![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
112 Cards in this Set
- Front
- Back
|
How many WBCs should there be in a liter of blood?
|
WBCs: in health, there should be 4.4-11.3 x 109/L of WBCs in blood.
|
|
|
What percent of plasma cells are found in blood?
|
• Its important to know that in health, there should never be plasma cells in the blood.
|
|
|
Which leukocyte includes the following properties?
Bactericidal “left shift”: increase in immature precursors |
Neutrophils (PMNs)
|
|
|
Which leukocyte includes the following properties?
allergic, anti-parasitic, drug, neoplasms |
Eosinophils
|
|
|
Which leukocyte includes the following properties?
immediate hypersensitivity reactions; ie, asthma |
Basophils
|
|
|
Which leukocyte includes the following properties?
“the mononuclear phagocyte system;” blood monocytes + those carried to peripheral tissues-> histeocyte or macrophage: bacteria, fungi, mycobacteria, protozoa, virus, take up senescent cells, antigen presentation |
Monocytes
|
|
|
What is the percentage of T lymphocytes compared to the rest of the lymphocytes?
|
80-90% of Lymphocytes
|
|
|
What is leukopenia usually attributed to?
|
A decrease in neutrophils (i.e. neutropenia or granulocytopenia)
|
|
|
What are the causes of Lymphopenia?
|
HIV
Glucocorticoids Drugs Autoimmune Acute viral Malnutrition |
|
|
What can be due to Decreased Production & Increased Destruction?
|
Neutropenia and Agranulocytosis
|
|
|
What are some Drugs that are attributed to increased destruction in Neutropenia and Agranulocytosis?
|
◊ Alkylating agents, antimetabolites
Choramphenical, sufonamides, chlorpromazine, thiouracil |
|
|
What are the clinical manifestations of Neutropenia & Agranulocytosis?
|
Infections (deep w/gray, green-black necrotic membranes)
Ulcerating Lesions of the: *Gingiva *Floor of Mouth *Buccal Mucosa *Pharynx *Oral Cavity (agranulocytic angina) *Elsewhere in body |
|
What are the 5 pools?
|
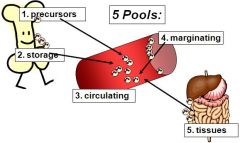
1. Precursors
2. Storage 3. Circulating 4. Marginating (cells stuck to the walls of the vessels) 5. Tissues |
|
|
What condition occurs due to too many leukocytes?
|
Reactive Leukocytosis
|
|
|
What is the difference in site and spread between Hodgkin's Lymphoma & NHL?
|
Hodgkin - Single node; contiguous; Rarely involves waldeyer ring & mesentery
NHL - Multiple nodes; Extranodal; Unpredictable spread; Waldeyer ring & mesentery |
|
|
What are the broad classifications for Neoplastic Lymphoid Disorders?
|
1. Lymphoid Neoplasms (has Hodgkin's Lymphoma)
2. Myeloid Neoplasms 3. Histiocytoses |
|
|
What is the characteristic cell found in Hodgkin's Lymphoma?
|
Reed-Sternberg
|
|
|
What are these classified as?
*Acute myelogenous leukemias *Myelodysplastic syndromes *Chronic myeloproliferative disorders |
Myeloid Neoplasms
|
|
|
What cell has the following properties?
in a non-neoplastic inflammatory background (EOS) Classically has two big nuclei that look like owl eyes. |
Reed-Sternberg
|
|
|
What kind of cells does non-classical hodgkin lymphoma have?
|
Popcorn or L&H cells (lymphocytic & histeocyte Reed-Sternberg variants)
|
|
|
What are the types of classical Hodgkin's Lymphoma?
|
1. Nodular Sclerosis
2. Mixed Cellularity 3. Lymphocyte Rich 4. Lymphocyte-depleted (least favorable diagnosis) |
|
|
What is the most common type of lymphoma?
|
Chronic Lymphocytic Leukemia (CLL)/Small Lymphocytic Lymphoma (SLL)
|
|
|
What type of lymphoma Always involves bone marrow & commonly the spleen. It also has Cytopenias: bleeding & infection?
|
CLL/SLL
|
|
|
What is the most common NHL?
|
Follicular Lymphoma
|
|
|
What type of lymphoma has t(14:18)?
