule (increase of Na+/K+ ATPase and increase of luminal Na+ permeability)
|
|
|
|
Action of ADH
|
1) Causes water resorption in the collecting duct
2) increases urea resorption in the collecting duct |
|
|
|
Action of endothelin
|
Acts on ETA and ETB receptors to constrict cortical arteries and inhibit Na+ resorption in the distal tubule, dilate medullary arterioles
|
|
|
|
Vasodilator prostaglandins
|
PGI2 and PGE2. (under normal conditions, don't alter renal blood flow, but with Na+ or volume depletion, they maintain.)
|
|
|
|
Effect of NO on renal blood flow
|
Activates soluble guanylyl cyclase to relax vascular smooth muscle cells - Inhibits Na+ reabsorption in distal tubule.
|
|
|
|
Effects of ANP
|
1) Dilates AFFERENT arteriole to increase GFR.
2) Decrease Na+ reabsorption through amiloride-sensitive Na+ channels (thru cGMP). 3) Inhibits secretion of aldosterone, AngII and renin. 4) results in natriuresis and diuresis. |
|
|
|
2 areas of great pressure drop in renal vasculature
|
afferent and efferent arteriole - regulation of BF
|
|
|
|
Cells that secrete renin
|
Juxtaglomerular cells
|
|
|
|
Features of peritubular capillary beds
|
Fenestrated, low hydrostatic pressure, high oncotic pressure - all facilitate reabsorption.
|
|
|
|
Control mechanisms of renal blood flow
|
myogenic tone (stretch stimulates contraction - buffers changes in systemic pressure), tubuloglomerular feedback (macula densa senses decreased NaCl and causes renin release and decreases afferent arteriolar resistance), sympathetic tone, RAS, other hormones
|
|
|
|
Factors that increase sensitivity of tubuloglomerular feedback
|
Volume contraction, adenosine, PGE2, Thromboxane, HETE, Angiotensin II
|
|
|
|
Factors that decrease sensitivity of tubuloglomerular feedback
|
Volume Expansion, ANP, NO, cAMP, PGI2, high protein diet
|
|
|
|
Effect of sympathetic nervous system on renal vasculature
|
1) VSMC have alpha receptors - constrict, decrease RBF (thru Gq, PLC)
2) juxtaglomerular cells have beta-1 receptors - release renin (thru Gs, AC, cAMP) |
|
|
|
Regulators of renin secretion
|
1) decreased NaCl at macula densa increases renin.
2) sympathetic stimulation increases renin. 3) Decreased stretch or shear increases renin. 4) increased intracellular Ca2+ INHIBITS renin release. |
|
|
|
Effects of Angiotensin II (5)
|
Constricts afferent and efferent arterioles, promotes Na+ and water resorption, constricts systemic vasculature, increases NE release, stimulates thirst and ADH in hypothalamus, stimulates aldosterone release.
|
|
|
|
Effects of aldosterone (2)
|
increases Na+/K+ ATPase activity in basolateral membrane of distal tubule, increases luminal Na+ and K+ permeability. (Na+ and water resorption)
|
|
|
|
Effects of ADH (2)
|
stimulates water resorption in collecting duct, increases urea reabsorption in collecting duct.
|
|
|
|
Effect of ET-1 on ET-A receptors
|
constrict cortical arteries and mesangial cells (increase blood pressure)
|
|
|
|
Effect of ET-1 on ET-B receptors
|
Inhibit Na+ reabsorption in the distal tubule and cause vasodilation of medullary arterioles (decrease blood pressure).
|
|
|
|
Why should Cox inhibitors be avoided during dehydration or stresses like surgery?
|
Under these conditions, PGE2 and PGI2 cause vasodilation and prevent too much vasoconstriction of afferent arteriole - maintain renal blood floow. If blocked, could cause acute renal failure.
|
|
|
|
Renal effects of blocking NO production
|
sodium retention, hypertension, block sensitivity of TGF
|
|
|
|
What is the filtration fraction?
|
The amount of plasma that is filtered in the glomerulus - about 20%
|
|
|
|
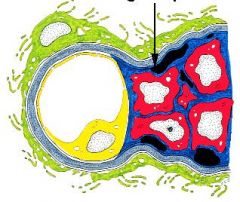
3 layers of filtration barrier
|
1) fenestrated endothelium
2) Basement membrane 3) Epithelium (podocytes with filtration slits) All these surfaces have highly negatively charged glycoproteins |
|
|
|
Layers of glomerular basement membrane
|
lamina rara interna, lamina densa, lamina rara externa
|
|
|
|
Cutoff size for things passing through glomerulus
|
70,000 kDa - but charge matters:
Albumin is 65,000, but has over 200 neg. charges, so will not be filtered |
|
|
|
Amount of filtrate reabsorbed
|
99% under normal conditions
|
|
|
|
Regulation of GFR
|
hydrostatic pressure in glomerulus and Bowman's capsule, oncotic pressure in glomerular capillary, Oncotic pressure in Bowman's space (O)
|
|
|
|
Starling equation
|
GFR = Kf * [(Pgc - Pbs) - pgc]
|
|
|
|
Features of Kf (filtration coefficient)
|
Index of health of filtration barrier, Normally 12.5 mL/min*mmHg, change in Kf chronically alters GFR, hormones and disease can alter Kf (DM), Kf acutely modified by contraction of mesangial cells
|
|
|
|
Normal values of Starling forces
|
1) Pgc = 45 mmHg
2) Pbs = 10 mmHg 3) pgc = 19 mmHg 4) Net filtration = 45 - 10 - 19 = 16 mmHg |
|
|
|
Effect of constriction of afferent arteriole
|
Decrease in RPF and GFR
|
|
|
|
Effect of dilation of afferent arteriole
|
Increases Pgc and GFR
|
|
|
|
Effect of constriction of efferent arteriole
|
Decreases RPF and Increases GFR, Pgc
|
|
|
|
Effect of dilation of efferent arteriole
|
Decreases Pgc and GFR
|
|
|
|
Effect of constriction of both efferent and afferent arterioles
|
Dereased flow - increases oncotic pressure - decreases GFR
|
|
|
|
Effect of increased protein concentration on GFR
|
decreases GFR
|
|
|
|
Effect of decreased protein concentration on GFR
|
increases GFR
|
|
|
|
Equation relating GFR and clearance of marker
|
GFR = uv/p
u = urine [marker] (mg/dL) v = urinary flow rate (mL/min) p = plasma [marker] (mg/dL) |
|
|
|
Reference values for urinary creatinine clearance
|
males: 94 - 110 mL/min
females: 72 - 110 mL/min |
|
|
|
Normal BUN/creatinine ratio
|
12-20:1
|
|
|
|
Factors affecting GFR
|
Renal Dz, DM, HTN, urinary tract obstruction, decreased RBF or increased plasma protein, decreased angiotensin II, increased sympathetic activity or vasoconstrictor autocoids, pregnancy
|
|
|
|
equation for amount of substance reabsorbed
|
[X] reabsorbed = GFR * [Px] -([Ux] * V)
|
|
|
|
5 important substances that are >99% reabsorbed by kideny
|
Water, sodium, bicarb, chloride, glucose
|
|
|
|
Part of nephron where glucose is actively reabsorbed
|
Glucose is actively cotransported with Na+ by a saturable mechanism in the PCT
|
|
|
|
Filtered Load
|
GFR * plasma [X]
|
|
|
|
Transport max for glucose
|
375 - 400 mg/min
(plasma threshold ~180 - 220 mg/dL) |
|
|
|
Substances that competitively inhibit glucose reabsorption
|
sulfates, amino acids, uric acid, organic acids
|
|
|
|
Part of nephron where urea is passively reabsorbed
|
PCT - no transport maximum for urea. Slower flow = more urea reabsorption.
|
|
|
|
Part of nephron where urea reabsorption is dependent on ADH
|
DCT - ADH increases premeability of DCT and water comes in, bringing urea with it
|
|
|
|
Substance used to estimate RPF
|
PAH (para-aminohippuric acid)
PAH is actively secreted by PT cells. |
|
|
|
Substances reabsorbed in the early proximal convoluted tubule
|
Na+, Glucose, amino acids, HCO3-, water
|
|
|
|
Substances reabsorbed in late proximal convoluted tubule
|
K+, Cl-, HCO3-, Ca2+, Mg2+, water
|
|
|
|
Substance secreted in proximal convoluted tubule
|
H+, organic acids
|
|
|
|
substances absorbed in thin descending loop of Henle
|
Water, salt, urea
|
|
|
|
Channel in Thick ascending loop of Henle responsible for countercurrent gradient
|
Na+/2Cl-/K+
|
|
|
|
Substances actively secreted in thick ascending loop of Henle
|
H+, K+
|
|
|
|
Channel in Early distal tubule
|
Thiazide sensitive Na+ and Cl- channel
|
|
|
|
Two cell types in the late distal convoluted tubule
|
Principal cell (hormone responsive - Na+, Cl- reabsorption, K+, Cl- secretion, H20 fm ADH), intercalated cell (acid-base balance)
|
|
|
|
Mechanism of Aldosterone increase of Na+ resorption in distal tubule, CCD, MCD
|
Increases transcription of Na+ channels, Na+/K+ ATPases in principal cells
|
|
|
|
Function of intercalated cells of the late distal tubule and collecting duct
|
Acid-base balance by K+/H+ ATPase, H+ pump, increase HCO3- with acidosis, No aquaporin
|
|
|
|
Site of regulation of aldosterone
|
Early distal tubule/collecting duct (increases reabsorption of NaCl, water, increase secretion of K+)
|
|
|
|
Site of regulation of angiotensin II
|
Proximal convoluted tubule (increases reabsorption of NaCl, water)
|
|
|
|
Site of regulation of ADH
|
Late DT, CCD/MCD (increase reabsorption of water and urea)
|
|
|
|
Site of regulation of ANP
|
Distal convoluted tubule/collecting duct (decrease NaCl reabsorption)
|
|
|
|
Site of regulation of PTH
|
Proximal convoluted tubule, TALH, Distal tubule (decrease PO4- and increase Ca2+ reabsorption)
|
|
|
|
Titratable acids (urinary buffers for secreting H+)
|
PO4-, creatinine, sulfates
|
|
|
|
substance secreted in proximal tubule in times of acidosis
|
NH4+ (forms NH3 - bicarb is formed, NH4+ is recycled in medulla - diffuses into collecting duct, binds H+ and excreted as H2CO3)
|
|
|
|
Mechanism of ADH action
|
ADH binds to V2 receptors on principal cells in collecting duct - stimulates AC - cAMP - pKA - phophorylates proteins in vesicles containing aquaporin - vesicles fuse to PM and create channels for H2O. Also: increases urea permeability, stimulates PGE2
|
|
|
|
Regulation of ADH secretion
|
1) Blood pressure (baroreceptors in aortic arch, carotid sinus, L atrium, pulmonary vessels - input to hypothalamus)
2) Plasma osmolality Osmoreceptors in hypothalamus sense when rises above a certain set point |
|
|
|
Equation for free water clearance
|
CH2O = V - (Uosm * V/Posm)
|
|
|
|
Nephrotic Syndrome
|
>3g/24 hr proteinuria, edema, hypoproteinemia, hyperlipidemia
|
|
|
|
Nephritic syndrome
|
hematuria, proteinuria, renal insufficiency, hypertension
|
|
|
|
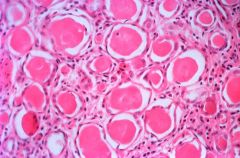
Minimal change glomerulopathy findings
|
Microvillous transformation, foot process fusion, No glomerular lesion. IF: no or slight immune deposition. Good prognosis, steroid responsive, childhood nephrotic syndrome.
|
|
|
|
Focal segmental glomerulosclerosis findings
|
Less than 50% of glomeruli have lesion, only part of glomerulus involved. Amorphous electron dense material and cellular debris, lipid laden cells, FSGS with hyalinosis, adhesions. IF: focal segmental IgM and C3, poss slight mesangial IgM and C3. Poor prognosis, not steroid responsive.
|
|
|
|
Membranous glomerulopathy findings
|
Most common cause of idiopathic nephrotic syndrome in adults. SUBEPITHELIAL deposits. Diffuse global capillary wall thickening, GBM irregularities. IF: diffuse global capillary wall granular staining for Ig and C.
|
|
|
|
Membranoproliferative glomerulonephritis findings
|
Mixed nephrotic/nephritic syndrome with hypocomplementemia.
|
|
|
|
MPGN type I findings
|
Type I: immune complex mediated, extensive subendothelial deposits and mesangial interposition. diffuse global hypercellularity with hypersegmentation, thickened cap walls, doubled GBM, varying number of PMN. IF: diffuse global capillary wall pseudolinear to granular Ig and C.
|
|
|
|
MPGN type II findings
|
Dense deposit disease. Dense transformation of GBM. Diffuse global hypercellularity with hypersegmentation and thickened cap walls. IF: pseudolinear cap wall and coarse granular mesangial C3.
|
|
|
|
Diabetic Glomerulosclerosis findings
|
Light: very thick GBM, mesangial matrix expansion - can produce Kimmelstiel-Wilson nodules. IF: linear staining of BM for IgG (ionic binding secondary to abnormal glycosylation)
|
|
|
|
Amyloidosis findings
|
Light: pale acidophilic amorphous material (birefringent with Congo Red) effacing portions of glomeruli, vessels, interstitium. IF: specific staining for amyloid AA or AL protein.
|
|
|
|
Electron dense immune complex deposits in mesangium
|
IgA nephropathy
|
|
|
|
Electron dense subendothelial immune complex deposits
|
MPGN and class IV lupus GN
|
|
|
|
GBM thickening
|
diabetic glomerulosclerosis
|
|
|
|
GBM thinning
|
thin BM nephropathy
|
|
|
|
GBM replication
|
MPGN
|
|
|
|
collagenous matrix expansion
|
sclerosis and/or hyalinosis (FSGN, amyloidosis)
|
|
|
|
Thin basement membrane nephropathy findings
|
Familial dz. Benign hematuria. Glomeruli unremarkable by light. Electron micro: reduced thickness of lamina densa. No findings on IF.
|
|
|
|
IgA nephropathy findings
|
varied clinical presentation: asymptomatic hematuria to renal failure. Slowly progressive course. Range of histo: no change to focal/diffuse hypercellularity to chronic sclerosing GN. IF: diffuse global granular mesangial IgA and C.
|
|
|
|
Acute post-infectious GN findings
|
Immune complex deposition. 1-2 weeks post-strep. Light: diffuse enlargement, hypercellularity, neutrophil infiltration, subepithelial HUMPS. IF: Diffuse global coarse granular capillary wall for IgG and C3, and along the BM.
|
|
|
|
Lupus GN findings
|
Widely varied clinical presentation and pathology. Class I: mesangial IC - mild hematuria/proteinuria.
Class II: mesangial IC with hypercellularity - mild hematuria/proteinuria. Class III: Mesangial and subendothelial IC - Moderate nephritis. Class IV: Mesangial and Subendothelial IC - Severe Nephritis. Class V: Subepithelial, mesangial IC - Nephrotic syndrome. Class VI: variable - chronic renal failure. |
|
|
|
Crescentic glomerulonephritis (rapidly progressing GN) findings
|
Crescents in some or all glomeruli, tuft shows features of inflammation and/or necrosis. Usually caused by immune complex dz in children and ANCA dz in adults.
|
|
|
|
Anti-glomerular Basement Membrane antibody GN findings
|
linear glomerular basement membrane staining for IgG, serologic detection of circulating anti-GBM Ab, crescenting glomeruli. Rare, but aggressive. Ab to Type IV collagen.
|
|
|
|
ANCA GN findings
|
Glomerular necrosis, crescents, no Ig deposits. 75% have necrotizing systemic small vessel vasculitis.
|
|
|
|
Three diseases associated with ANCA Ab.
|
Wegener's granulomatosis (small vessel vasculitis, necrotizing granulomas - usu. respiratory, usu C-ANCA), Churg-Strauss Syndrome (eosinophilia and asthma - usu P-ANCA), Microscopic polyangiitis (small vessel vasculitis - usu P-ANCA).
|
|
|
|
Proteins targeted by ANCA
|
myloperoxidase (MPO-ANCA; perinuclear staining = P-ANCA) or proteinase 3 (PR3-ANCA; cytoplasmic staining = C-ANCA) usually in neutrophils and monocytes.
|
|
|
|
Henoch-Schonlein purpura
|
Most common childhood vasculitis. IgA immune complex deposition in vasculature. Involves skin, gut, glomeruli. Arthralgias, arthritis.
|
|
|
|
Cryoglobulinemic GN
|
Type I MPGN phenotype. Type I - IgM, Type II - rheumatoid IgM complex w/IgG, Type III - polyclonal. Most patients have hepatitis C.
|
|
|
|
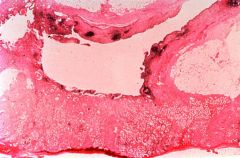
Hypertensive nephrosclerosis
|
Renal vascular and glomerular sclerosis caused by mild to moderate HTN. Hyaline arteriolosclerosis.
|
|
|
|
Malignant nephrosclerosis
|
Renal injury caused by malignant HTN. Thrombotic microangiopathy, fibrinoid necrosis of arterioles, GBM doubling, wrinkling, mesangial congestion.
|
|
|
|
Acute tubuar Necrosis
|
rapidly rising serum creatinine usu associated with oliguria. Swollen kidneys with pale cortex and congested medulla. Flattened epithelium in tubule and loop of henle, dilation of lumens, loss of brush border, necrosis.
|
|
|
|
Causes of acute tubular necrosis
|
Ischemia (hemorrhage, burns, dehydration, prolonged diarrhea, congestive heart failure), Nephrotoxins (aminoglycosides, amphoB, radiographic contrast, heavy metals, organic solvents, paraquat)
|
|
|
|
Pathology of drug induced (hypersensitivity) acute tubulointerstitial nephritis
|
patchy infiltration of cortex, and some medulla by lymphocytes and eosinophils. PCT and DCT have focal invasion. Glomeruli and vessels not invaded.
|
|
|
|
Drugs causing acute tubulointerstitial nephritis
|
NSAIDs, diuretics, beta-lactam antibiotics.
|
|
|
|
Cause of acute pyelonephritis
|
Gram-negative bacteria from feces (mostly e.coli) cause 80%.
|
|
|
|
Pathology seen in acute pyelonephritis.
|
kidneys have small white abscesses on subcapsular surfaces and cut surface. The epithelium of pelvis and calyces is hyperemic with purulent exudate.
|
|
|
|
Clinical symptoms of acute pyelonephritis
|
fever, chills, sweats, malaise, flank pain, costovertebral angle tenderness. Leukocytosis with neutrophilia, casts in urine.
|
|
|
|
Chronic pyelonephritis pathology
|
atrophy, scarring, contraction of papillary tip, thinning of cortex, deformed calyces, corticomedullary scarring.
|
|
|
|
Pathology of Light chain (multiple myeloma) cast nephropathy
|
numerous dense hyaline casts in distal tubules and collecting ducts - eosinophilic and glassy, often with fractures and angular borders.
|
|
|
|
Pathogenesis of light chain (multiple myeloma) cast nephropathy
|
circulating monoclonal light chains cross glomerular capillaries and precipitate, causing obstruction.
|
|
|
|
Pathology of drug induced (hypersensitivity) acute tubulointerstitial nephritis
|
patchy infiltration of cortex, and some medulla by lymphocytes and eosinophils. PCT and DCT have focal invasion. Glomeruli and vessels not invaded.
|
|
|
|
Drugs causing acute tubulointerstitial nephritis
|
NSAIDs, diuretics, beta-lactam antibiotics.
|
|
|
|
Cause of acute pyelonephritis
|
Gram-negative bacteria from feces (mostly e.coli) cause 80%.
|
|
|
|
Pathology seen in acute pyelonephritis.
|
kidneys have small white abscesses on subcapsular surfaces and cut serface. The epithelium of pelvis and calyces is hyperemic with purulent exudate.
|
|
|
|
Clinical symptoms of acute pyelonephritis
|
fever, chills, sweats, malaise, flank pain, costovertebral angle tenderness. Leukocytosis with neutrophilia, casts in urine.