|
Follicular Lymphoma
t(14:18) 14 is the heavy change locus of immunoglobulins |
|
|
What type of lymphoma is: *Indulent & Incurable
*BCL-2 expression (normal germinal centers are BCL-2 neg) *t(14:18) *A lymph node w/many follicles; normal architecture effaced |
Follicular Lymphoma
|
|
|
What type of lymphoma has t(11:14)?
|
Mantle Cell Lymphoma
|
|
|
What type of lymphoma has the properties:
*t(11:14) *Cyclins D-1 protein |
Mantle Cell Lymphoma
|
|
|
What type of lymphoma ARISES AS A SINGLE RAPIDLY GROWING, SYMPTOMATIC MASS?
|
Diffuse Large B-cell Lymphoma
Aggressive- requires intense chemotherapy Large neoplastic cell size, diffuse growth pattern |
|
|
What are the different types of plasma cell neoplasms?
|
MGUS (monoclonal gammopathy of uncertain significance)
Waldenstrom Macroglobulinemia |
|
|
What is the prognosis of multiple myeloma?
|
Poor Prognosis
Die within 3-5 years |
|
|
What is the plasma cell content in bone marrow for Multiple Myeloma?
|
>30% plasma cells in marrow
|
|
|
What type of lymphoma displays symptoms of Infection, Renal Insufficiency, Hypercalcemia (due to the break-down of bone)
|
Multiple Myeloma
|
|
|
What is significant regarding ALLs & AMLs?
|
They can have identical signs and symptoms
|
|
|
Who is affected most in ALL (Acute Lymphoblastic Leukemia)?
|
Younger people are affected
(80% B-cell precursors, 20% T-cell precursors) |
|
|
Who is affected most in AML (Acute Myelogenous Leukemia)?
|
Adults
|
|
|
What does the cellular composition of AML look like?
|
Have looser nuclei
Prominent nucleoli More cytoplasm often with Granules |
|
|
What type of lesions are common with AML (Acute Myelogenous Leukemia)
|
Mouth/Throat Ulcers
|
|
|
**What type of leukemia has the following properties?
*t(15:17) PML/RARα *usually present w/DIC *Response to RETINOIC ACID as a treatment |
Acute Promyelocytic Leukemia
|
|
|
What has Birbeck granules in the cytoplasm (electron microscopy)?
|
Langerhans Cell Histiocytosis
(neoplastic cell is a dendritic cell) |
|
|
What are the different types of Myeloproliferative Disorders?
|
Myeloproliferative Disorders
Chronic Myelogenous Leukemia (CML) Polycythemia Vera Essential Thrombocytosis Primary Myelofibrosis |
|
|
What are common symptoms of Myeloproliferative Disorders?
|
Splenomegaly
Spent phase cytopenias and marrow fibrosis Can progress over time to acute leukemia (CML invariably does) |
|
|
What type of Myeloproliferative disorder has a Philadelphia (Ph1) chromosome: t(9:22)?
|
Chronic Myelogenous Leukemia (CML)
Translocation is present in 95% of cases BCT-ABL fusion (tyrosine kinase activity; unregulated myeloproliferation!) Gleevec (imtinib) inhibits tyrosine kinase |
|
|
What stage of Acute Leukemia (AML) is M0?
|
minimally differentiated
|
|
|
What stage of Acute Leukemia (AML) is M1?
|
Without maturation
|
|
|
What stage of Acute Leukemia (AML) is M2?
|
With maturation (AUER RODS)
|
|
|
What stage of Acute Leukemia (AML) is M4?
|
Myelomonocytic
|
|
|
What stage of Acute Leukemia (AML) is M5?
|
M5a = Monoblasts
M5b = Monocytic |
|
|
What stage of Acute Leukemia (AML) is M6?
|
Erythroleukemia
|
|
|
What stage of Acute Leukemia (AML) is M7?
|
Magakaryoblastic
|
|
|
What condition has the following features?