|
|
|
|
Chronic pyelonephritis pathology
|
atrophy, scarring, contraction of papillary tip, thinning of cortex, deformed calyces, corticomedullary scarring.
|
|
|
|
Pathology of Light chain (multiple myeloma) cast nephropathy
|
numerous dense hyaline casts in distal tubules and collecting ducts - eosinophilic and glassy, often with fractures and angular borders.
|
|
|
|
Pathogenesis of light chain (multiple myeloma) cast nephropathy
|
circulating monoclonal light chains cross glomerular capillaries and precipitate, causing obstruction.
|
|
|
|
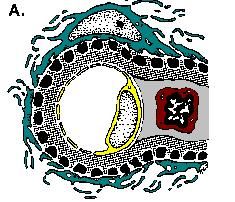
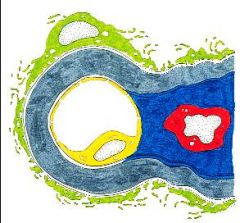
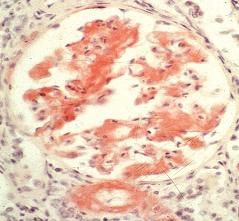
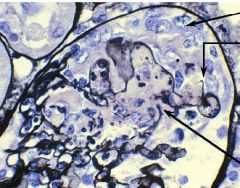
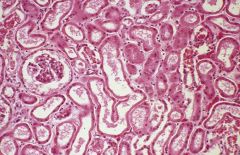
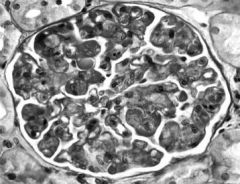
1) Acute post-infectious glomerulonephritis.
2) Subepithelial humps = dense deposits of immune complexes. Diffuse granular hypercellularity with numerous PMNs. 3) Diffuse and Global coarse Granular capillary wall IgG and C3. |
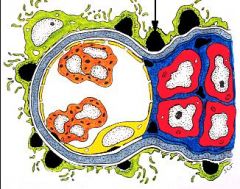
1) What disease is depicted?
2) Describe the pathology. 3) What would you expect to see on IF? |
Children with recent strep infections.
|
|
|
1) Acute post-infectious GN
2) hypocomplementemia, hematuria, proteinuria, decreased GFR, oliguria, salt and water retention, edema, HTN. |
1) What disease process is depicted?
2) what are clinical findings? |
Child with recent strep infection.
|
|
|
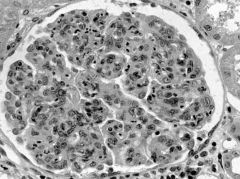
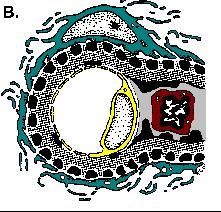
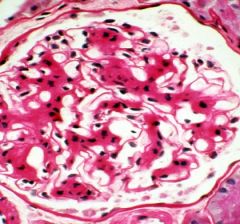
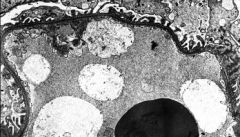
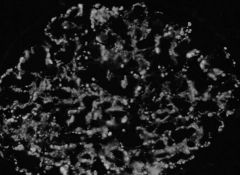
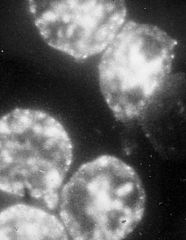
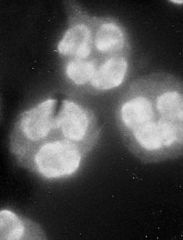
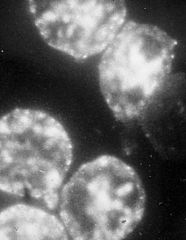
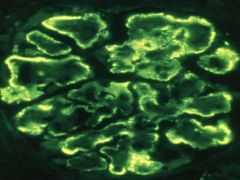
1) Minimal change glomerulopathy.
2) microvillous transformation and foot process fusion. 3) Common cause of childhood nephrotic syndrome: good prognosis, steroid responsive. 4) no or only slight immune deposition. |
1) What disease is depicted?
2) Describe the pathology. 3) what is the prognosis? 4) What would you expect to see on IF? |
|
|
|
1) minimal change glomerulopathy.
2) theory suggests a role for a T-lymphocyte derived factor. |
1) what disease is depicted?
2) what is the pathogenesis? |
|
|
|
1) FSGS
2) amorphous electron dense cellular debris, lipid laden cells. 3) poor prognosis; non-steroid responsive. |
1) What disease is depicted?2) Describe the pathology.
3) What is the prognosis? |
|
|
|
1) Minimal change glomerulopathy.
2) Hodgkin's dz, NHL, allergy, lithium, NSAIDs, AIDS, diabetes, congenital. 3)significant proteinuria and pitting edema, periorbital edema. |
1) What disease is depicted?
2) What are secondary causes? 3) What are clinical findings? |
|
|
|
1) Minimal change glomerulopathy.
2) Hodgkin's dz, NHL, allergy, lithium, NSAIDs, AIDS, diabetes, congenital. 3)significant proteinuria and pitting edema, periorbital edema. |
1) What disease is depicted?
2) What are secondary causes? 3) What are clinical findings? |
|
|
|
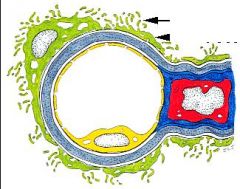
1) Membranous glomerulopathy.
2) Subepithelial deposits, diffuse global capillary wall thickening with GBM spikes. 3) Diffuse global capillary wall granular staining for Ig and C |
1) What disease is depicted?
2) Describe the pathology. 3) What would you see on IF? |
|
|
|
1) primary membranous glomerulopathy.
2) idiopathic - most likely secondary to in situ Ab-Ag immune complex formation. |
1) What disease is depicted?
2) What is the etiology? |
|
|
|
1) Secondary membranous glomerulopathy.
2) autoimmune dz (lupus), drug exposure (gold), infection (HepB), malignancy, renal vein thrombosis. 3) subepithelia deposits AND mesangial and small subendothelial dense deposits. |
1) What disease is depicted?
2) What is the etiology? 3) Describe the pathology. |
|
|
|
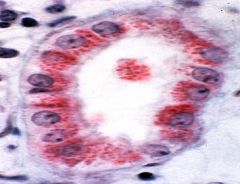
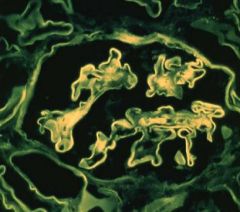
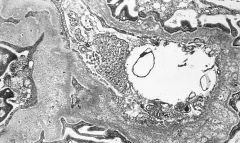
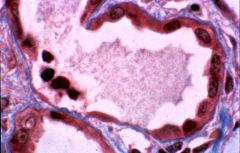
1) MPGN type I
2) Subendothelial deposits, circumferential mesangial interposition, diffuse hypercellularity, thickened capillary walls, doubled GBMs and PMNs. 3) Immune complex mediated - infection (Hep C), cryoglobulinemia. 4) Diffuse global capillary wall pseudolinear to granular Ig and C. 5) mixed nephrosis/nephritis, hematuria, hypocomplementemia. |
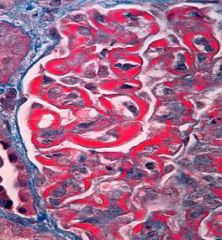
1) What disease is depicted?
2) Describe the pathology. 3) What is the etiology? 4) What would you see on IF? 5) What would you see clinically? |
|
|
|
1) MPGN Type I
2) subendothelial deposits, mesangial interposition. 3)diffuse global capillary wall pseudolinear to granular Ig and C. |
1) What disease is depicted?
2) What would you see on EM? 3) Describe the IF. |
|
|
|
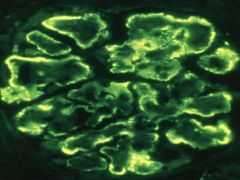
1) MPGN Type II (dense deposit disease)
2) hypocomplementemia 3) renal transplants |

1) What disease is depicted?
2) What characteristic lab result is expected? 3) Has a high recurrence with ______ |
|
|
|
1) Diabetic glomerulosclerosis.
2) Kimmelsteil-Wilson nodules 3) linear staining of GBM for IgG |
1) What disease is depicted?
2) What is a characteristic light microscopy finding? 3) What would you see on IF? |
|
|
|
1) Diabetic Glomerulosclerosis.
2) Increased abnormal glycosylation of IgG. 3) ESRD. |
1) What disease is depicted?
2) What is the pathogenesis? 3) This is the most common cause of ______ in the US. |
|
|
|
1) Diabetic glomerulosclerosis.
2) Linear staining of BM for IgG - IgG binds to collagen secondary to abnormal glycosylation. |
1) What disease is depicted?
2) Describe the IF. |
|
|
|
1) Diabetic glomerulosclerosis.
2) Kimmelsteil-Wilson nodules. |
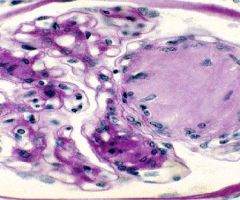
1) What disease is depicted?
2) What is the characteristic finding shown? |
|
|
|
1) Amyloidosis.
2) Specific staining for amyloid AA or AL. 3) plasma cell dyscrasia, neoplastic, or chronic inflammatory conditions. |
1) What disease is depicted?
2) What would you see on IF? 3) What is it associated with? |
|
|
|
1) Amyloidosis.
2) Specific stain for amyloid (AA or AL). 3) fluffy, pale pink "cotton candy" appearance throughout mesangium, can also involve vessels and interstitium. |
1) What disease is depicted?
2) What would you see on IF? 3) Describe the pathology. |
|
|
|
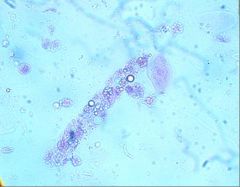
1) Hematuria (red blood cell casts in urine - active urine sediment)
2) Nephritic syndrome: hematuria, proteinuria, decreased GFR, increased BUN, creatinine, oliguria, salt and water retention, edema, HTN. |
1) What disease process is depicted?
2) In what syndrome will this be seen, and what are the clinical characteristics. |
|
|
|
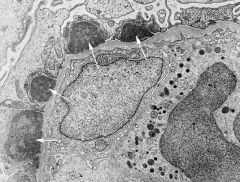
1) Thin Basement Membrane dz. (benign familial hematuria)
2) asymptomatic hematuria - do not develop renal failure, usually don't have proteinuria. 3) Nothing on IF. |
1) What disease is depicted?
2) What is the clinical presentation? 3) What would you see on IF? |
|
|
|
1) Thin basement membrane glomerulopathy (benign familial hematuria)
2) reduced thickness of lamina densa, normal podocytes, everything else normal. |
1) What disease is depicted?
2) Describe the pathology. |
|
|
|
1) Alport's Syndrome.
2) Genetic (mostly X-linked dom, could be AR, AD). Primary defect in Type IV collagen. 3) hematuria - may be assoc with proteinuria, HTN, chronic renal failure, bilateral sensorineural hearing loss, ocular changes in lens, retina, or cornea |
1) What disease is depicted?
2) What is the etiology? 3) What is the clinical presentation? |
|
|
|
1) Alport's Syndrome.
2) Foam cells in the interstitium of an inflamed kidney. |
1) What disease is depicted?
2) Describe the pathology. |
|
|
|
1) IgA nephropathy.
2) Antigen has not been determined - IgA immune complex deposition. Patients often have elevated blood levels of IgA. 3) Variable. Focal segmental to diffuse global mesangial cell hyperplasia. |
1) What disease is depicted?
2) What is the pathogenesis? 3) Describe the pathology. |
|
|
|
1) Crescentic glomerulonephritis.
2) Children: immune complex diseases. Adults: ANCA. 3) RPGN |
1) Describe the histology.
2) What are the most frequent causes in children and adults? 3) what clinical syndrome is often produced? |
|
|
|
1)Acute post-infectious GN.
2)Capillary wall deposition of immune complexes - punctate "christmas tree light" pattern. 3) hypercellular, can't see open capillary loops, neutrophilic infiltration. On EM: large subepithelial humps. |
1) What disease is depicted?
2) Describe the IF. 3) What is seen on light microscopy and EM? |
|
|
|
1) Acute post-infectious GN.
2) subepithelial humps, may be a few mesangial immune deposits. |
1) What disease is depicted?
2) Describe the characteristic feature. |
|
|
|
1) Lupus nephritis.
2) "full-house" staining, IgG usually dominant, C1q present. Everything stains. |
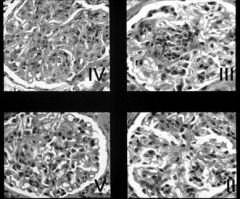
1) What disease is depicted?
2) What would you see on IF? |
|
|
|
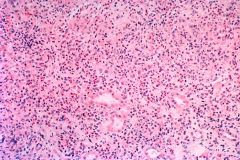
1) Acute Tubular necrosis.
2) dirty brown granular casts 3) dehydration, CHF, burns, shock, hemorrhage. |
1) What is the disease process depicted?
2) What would you see in the urine? 3) What are some causes? |
|
|
|
1) Acute Tubular Necrosis.
2) Yes - this is reversible. 3) Increased serum Creatinine, oliguria, increased BUN. |
1) What is the disease process depicted?
2) Is this reversible? 3) What would you expect to see for each of the following: Serum creatinine, urine output, BUN? |
|
|
|
1) Acute tubular necrosis.
2) ischemic and nephrotoxic. |
1) What is the disease process depicted?
2) what are the two types? |
|
|
|
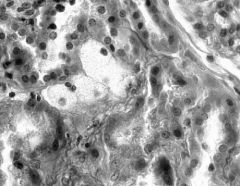
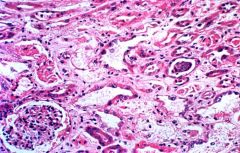
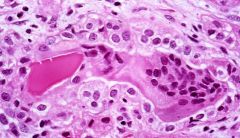
1) Acute tubulointerstitial nephritis.
2) Type IV cell-mediated response to drug - lymphocytic and eosinophilic infiltrate. 3) Ibuprofen, Naproxen, Thiazide diuretics, ACE inhibitors, penicillins, beta-lactams, sulfa drugs. |
1) What is the disease process depicted?
2) What is the pathogenesis? 3) What drugs are implicated? |
|
|
|
1) Acute tubulointerstitial nephritis.
2) eosinophils (also lymphocytes). 3) WBC casts in urine. |
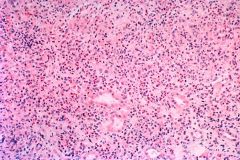
1) What is the disease process depicted?
2) What cell type is prominent in the infiltrate? 3) What might be seen in the urine? |
|
|
|
1) acute tubulointerstitial nephritis.
2) Normal glomeruli, interstitium filled with a sea of lymphocytes and eos. Tubules effaced. |
1) What is the disease process depicted?
2) Describe the pathology. |
|
|
|
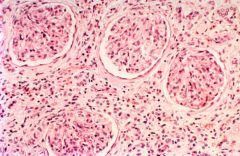
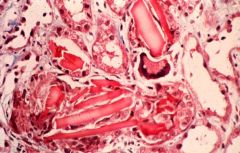
1) Acute pyelonephritis.
2) Tubules containing WBC casts - neutrophils and lymphocytes. 3) Fever, chills, sweats, malaise, flank pain, CVA tenderness, leukocytosis, WBC casts in urine. |
1) What is the disease process depicted?
2) Describe the pathology. 3) What is the clinical picture? |
|
|
|
1) Chronic pyelonephritis.
2) recurrent bacterial infection with urinary tract obstruction, urine reflux, or both. 3) atrophy, scarring, thinning of cortex, calyectasis. |

1) What is the disease process depicted?
2) What is the pathogenesis? 3) Describe the pathology. |
|
|
|
1) Chronic pyelonephritis.
2) Calyectasis, cortical thinning. 3) Thyroidization - atrophic tubules. |
1) What is the disease process depicted?
2) What are two features shown in the histology? 3) What is commonly seen on higher power? |
|
|
|
1) Chronic pyelonephritis.
2) "Thyroidization" - atrophic tubules. 3) urinary tract obstruction or urine reflux - chronic bacterial infection. |
1) What is the disease process depicted?
2) Describe the pathology. 3) What is the pathogenesis? |
|
|
|
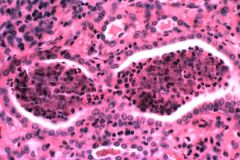
1) Light chain (myeloma) cast nephropathy.
2) Monoclonal light chains cross into tubules, mix with urinary proteins, and obstruct tubules. 3) Pink mass of obstructing light chains, with multinucleate giant cell attempting to engulf. |
1) What is the disease process depicted?
2) What is the pathogenesis? 3) Describe the pathology. |
|
|
|
1) Light chain nephropathy.
2) fractured casts of light chains/proteins with multinucleate giant cell. 3) Multiple myeloma. |
1) What is the disease process depicted?
2) Describe the pathology. 3) In what disease would this be seen? |
|
|
|
1) Where is renal K+ regulated?
2) What are the channels utilized? |
1) The principal cell of the cortical collecting duct.
2) ROMK - usually open, responds to incoming Na+. MaxiK - Not as often open, but opens with increased urine flow. |
|
|
|
What are some causes of hypokalemia?
|
Metabolic acidosis, increased beta-adrenergic, vomiting, diarrhea, loop and thiazide diuretics, primary mineralocorticoid excess, secondary hyperaldosteronism due to renal artery stenosis, renal tubular acidosis, insulin.
|
|
|
|
What are some causes of hyperkalemia?
|
metabolic acidosis, hyperglycemia, beta-blockade, tissue breakdown, exercise, reduced GFR, volume depletion, hypoaldosteronism, K+ sparing diuretics, adrenal insufficiency.
|
|
|
|
1) C-ANCA.
2) MPO-ANCA (C-ANCA) this is cytoplasmic staining of neutrophils. |
1) What is the disease process depicted?
2) What protein is involved? |
|
|
|
1) P-ANCA
2) MPO-ANCA (P-ANCA) This is perinuclear staining of neutrophils. |
1) What is the disease process depicted?
2) What is the protein involved? |
|
|
|
1) ANCA stained neutrophils.
2) Microscopic polyangiitis, Wegener's granulomatosis, Churg-Strauss syndrome. |
1) What is the disease process depicted?
2) What are three systemic diseases associated with this type of dz process? |
|
|
|
1) What is the site of action of Carbonic anhydrase inhibitor diuretics?
2) Name an example. 3) How do they work? 4) When are they used? 5) Side effects? |
1) PCT
2) Acetazolamide 3) Blocks breakdown of H2CO3 to H+ and HCO3-, decreases Na+ reabsorption thru Na+/H+ exchange, causes K+ loss. 4) open angle glaucoma, mountain sickness. 5) Creates a mild metabolic acidosis - good for mountain sickness - stim resp. |
|
|
|
1) Where is the site of action of Osmotic diuretics?
2) Name an example. 3) How do they work? 4) When are they used? 5) Side effects? |
1) PCT and descending limb Loop of Henle.
2) Mannitol. 3) Freely filtered, but not reabsorbed by tubules - inhibits water and solute reabsorption by increasing osmolarity of tubular fluid. 4) Cerebral edema. 5) hypernatremic dehdration if water not replaced. |
|
|
|
1) What is the site of action of Loop diuretics?
2) Name an example. 3) How do they work? 4) When are they used? 5) Side effects? |
1) Thick ascending loop of Henle.
2) Furosemide, Bumetanide. 3) Blockage of Na+/K+/2Cl- transporter. Blocks sodium reabsorption and increases K+, Ca2+, Mg2+ and H+ excretion. 4) Edema from congestive heart failure, cirrhosis, nephrotic syndrome, hypercalcemia. 5) hypomagnesemia, metabolic alkalosis. |
|
|
|
1) What is the site of action of Thiazide diuretics?
2) Name an example. 3) How do they work? 4) When are they used? 5) Side effects? |
1) Early DCT.