• Men,50-60 yrs. • Multiple skeletal sites “punched out” lesions § Plasma cells invade and erode bone. • Erode bone • pathologic fractures • Marrow: for diagnosis, you will have to have >30% plasma cells § You should normally have no more than 2% • M-component: 55% IgG; § serum IgG>3.5g/dL,IgA>2g/dL • *Rare to see plasma cells in peripheral blood • *Infection, renal insufficiency, hypercalcemia (due to the breakdown of bone) • Poor prognosis: Die within 3-5 years |
Multiple Myeloma
|
|
|
What disorder has a Monoclonal spike of IgG?
|
Multiple Myeloma
|
|
|
Leukemia Clue: Children
|
ALL
|
|
|
Leukemia Clue: Myeloblasts
|
AML
|
|
|
Leukemia Clue: Auer Rods
|
AML, promyelocytic
|
|
|
Leukemia Clue: DIC
|
Promyelocytic
|
|
|
Leukemia Clue: Elderly
|
CLL
(chronic lymphocytic leukemia) |
|
|
Leukemia Clue: Splenomegaly
|
CML
|
|
|
Leukemia Clue: Philadelphia Chromosome
|
CML
|
|
|
Leukemia Clue: Tartrate-resistant acid phosphatase
|
Hairy Cell
|
|
|
Leukemia Clue: HTLV-1
|
Adult T cell
|
|
|
What is the major difference between Multiple Myeloma & Waldenstrom Macroglobulinemia?
|
Lack of lytic bone lesions in Waldenstrom
|
|
|
What is the major difference between Acute Leukemias and Chronic Leukemias?
|
Acute Leukemias have blasts in peripheral blood and decreased mature cells
Chronic Leukemias have an increased number of mature WBCs in the peripheral blood |
|
|
What is significant about Leukocyte alkaline phosphatase?
|
It is elevated in inflammatory leukocytosis
It is depressed in chronic myelogenous leukemia |
|
|
Where is factor VIII synthesized?
|
Factor VIII is synthesized in the endothelium of vessels
(the other clotting factors are synthesized in the liver) |
|
|
What condition has a JAK-2 mutation (pH absent) & Low erythropoietin levels (vs. relative polycythemias)
|
Polycythemia Vera
|
|
|
What type of lymphoma is associated w/EBV and displays a starry sky pattern?
|
Burkitt Undifferentiated Lymphoma
|
|
|
What are normal levels of hemoglobin (gm/dL)?
|
Male 13.6-17.2
Female 12-15 |
|
|
What are normal levels of HCT (hematocrit)?
|
Male 39-49
Female 33-43 |
|
|
What is the normal MCV (mean cell volume)?
|
82-96
|
|
|
What is the definition of anemia?
|
Reduced Oxygen carrying capacity of blood
|
|
|
What lab values are reduced in anemia?
|
hematocrit HCT
hemoglobin Hb |
|
|
_______ is the percentage of whole blood that is RBCs
|
Hematocrit
|
|
|
___________________ is the coefficient of variation of red blood cell volume
|
Red Blood Cell Distribution Width (RDW)
|
|
|
_____________ is the average concentration of Hb in a volume of RBCs
|
Mean cell hemoglobin concentration (MCHC)
|
|
|
___________ is the average content of Hb per RBC
|
Mean Cell Hemoglobin (MCH)
|
|
|
_________ is the average volume of a RBC
|
Mean Cell Volume (MCV)
|
|
|
What are the causes of Megaloblastic anemia?
|
B12, Folate deficiency
Drug use |
|
|
Why do RBC's need to have highly pliable membranes?
|
To navigate between splenic sinusoids
|
|
|
What type of anemia has a membrane that is less stable and inflexible resulting in the erythrocyte not being able to leave the spleen. Condition is congenital and the RBC life span is decreased to 10-20 days?
|

Hereditary Spherocytosis (hemolytic anemia)
**Mutation in ANKYRIN, a component of the RBC membrane |
|
|
What type of anemia protects against malaria?
|
Glucose-6-Phosphate Dehydrogenase Deficiency (G6PD)
|
|
|
What shows up clinically as hemolysis after exposure to oxidant stress (drugs, foods-fava beans, infection)?
|
G6PD deficiency
|
|

What is shown in this picture and what anemia causes it?
|

Bite cells & Heinz Bodies
Caused by G6PD deficiency |
|
|
In sickle cell disease defective hemoglobin is produced due to ________
|
Valine instead of Glutamic acid
|
|
|
Among those with sickle cell disease (S/S), what percentage have what types of hemoglobin?
|
80% HbS
20% HbF NO HbA |
|
|
Among those with sickle cell trait(A/S), what percentage have what types of hemoglobin?
|
60% HbA
40% HbS |
|
|
What is the abnormal hemoglobin in sickle cell patients?
|
HbS
|
|
|
What is the % hemoglobin of normal adults?