2) hydrochlorothiazide. 3) Blockage of thiazide-sensitive Na+/Cl- transporter. 4) Drug of choice for Tx of hypertension. Tx mild edematous conditions, diabetes insipidus. 5) hyponatremia, hypercalcemia, metabolic alkalosis, hyperglycemia, hyperlipidemia, hyperuricemia (gout). |
|
|
|
1) What is the site of action of Potassium Sparing diuretics?
2) Name three examples. 3) How do they work? 4) When are they used? 5) Side effects? |
1) Principal cells of late DCT, Collecting tubules.
2) Spironolactone, amiloride, triamterene. 3) Spironolactone blocks mineralocorticoid receptors (aldosterone), triamterene and amiloride block Na+/K+ exchange. 4) Combination with more proximal-acting diuretics to prevent K+ loss; Mild edema, Spironolactone can tx hirsutism in women. 5) gynecomastia (spironolactone) |
|
|
|
What enzymes are important in thyroid hormone synthesis?
|
peroxidase - adds I and couples DIT.
|
|
|
|
What is the mechanism of thyroid hormone action?
|
T4/T3 binds diffuses across PM, binds nuclear receptor, localized to nucleus and associates with another T3 or RXR, binds to TRE and alters transcription rates.
|
|
|
|
How is thyroid hormone release regulated?
|
Hypothalamus releases TRH - causes pituitary to release TSH - causes thyroid to release T4. T3 feeds back and inhibits release of TSH and TRH.
|
|
|
|
What lab findings would be expected in a patient with hyperthyroidism caused by a pituitary adenoma?
|
Very high TSH, high T4.
|
|
|
|
What lab findings would be expected in a patient with hyperthyroidism caused by overingestion of thyroxine?
|
Low TSH, High T3/T4, low thyroglobulin level.
|
|
|
|
What are Thianomides, and what are they used for?
|
propothiouracil (PTU) and Methimazole. These block synthesis of thyroid hormone. Useful in Graves, adenomatous dz, TSH secreting tumor.
|
|
|
|
What are lab findings in thyroid hormone resistance: generalized, at pituitary and at periphery?
|
Generalized: no clinical findings, increased TSH, T4.
Pituitary: hyperthyroid Sx, increased TSH, T4. Periphery: hypothyroid Sx, TSH and T4 normal. |
|
|
|
What is meant by euthyroid sick?
|
With acute and chronic illness, TSH is normal, but T4 and T3 are low. NO need to tx. Resolves with illness.
|
|
|
|
Symptoms of Craniopharyngioma?
|
Headache, visual field defects, pituitary deficiency, GH deficiency, diabetes insipidus.
|
|
|
|
What are the symptoms of a prolactin-secreting pituitary tumor?
|
amenorrhea, galactorrhea, erectile dysfunction. Can tx w/DA agonist.
|
|
|
|
What are symptoms of a non-secreting pituitary tumor?
|
visual field defects, headache, pituitary and GH deficiency. Tx w/surgery.
|
|
|
|
What are symptoms of a GH secreting pituitary tumor?
|
gigantism (child), acromegaly (adult), high IGF1. Tx w/surgery, somatostatin.
|
|
|
|
What are symptoms of an ACTH secreting pituitary tumor?
|
hypertension, hypokalemia, hypercortisolemia, Cushing's sx. Increased cortisol, ACTH. Tx w/surgery.
|
|
|
|
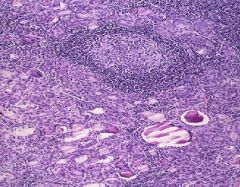
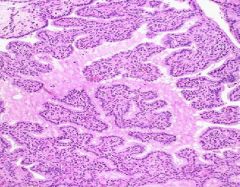
1) Hashimoto's thyroiditis.
2) autoimmune thyroid destruction. |
1) What disease is depicted?
2) What is the etiology? |
|
|
|
1) Graves' Disease.
2) Autoimmune disorder - thyroid stimulating immunoglobulin. |
1) What is the disease process depicted?
2) What is the etiology? |
|
|
|
Symptoms of hyperparathyroidism
|
osteoporosis (fractures), bone pain, abdominal pain, depression, memory loss, difficulty concentrating, nephrogenic diabetes insipidus. (Too much Ca2+, not enough K+)
|
|
|
|
What is Wermer's syndrome?
|
Multiple endocrine neoplasia type I. Autosomal dominant. MEN1 tumor suppressor gene mut. Multiple tumor types: hyperparathyroid, pancreatic, pituitary, carcinoid, adrenal, lipomas, angiofibromas, collagenomas.
|
|
|
|
What is the mutation in MEN IIa? What are common tumors?
|
Autosomal dominant mut in RET protooncogene. Thyroid, pheocromocytoma, hyperparathyroid tumors.
|
|
|
|
What is the mutation in MEN IIb? What are common tumors?
|
Autosomal dominant mut in RET protooncogene. 100% have medullary Thyroid CA and mucosal neuromas. Others: pheochromocytoma, marfanoid habitus.
|
|
|
|
Symptoms of adrenal adenoma?
|
High cortisol, low ACTH. Cushing's sx: glc intolerance, moon facies, buffalo hump, central obesity, striae.
|
|
|
|
Symptoms of Aldosterone-secreting adrenal carcinoma
|
Hypertension, hypokalemia, low renin, high aldosterone
|
|
|
|
Symptoms of pheochromocytoma
|
Hypertension, headache, sweating, tachycardia, palpitations, orthostatic hypotension, sense of "impending doom". High epinephrine, NE.
|
|
|
|
Cell type of tumor secreting PTH-rP, symptoms.
|
Squamous cell tumor; hypercalcemia, low PTH
|
|
|
|
Cell type of tumor secreting ADH, symptoms.
|
Small cell, bronchial tumors; hyponatremia, high ADH.
|
|
|
|
Cell type of tumor secreting ACTH, symptoms.
|
Small cell, squamous cell; hyperaldosteronism, severe hypertension and hypokalemia, high cortisol.
|
|
|
|
Describe the regulation of Prolactin.
|
PRL is under tonic inhibitory control by dopamine.
|
|
|
|
Describe the rhythm of secretion of ACTH and cortisol.
|
Diurnal rhythm with peak in the early morning.
|
|
|
|
Describe the rhythm of secretion of GH and LH.
|
ultradian rhythm with multiple peaks.
|
|
|
|
Describe the rhythm of secretion of TSH.
|
Quasi-diurnal, with peak in the early morning.
|
|
|
|
Describe the rhythm of secretion of testosterone.
|
multiple peaks during the day. Higher levels in the morning.
|
|
|
|
Describe the regulation of prolactin secretion.
|
Under tonic inhibitory control by Dopamine.
|
|
|
|
Name 6 hormones secreted by the anterior pituitary.
|
ACTH, GH, TSH, LH, FSH, PRL.
|
|
|
|
What are the determinants of ADH secretion?
|
Osmolality is the main determinant until blood volume is very low, then BP.
|
|
|
|
What are the actions of ADH?
|
Decreases medullary blood flow, increases H2O permeability in the DT and CD, increases Na+, Cl-, and K+ reabsorption, vasoconstriction, increased BP and SVR, decrease gluconeogenesis, increased ACTH.
|
|
|
|
What are the acidophilic cells in the anterior pituitary, and what hormones do they release?
|
1) Somatotroph - GH
2) Lactotroph - PRL 3) Somatomammotroph - GH, PRL |
|
|
|
What are the basophilic cells in the anterior pituitary, and what hormones do they release?
|
1) Corticotroph - ACTH, MSH, LPH, beta-endorphin.
2) Gonadotroph - LH, FSH, beta-hCG. 3) Thyrotroph - TSH |
|
|
|
What is Nelson's Syndrome?
|
hyperpigmentation caused by pituitary ACTH-secreting tumor.
|
|
|
|
What is the mechanism of GH?
|
Mediated through IGF-1, causes anabolic effects. Feedback inhibition occurs by IGF-1 stimulation of somatostatin.
|
|
|
|
How does TSH function?
|
Stimulates production of thyroid through cAMP generation.
|
|
|
|
How is LH regulated?
|
Inhibited by testosterone and estrogen in male, alternately inhibited and stimulated by estrogen in female.
|
|
|
|
What is Sheehan's syndrome?
|
Common cause of hypopituitarism in women, preceded by traumatic delivery. No breast milk, no periods.
|
|
|
|
Causes of hypopituitarism.
|
Pituitary adenoma, craniopharyngioma, Sheehan's syndrome, cerebral aneurysms, Tb, Fungus, Syphillis, Meningitis, amyloidosis, hemochromatosis, post-hypophysectomy, idiopathic.
|
|
|
|
Symptoms of pituitary insufficiency.
|
Lack of: ADH (polyuria, polydipsia), ACTH (hypotension, hypoglycemia), TSH (hypothyroid sx) LH/FSH (impotence, amenorrhea), PRL (no milk), GH (malaise, weakness).
|
|
|
|
What are the symptoms of acromegaly?
|
Joint pain, growth of tissues of extremities, face, glucose intolerance, organomegaly, hyperprolactinemia, mass effects, CVD.
|
|
|
|
What are the three types of cyroglobulinemia?
|
1) Type I: monoclonal IgM (seen in multiple myeloma, lymphoma).