|
96% HbA
|
|
|
What is the % hemoglobin of normal babies?
|
75% HbF
25% HbA |
|
|
What is the problem with HbS being sticky?
|
The stickiness leads to cells “hanging” around in these sluggish areas; which exposes them to hypoxic environmnet, the sickling persists, the tissues become inflamed, blood flows EVEN SLOWER, WBCs release pro-imflammatory cytokines; it’s a vicious cycle!!!
|
|
|
What are the treatments for sickle cell anemia?
|
Hyroxyurea: increases HbF, which inhibits polymerization of HbS, decreased inflammation
Crises: exchange transfusion |
|
|
What are Thalassemias?
|
Decreased synthesis of NORMAL alpha or beta hemoglobin chain
|
|
|
What is the problem we run into with Alpha Thalassemia?
|
Excess of unpaired Beta chains
|
|
|
What is the problem we run into with Beta Thalassemia?
|
Excess of unpaired Alpha chains
|
|
|
Where does hemolytic anemia (increased destruction)occur?
|
Mostly in Spleen (EXTRAVASCULAR HEMOLYSIS)
Rarely in the vessels (INTRAVASCULAR HEMOLYSIS) |
|
|
What type of anemia is congenital with a mutation in ANKYRIN, a component of the RBC membrane?
|
Hemolytic Anemia: HS (hereditary spherocytosis)
|
|
|
What type of anemia protects against Malaria (plasmodium falciparum)?
|
Hemolytic Anemia: G6PD deficiency
Glucose-6-Phosphate Dehydrogenase Deficiency |
|
|
What is:
- An intermittent hemolytic anemia of OLDER RBCs - Hemolysis after exposure to oxidant stress (drugs, foods-fava beans, infection) - Heinz bodies (MACROPHAGES IN SPLEEN PLUCK THEM OUT OF MEMBRANE -> BITE CELLS |
Hemolytic Anemia: G6PD Deficiency
|
|
|
In Hemolytic Anemia: Sickle Cell Disease, those with disease have what type of hemoglobin?
|
80% HbS
20% HbF **NO HbA** |
|
|
In Hemolytic Anemia: Sickle Cell Disease those with trait (A/S) what is the hemoglobin content?
|
60% HbA
40% HbS Patient functions fairly well |
|
|
Which Thalassemia targets cells?
|
Beta Thalassemia
|
|
|
What condition has an acquired defect in RBC membrane, a mutation in phosphatidykinositol glycan A (PIGA), a GPI protein
|
Paroxysmal Nocturnal Hemoglobinuria (PNH)
|
|
|
Which disease has RBCs susceptible to lysis by complement - there is a decrease in ALL GPI proteins
*CD55, 59 |
Paroxysmal Nocturnal Hemoglobinuria (PNH)
|
|
|
In Paroxysmal Nocturnal Hemoglobinuria (PNH), ALL RBCs ARE NOT AFFECTED. Why?
|
A mutant clone exists as well as normal RBCs Present
|
|
|
In RBC destruction due to trauma what shows up on a peripheral smear?
|
RBC fragments AKA SCHISTIOCYTES
|
|
|
What test for Immunohemolytic anemia demonstrates AB or complement bound to patient's RBCs?
|
DAT (direct antiglobulin test) "Coombs Test"
- antihuman Ig - a + test has clumping/agglutination |
|
|
What disease has laboratory findings of Hypochromic microcytic anemia (Decreased MHC & MCV)?
|
Iron Deficiency Anemia
|
|
|
What is important regarding anemia of chronic disease?
|
Impaired Fe utilization secondary to a chronic disease (i.e. rheumatoid arthritis, infections)
|
|
|
What type of anemia has Hypersegmented neutrophils & pancytopenia?
|
megaloblastic anemia
|
|
|
What are the properties of polycythemia?
|
- Non-clonal increase in the concentration of red blood cells unlike myeloproliferative disorders
- Causes: Increased EPO (tumor or hypoxemia) & Dehydration - Clinically patients present w/difficulty breathing & thrombosis - Treatment includes therapeutic phlebotomy or hydration |
|
|
What type of anemia presents clinically as:
- mucocutaneous bleeding and infections - splenomagaly - reticulocytopenia - normocytic, normochromic anemia |
Aplastic Anemia
*************** |
|
|
Will vessel wall damage affect blood test results?
|
No
|