2) Type II: monoclonal rhematoid factor iGM + polyclonal Ig. (often seen in Hepatitis C). 3) Type III: polyclonal immune complexes with no monoclonal. (seen in Lupus, chronic infection) |
|
|
|
What type of renal disease process is seen with cryoglobulinemia?
|
MPGN-I. hypercellular, hyaline thrombi, tram-tracking. Large subendothelial deposits.
|
|
|
|
MPGN Type II. Cryoglobulinemia. Monoclonal RF IgM with polyclonal Ig immune complex deposition.
|
A patient with Hepatitis C showed the following on renal biopsy. What is the disease? What is the pathogenesis?
|
|
|
|
MPGN Type I. Monoclonal IgM only staining peripheral capillary wall.
|
A patient with lymphoma had the following IF. What is the disease process? What is staining?
|
|
|
|
What types of vasculitis affect large vessels (the aorta)?
|
Giant cell arteritis, Takayasu arteritis.
|
|
|
|
Name 3 immune complex mediated vasculitides that affect small vessels.
|
1) Cryoglobulinemic
2) Henoch-Schonlein purpura 3) Lupus/rheumatoid |
|
|
|
Name 3 ANCA mediated vasculitides that affect small vessels.
|
1) Microscopic polyangiitis
2) Wegener's granulomatosis 3) Churg-Strauss syndrome |
|
|
|
Name 2 vasculitides that affect medium-sized vessels.
|
1) Polyarteritis Nodosa
2) Kawasaki dz (Fifth's) |
|
|
|
Describe the pathology seen in Microscopic polyangiitis.
|
Necrotizing and crescentic GN. ANCA mediated.
|
|
|
|
Describe the pathology of hypertensive nephrosclerosis.
|
Globally sclerotic glomerulus, scarring everywhere in nephron, thin, scarred cortex. Onion-skin vessels. Early: can see wrinkled capillary loops, intimal hyalinosis of vessels.
|
|
|
|
Name some causes of prerenal acute renal failure.
|
Hemorrhage, septic shock, low cardiac output.
|
|
|
|
Name some causes of intrarenal acute renal failure.
|
renal parencymal disease - GN, vasculitis, RPGN.
|
|
|
|
Name some causes of post-renal acute renal failure.
|
Urinary tract obstruction - stones, stricture, tumor.
|
|
|
|
3 drugs that decrease PCT secretion and falsely elevate creatinine
|
cimetidine, triamterene, trimethoprim
|
|
|
|
6 causes of prerenal (ischemic) acute renal failure in hospitalized pts
|
CHF, Sepsis, Volume depletion (diuretics), liver dysfunction, post obstructive diuresis. hypotension.
|
|
|
|
Causes of prerenal (ischemic) acute renal failure in outpatients. (7)
|
Vomiting, diarrhea, fever, poor oral intake, diuretics, CHF, debilitation.
|
|
|
|
Toxins causing intrarenal acute renal failure. (6)
|
Aminoglycosides, cyclosporin, radiocontrast, ACE-inhibitors, NSAIDS.
|
|
|
|
Nephrotoxic causes of acute renal failure.
|
Diabetic nephropathy, CHF, reduced renal function, concurrent disease, medications, electrolyte or acid-base abnormalities. Age>70.
|
|
|
|
4 causes of interstitial nephritis - Acute Renal Failure
|
Allergic reaction to drugs, autoimmune dz (lupus), infiltrative dz (sarcoidosis), infectious (legionnaire's)
|
|
|
|
Clinical features of tubulointerstitial nephritis (acute renal failure)
|
mild proteinuria, sterile pyuria, polyuria/nocturia, eosinophilia, fanconi-like syndrome (glycosuria, phosphaturia)
|
|
|
|
Causes of postrenal acute renal failure (5)
|
Prostatic hypertrophy, stones, medications (crystal formation, outlet obstruction), neoplastic, retroperitoneal disorder.
|
|
|
|
Drugs associated with post-renal acute renal failure
|
Sulfonamides, Methotrexate, Acyclovir, Triamterene, Ethylene glycol, protease inhibitor.
|
|
|
|
In which type of acute renal failure would Brown casts be seen, along with high urine sodium?
|
Intrarenal
|
|
|
|
In what type of acute renal failure would hyaline casts be seen?
|
Prerenal.
|
|
|
|
What should be suspected when dysmorphic red cells are seen in the urine?
|
Glomerulonephritis or vascular disease.
|
|
|
|
What should be suspected if monomorphic red cells are seen in the urine?
|
Bleeding from a post-glomerular site: foley catheter, bladder infection, interstitial nephritis, stone, renal cell carcinoma
|
|
|
|
Nephrotic syndrome. Urine sediment shows a fatty cast.
|
A patient with proteinuria has the following in his urine. What type of renal dysfunction is present?
|
|
|
|
hypertension, proteinuria and hematuria
|
Glomerulonephritis
|
|
|
|
Types of glomerular disease in acute renal failure
|
Rapidly progressive glomerulonephritis [systemic lupus erythematosus, small-vessel vasculitis (Wegener's granulomatosis or polyarteritis nodosa), Henoch-Schönlein purpura (immunoglobulin A nephropathy), Goodpasture's syndrome]
Acute proliferative glomerulonephritis: (endocarditis, poststreptococcal infection, postpneumococcal infection) |
|
|
|
Acute tubular necrosis
|
A patient with acute renal failure has the following urine sediment. The patient has been taking an aminoglycoside. What is the diagnosis?
|
|
|
|
High sodium chloride, without water.
|
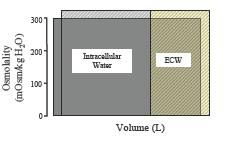
The diagram represents the fluid volume of a patient. What did the patient ingest?
|
|
|
|
SIADH
|
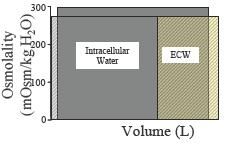
The diagram represents the fluid volume of a patient. what does the patient have?
|
|
|
|
Infusion of isotonic NaCl.
|
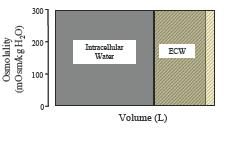
The diagram represents the fluid volume of a patient. What has been given to the patient?
|
|
|
|
What is the effect on GFR, RPF, and filtration fraction of constricting the afferent arteriole?
|
Decreased GFR, Decreased RPF, no change in filtration fraction.
|
|
|
|
What is the effect on GFR, RPF, and filtration fraction of constricting the efferent arteriole?
|
Increased GFR, decreased RPF, increased filtration fraction.
|
|
|
|
What is the effect on GFR, RPF, and filtration fraction of increased plasma protein?
|
Decreased GFR, no change in RPF, decreased filtration fraction.
|
|
|
|
What is the effect on GFR, RPF, and filtration fraction of a ureteral stone?
|
Decreased GFR, no change in RPF, decreased filtration fraction.
|
|
|
|
What happens to [K+] in the blood when there is metabolic acidosis?
|
Acidosis causes hyperkalemia, because H+ enters cells and shifts K+ out.
|
|
|
|
Where is the majority of HCO3- reabsorbed?
|
PCT. In the PCT, CA is present both intracellularly and in the lumen. Bicarb is reabsorbed at the basolateral surface with Na+
|
|
|
|
What happens to pH [HCO3-] when ECF volume expands?
|
Less HCO3- is reabsorbed because of low oncotic pressure in peritubular capillaries, so pH goes down. (With overhydration, edema)
|
|
|
|
What happens to pH [HCO3-] in dehydration?
|
PCT isosmotic reabsorption is stimulated due to high oncotic pressure. More bicarb is reabsorbed, pH goes up. (metabolic alkalosis).
|
|
|
|
What happens to pH in dehydration (due to AgII)?
|
Increased RAA system causes AgII stimulation of Na+/H+ exchanger and increased bicarb reabsorption. (alkalosis)
|
|
|
|
Where and how does the kidney create new bicarb?
|
1) Intercalated cells of the collecting duct: For every titratable acid filtered, a new bicarb is synthesized by CA as H+ is secreted into the lumen. 2) PCT: Glutamine is deaminated, NH4+ is exchanged for Na+. a-ketoglutarate breakdown gives bicarb.
|
|
|
|
What type of pH abnormality is caused by cocaine?
|
Respiratory acidemia - Depressed CNS respiratory center.
|
|
|
|
A patient has a panic attack. What type of pH imbalance results?
|
Respiratory alkalemia from hyperventilation.
|
|
|
|
A patient has had severe diarrhea. What pH abnormality results?
|
Metabolic acidemia due to excessive loss of HCO3-.
|
|
|
|
A patient is in kidney failure. What type of pH abnormality results?
|
Metabolic acidemia due to reduced excretion of acids.
|
|
|
|
What type of pH abnormality is present in a patient with COPD?
|
respiratory acidemia (too much CO2)
|
|
|
|
A patient has an adrenal adenoma. What type of pH abnormality is present?
|
Metabolic alkalemia. Increased aldosterone causes hypokalemia, which causes H+ to shift intracellularly.
|
|
|
|
Anion gap > 25 mM
|
Metabolic acidosis.
|
|
|
|
Anion gap = 10 mM
|
Normal.
|
|
|
|
Anion gap > 15 mM.
|
Potential metabolic acidosis.
|
|
|
|
Causes of metabolic acidosis.
|
Diabetic ketoacidosis, alcohol poisoning, drug OD.
|
|
|
|
In acidemia, what should happen to urine anion gap?
|
There should be a large negative gap, due to excretion of NH4Cl (hyperchloremic metabolic acidosis). If there is not a large negative gap with acidemia - suggests kidney failure.
|
|
|
|
Measured serum osm - calculated serum osm
|
Serum osmolal gap.
SOG > 15mM may be metabolic acidemia. SOG> 25mM is always metabolic acidemia. |
|
|
|
Unmeasured solutes that may increase SOG.
|
ketoacids, lactic acid, drug metabolites, methanol, ethanol.
|
|
|
|
A patient has an anion gap of 20. Bicarb is 21. What acid-base problem may be present?
|
Metabolic alkalosis. Anion gap is increased by 5, so Bicarb should decrease by 5 (to 19).
|
|
|
|
A patient has a defect in their luminal H+ ATPase in the distal tubule. What pH abnormality results?
|
Metabolic acidemia. (Type 1 RTA - decreased NH4+ and TA excretion)
|
|
|
|
A patient has Aldosterone deficiency. What pH abnormality results?
|
Metabolic acidemia. (Type 4 RTA). Aldosterone can't stimulate H+ ATPase and H+/K+ exchange. Hyperkalemia impairs NH4+ production and excretion. Tx by lowering K+.
|
|
|
|
Nothing. This is an artifact - talc from exam gloves.
|

If you saw the following on UA, what would you conclude?
|
|
|
|
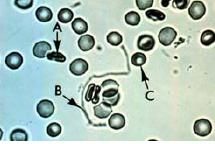
E. coli.
|
A UA from a patient showed the following. What organism is most likely the cause?
|
|
|
|
Budding yeast.
|

A UA from a patient shows the following. What is the problem?
|
|
|
|
Calcium oxalate crystal: associated with stones, large number with ethylene glycol.
|

What abnormality is associated with this UA?
|
|
|
|
Cholesterol crystal - seen with nephrotic syndrome and lipiduria.
|

This type of crystal is seen with what type of renal dysfunction?
|
|
|
|
Cystinuria. (cysteine crystals)
|
A child presented with this UA. What is the diagnosis?
|
|
|
|
Probably normal urine. This is a granular cast, which is made of protein, increased in strenuous exercise, dehydration, infection, chronic renal disease.
|

A marathon runner had this UA. What is the diagnosis?
|
|
|
|
This is a hyaline cast, which has no significance.
|

A patient presented with this UA. What is the diagnosis?
|
|
|
|
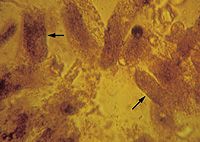
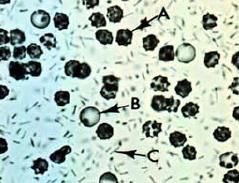
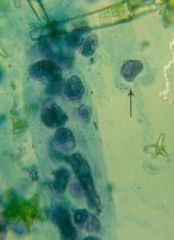
Mucous strands - indicative of infection, inflammation, or irritation.
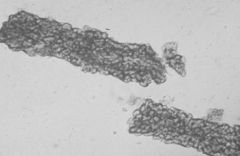
|

What is indicated by arrow A in this UA?
|
|
|
|
Nephritic syndrome - many rbc's. Nephrotic syndrome would show proteinuria, but not blood.
|
Is this UA more consistent with nephritic syndrome or nephrotic syndrome?
|
|
|
|
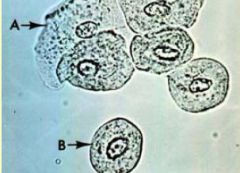
Transplant rejection. This is a renal tubular epithelial cell cast - indicated advanced tubular destruction, which may indicate rejection (or metal or drug poisoning, viral infection, pyelonephritis.)
|
A patient with a recent kidney transplant has this UA. What would you be concerned about?
|
|
|
|
This is a transitional epithelial cell - linig of renal pelvis, calyces, ureters, bladder, upper urethra. Often seen in catheterized patients.
|
What is the origin of Cell B in this UA?
|
|
|
|
Large numbers of squamous cells may indicate urine is contaminated with vaginal secretions.
|

The following is seen in the UA of a female patient. What does it indicate?
|
|
|
|
Trichomonas vaginalis infection (and contamination of urine with vaginal secretions).
|

This is found in the urine of a female patient. what does it indicate?
|
|
|
|
Probably none. These are triple phosphate crystals, which may be seen in normal urine, but also with elevated pH.
|
What is the clinical significance of this finding on UA?
|
|
|
|
Inborn error of metabolism - these are tyrosine crystals.
|

A child presents with the following UA. What is the diagnosis?
|
|
|
|
These are uric acid crystals, which accompany any condition with increased purine metabolism.
|
A patient with Lesch-Nyhan syndrome has the following UA. What is the significance?
|
|
|
|
Poor. These are waxy casts, which represent urinary stasis - dilated tubules that have undergone necrosis.
|
What is the prognosis for a patient with this UA?
|
|
|
|
This is a WBC cast. Would see with pyelonephritis, interstitial nephritis, sometimes GN.
|
In what types of renal disease would you see the following on UA?
|
|
|
|
What does a positive leukocyte esterase test indicate?
|
Presence of WBC. If the test is negative, it is very unlikely that there is an infection.
|
|
|
|
Three things that regulate PTH secretion
|
1) drop in plasma free Ca2+ and 2) hyperphosphatemia both increase PTH.
3) Calcitriol (active VitD) inhibits PTH synthesis. |
|
|
|
How does the parathyroid gland sense Ca2+ levels?
|
Through CASR, an integral membrane calcium responsive protein.
|
|
|
|
What is the molecular mechanism of PTH activity?
|
Activates G-protein coupled receptor - adenylate cyclase - cAMP - PLC and PKC pathways. Stimulates osteoblasts.
|
|
|
|
Where in the nephron is Ca2+ reabsorbed?
|
Passively in the PCT and loop of Henle. Actively in the distal tubule stimulated by PTH.
|
|
|
|
4 functions of interglomerular mesangial cells
|
1) physical support for capillaries.
2) phagocytic activity to maintain filtration slits. 3) contractile - regulate blood flow (pressure) 4) Secretion of prostaglandins and endothelins. |
|
|
|
What are juxtaglomerular cells?
|
Modified smooth muscle cells of the afferent arteriole which monitor BP, manufacture and secrete renin.
|
|
|
|
What are lacis cells?
|
extraglomerular mesangial cells. Function?
|
|
|
|
Describe the development of the pituitary gland.
|
In the 3rd week of development, 2 buds develop. One from the epithelium of the throat (Rathke's pouch), and one from the hypothalamus (neurohypophyseal bud - will become posterior pituitary). By 10 weeks, they begin to join. The sella turcica froms around the pituitary.
|
|
|
|
What is the origin of the ultimobranchial body, and what does it do?
|
Originates in the 4th pharyngeal pouch. Becomes the C Cells of the thyroid (parafollicular - calcitonin secreting)
|
|
|
|
What is a pheochromocytoma?
|
A tumor of the adrenal medulla - secretes epinephrine, NE.
|
|
|
|
What is the most common enzyme is missing in Congenital Adrenal Hyperplasia, and what is the result?
|
21-Hydroxylase. Result is deficiency of both cortisol and aldosterone. Electrolyte and fluid loss appear after the fifth day of life: hyponatremia, hyperkalemia, acidosis, dehydration, hypotension. Virilization of females.
|
|
|
|
2 factors that affect free plasma calcium level.
|
plasma protein level and pH. (Alkalosis causes decrease in free calcium)
|
|
|
|
What are three regulators of plasma calcium level?
|
1) PTH - increases Ca2+
2) 1,25-OH VitD increases 3) Calcitonin decreases |
|
|
|
4 regulators of PTH secretion
|
1) Low plasma Ca2+ increases
2) Hyperphosphatemia increases 3) High calcitriol inhibits 4) Normal Mg2+ is necessary |
|
|
|
How are plasma phosphate levels regulated?
|
Mainly through PTH acting in the proximal tubule to decrease Na+/Phosphate cotransporters in the luminal membrane.
|
|
|
|
Effects of PTH
|
Action on bone, kidney, intestine to restore plasma Ca2+ levels.
1) Immediate stimulation of osteoblasts, indirectly osteoclasts. 2) Stimulates Ca2+ reabsorption in Kidney - induction of calbindin. 3) Stimulates renal 1-hydroxylase, inhibits renal 24-hydroxylase (activation of Vitamin D) |
|
|
|
Symptoms of hypercalcemia
|
polyuria, polydipsia, fatigue, weakness, nausea, vomiting, pruritus, HTN, stones
|
|
|
|
What 2 diagnoses would be most likely for a patient presenting with asymptomatic glomerular hematuria?
|
IgA nephropathy and thin basement membrane nephropathy.
|
|
|
|
What is the major site of renal K+ regulation?
|
Principal cell of the CCD. K+ is excreted in response to incoming Na+ by the ROMK channel, and the MaxiK channel when urine flow is high.
|
|
|
|
How does hydrochlorothiazide affect K+?
|
It increases urine flow and reabsorption of Na+, both of which cause K+ to be excreted.
|
|
|
|
How Chloride affect K+?
|
If Cl- is low in the DCT, K+ will be lost. (anion effect)
|
|
|
|
How does insulin affect K+?
|
Shifts K+ into cells - can cause hypokalemia.
|
|
|
|
How does hypokalemia appear on an EKG?
|
Prominent U waves.
|
|
|
|
How does high serum glucose affect K+?
|
Shifts K+ out of cells and causes hyperkalemia.
|
|
|
|
How does renal failure affect K+?
|
Decrease of Na+ delivery to CCD causes K+ retention - hyperkalemia.
|
|
|
|
How does hyperkalemia appear on EKG?
|
Widened QRS, tall, thin T-wave.
|
|
|
|
How is hyperkalemia treated?
|
IV calcium gluconate stabilizes membranes rapidly. NaHCO3, insulin/glucose, albuterol all increase K+ uptake by cells. Hemodialysis to remove K+.
|
|
|
|
Substances reabsorbed and substances secreted in the DCT.
|
Reabsorbed: Na+, H20 (if ADH present), HCO3-.
Secreted: K+, urate, NH3. |
|
|
|
Mechanism of action, location, and example of carbonic anhydrase inhibitors.
|
Acetazolamide. Blocks conversion of H2CO3 to H+ and HCO3- at PCT. Blocks Na2HCO3 reabsorption (Na+/H+ exchanger). Causes mild metabolic acidosis. Weak diuretic.
|
|
|
|
What are indications for use of carbonic anhydrase inhibitors?
|
open angle glaucoma, mountain sickness, metabolic alkalosis.
|
|
|
|
Mechanism of action, location, and example of osmotic diuretic.
|
Mannitol. Freely filtered but poorly reabsorbed. PCT and thin limbs osmotic reabsorption of Na+ and fluid. Acutely causes hyponatremia, but later hypernatremic dehydration if water is not replaced. Useful in cerebral edema.
|
|
|
|
Mechanism of action, location, and example of Loop diuretic.
|
Furosemide. Blocks Na+/K+/2Cl- transporter in thick ascending limb. Blocks Na+ reabsorption and increases K+ and H+ excretion. Hypokalemic metabolic alkalosis if KCl not repleted. Increase excretion of Ca2+ and Mg+.
|
|
|
|
Indications for use of loop diuretics?
|
Moderate to severe edema with CHF, cirrhosis, nephrotic syndrome, hypercalcemia. Rapid onset, short half-life.
|
|
|
|
Mechanism of action, location, and example of thiazide diuretics.
|
Hydrochlorothiazide. Early DCT blocks thiazide-sensitive Na+/Cl- cotransport. Hypokalemia, metabolic alkalosis, hypercalcemia possible. Drug of choice for HTN.
|
|
|
|
Indications for the use of thiazide diuretics.
|
HTN, mild edematous conditions, hypercalciuria, nephrogenic diabetes insipidus. SFx: hypokalemic alkalosis, impaired CHO tolerance, increased LDL and total cholesterol.
|
|
|
|
Mechanism of action, location of action of spironolactone.
|
Competitive antagonist of aldosterone at mineralcorticoid receptors - DCT. Mild Mg2+, Ca2+ sparing - mech unknown.
|
|
|
|
Mechanism of action, location of action of triamterene and amiloride.
|
Principal cells of the DCT, CD - block Na+/K+ exchange. Mild short-term natriuresis, reduced excretion of K+ and H+.
|
|
|
|
Indications for use of K+ sparing diuretics.
|
mild edema, use in HTN combined with loop diuretics to prevent hypokalemic alkalosis, use where aldosterone levels are high, tx hirsutism in women.
|
|
|
|
What diuretic is useful for treating renal tubular acidosis with hypercalcemia?
|
Furosemide.
|
|
|
|
What diuretic is useful for treating nephrolithiasis, osteoporosis, diabetes insipidus?
|
Thiazides.
|
|
|
|
Which diuretic produces the following side effects: hypercalcemia, metabolic alkalosis, hyponatremia, hyperglycemia, hyperlipidemia, hyperuricemia?
|
Thiazides.
|
|
|
|
What diuretic produces the following side effects: hypomagnesemia, metabolic alkalosis?
|
Loop diuretics.
|
|
|
|
What diuretic may produce metabolic acidosis?
|
Carbonic anhydrase inhibitors.
|
|
|
|
What does deiodinase do?
|
Converts T4 to T3.
|
|
|
|
Lab tests show: normal TSH, High TT4, High TT3, Low T3 reuptake, normal FT4. Dx?
|
TBG excess: pregnancy, congenital, estrogen.
|
|
|
|
Lab tests show: Low TSH, High TT4, High TT3, High T3 reuptake, High FT4. Dx?
|
Hyperthyroidism: Grave's Dz, multinodular goiter, struma ovarii, exogenous T4.
|
|
|
|
Lab tests show: Low TSH, Normal TT4, High TT3, Normal T3 reuptake, Normal FT4. Dx?
|
T3 toxicosis: toxic adenoma.
|
|
|
|
Lab tests show: Low TT4, High TT3, Low or normal T3 reuptake, Low FT4. Dx?
|
Cytomel ingestion.
|
|
|
|
Lab tests show: High TSH, High TT4, High TT3, High T3 reuptake, High FT4. Dx?
|
Secondary hyperthyroidism: TSH-secreting pituitary adenoma,
|
|
|
|
Lab tests show: normal TSH, Low TT4, Low TT3, High T3 reuptake, normal FT4. Dx?
|
TBG deficiency.
|
|
|
|
Lab tests show: Low TSH, Low TT4, Low TT3, Low T3 reuptake, Low FT4. Dx?
|
Secondary hypothyroidism.
|
|
|
|
Lab tests show: High TSH, Low TT4, Low TT3, Low T3 reuptake, Low FT4. Dx?
|
Primary hypothyroidism.
|
|
|
|
Lab tests show: High TSH, Normal TT4, Normal TT3, Normal T3 reuptake, Normal FT4. Dx?
|
Subclinical hypothyroidism.
|
|
|
|
Treatment of hyperthyroidism?
|
1) PTU (propothiouracil - blocks conversion of T4 to T3): Grave's, adenoma, TSH-secreting tumor.
2) Radioiodine: Grave's, not very useful for MNG, adenoma. |
|
|
|
Lab findings: increased TSH, increased T4, with no symptoms. Dx and Tx?
|
Generalized Thyroid hormone resistance - no Tx needed.
|
|
|
|
Lab findings: TSH normal, T4 normal, symptoms of thyroid deficiency. Dx and Tx?
|
Peripheral resistance to thyroid hormone. Tx w/T4.
|
|
|
|
Symptoms: osteoporosis, bone pain, dyspepsia, depression, nephrogenic diabetes insipidus. Dx?
|
Hyperparathyroidism, likely due to adenoma.
|
|
|
|
Symptoms: hypoglycemia, weight gain, hyperphagia. Dx?
|
Insulinoma.
|
|
|
|
Symptoms: HTN, headache, sweating, tachycardia, palpitations, sense of impending doom. Dx?
|
pheochromocytoma.
|
|
|
|
Symptoms: Hyperparathyroidism, pancreatic tumor, pituitary adenoma. Dx?
|
Wermer's syndrome - autosomal dominant mutation in MEN I tumor suppressor gene.
|
|
|
|
symptoms: medullary carcinoma of thyroid, pheochromocytoma. Dx?
|
Autosomal dominant mutation in RET protooncogene.
|
|
|
|
Symptoms of ACTH deficiency?
|
Hypotension, hypoglycemia, weakness, dehydration, nausea, weight loss.
|
|
|
|
Tx of prolactinoma?
|
Dopamine agonist (bromocriptine)
|
|
|
|
Tx of GH and TSH secreting pituitary adenomas?
|
Somatostatin analog (octreotide)
|
|
|
|
Tx of Cushing's (ACTH-secreting adenoma)?
|
adrenalectomy.
|
|
|
|
Indications for dialysis?
|
uremic encephalopathy, uremic neuroirritability, refractory hyperkalemia, refractory acidosis, refractory volume overload, uremic pericarditis, ethylene glycol ingestion, lithium, some OD.
|
|
|
|
pKa of the bicarbonate pair?
|
6.1
|
|
|
|
Anion gap > 25
|
metabolic acidosis
|
|
|
|
Hypochloremic metabolic acidosis
|
Kidneys excreting NH4Cl to compensate - increased negative urine ion gap
|
|
|
|
Causes of hyperchloremic metabolic acidosis.
|
Loss of HCO3- by diarrhea or decreased reabsorption in PCT.
|
|
|
|
Rapid acting insulin for meals.
|
Lispro or Aspart.
|
|
|
|
Intermediate-acting insulin (2 hr onset, last for 6 hrs)
|
NPH
|
|
|
|
Long acting insulin.
|
Glargine.
|
|
|
|
Drug that sensitizes tissues to insulin, decreases gluconeogenesis in liver.
|
Biguanides (Metformin). SFx: diarrhea, lactic acidosis (ContraIx in renal impairment).
|
|
|
|
Oral insulin secretagogues.
|
Tolbutaminde, Glyburide, Glipizide, Repaglinide, Nateglinide.
|
|
|
|
Mechanism and examples of sulfonylureas.
|
Glyburide, Glipizide, Tolbutamide. Inhibit K+ channels in pancreatic beta cells, prolong depolarization, increase Ca2+, sustained insulin release. Sfx: hypoglycemia, weight gain.
|
|
|
|
Mechanism and examples of Meglitinides.
|
Repaglinide, Nateglinide. Stimulate rapid, brief insulin secretion in response to glucose by inhibition of K+ channels in beta cells. Sfx: weight gain, hypoglycemia.
|
|
|
|
Mechanism and examples of alpha glucosidase inhibitors.
|
Acarbose, Miglitol. Decrease intestinal absorption of glucose. Sfx: abdominal discomfort, gas, contraindicated with IBD, cirrhosis.
|
|
|
|
Mechanism and examples of Thiazoladindiones.
|
Pioglitizone, Rosiglitizone: increase insulin uptake by muscle and adipose cells by upregulating GLUT4. Decreases hepatic gluconeogenesis. Benefit: helps LDL. SFx: weight gain, edema, hypoglycemia, Contraindicated in CHF, liver dysfx.
|
|
|
|
Drugs that sensitize the body to insulin.
|
Thiazolidindiones (Pioglitazone) and biguanides (Metformin).
|
|
|
|
Drugs that stimulate insulin release.
|
Sulfonylureas (Glipizide) and Meglitinides (Repaglinide).
|
|
|
|
Drugs that slow the absorption of carbohydrates.
|
Alpha-glucosidase inhibitors (Acarbose).
|
|
|
|
Drugs that slow gastric emptying, suppress glucagon secretion, and decrease appetite.
|
Amylin analogues. (Pramlintide, Symlin)
|
|
|
|
Drugs that enhance glucose-dependent insulin secretion in response to food.
|
Incretin mimetics (exenatide, Byetta)
|
|
|
|
Factors affecting free plasma Ca2+
|
plasma protein level, PTH, VitD, PO4-, pH (decreased free Ca2+ with alkalosis)
|
|
|
|
In positive Ca2+ balance, what does kidney do to VitD?
|
Hydroxylates at 24 position to inactivate.
|
|
|
|
In negative Ca2+ balance, what does kidney do to VitD?
|
Hydroxylates at 1 position to activate to calcitriol.
|
|
|
|
Causes of hypercalcemia
|
primary hyperparathyroidism, familial benign hypocalciuric hypercalcemia, sarcoid and granulomatous dz, malignancies, endocrinopathies, drug-induced, immobilization, ARF.
|
|
|
|
What is the effect of anticholinergic drugs (antipsychotics, antidepressants) on the urinary system?
|
Urinary retention. They block the parasympathetic action on the detrussor muscle.
|
|
|
|
What is the sympathetic innervation of the bladder?
|
Dome of the bladder is innervated by beta-adrenergics (stimulation causes relaxation); bladder neck by alpha-adrenergics (stimulation causes contraction) - overall effect of sympathetic stimulation is urinary retention.
|
|
|
|
What is the cause of urge incontinence?
|
Overactive detrussor (MS, parkinsonism, bladder carcinoma, cystitis, BPH); or alcohol, caffeine, diuretics, sedatives. Tx with anticholinergics (oxybutynin or tolterodine, TCA, Ca2+ channel blocker.)
|
|
|
|
What is the cause of overflow incontinence?
|
Detrussor underactivity (diabetes, obstruction, disc compression, pelvic surgery)or high sphincter activity (obstruction - BPH, stricture).
|
|
|
|
What is the cause of stress incontinence?
|
Sphincter laxity.
|
|
|
|
Indications for dialysis in CKD?
|
Severe volume overload with CHF, pericarditis, severe electrolyte abnormalities, life-threatening acidosis, bleeding with BUN>100, advanced uremic symptoms.
|
|
|
|
Uremic symptoms?
|
bruising/bleeding, drowsiness, confusion, coma, muscle twitching, seizures, pruritus, headache, nausea, vomiting, hiccups, foot drop, altered skin and nail color.
|
|

