![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
155 Cards in this Set
- Front
- Back
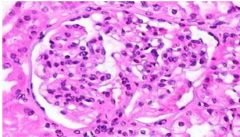
What glomerular nephropathy is pictured? What are the key features?
|
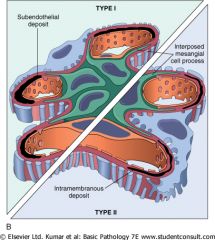
• Membranoproliferative glomerularnephritis
• Characterisitc apperance is "tram-tracking" due to splitting of the basement membrane because of sub-ENDOTHELIAL (Type I) or intramembranous depositis (Type II). |
|
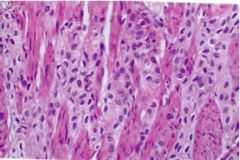
What disease is pictured?
What population does it affect? Where is the primary lesion? |
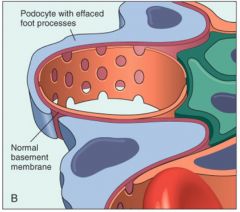
• Minimal Change Glomerulopathy (Liphoid nephrosis)
• Primarily affects children • 1º lesion is in the visceral epithelium (podocytes) --> effacement |
|
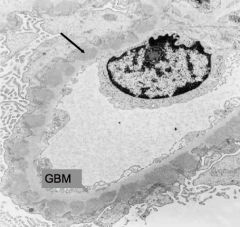
What disease is pictured? (See arrow) How does it present?
|
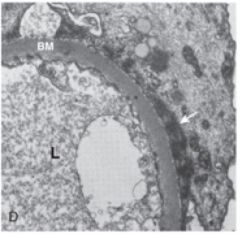
• Minimal Change Disease (Liphoid nephritis)
• Presents in children with selective proteinuria (child often has edema) dues to effacement of the podocytes |
|
What disease is pictured? What is the pathophysiology? Does it present with non-selective or selective proteinuria?
|
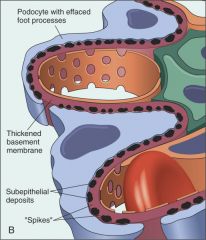
• (Diffuse) Membranous nephropathy
• Caused by the deposition of *subEPITHELIAL Ig-complexes* along the GBM (-situ immune complex formation) • Non-selective because MAC damages capillary walls |
|
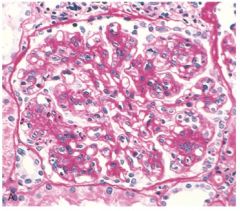
What nephropathy is pictured? What is the classic sign called? What is it due to?
|
• Diffuse Membranous Nephropathy
• Caused by the deposition of *subEPITHELIAL Ig-complexes* along the GBM (in-situ immune complex formation) • Referred to as "spike & dome" appearance on silver stain |
|
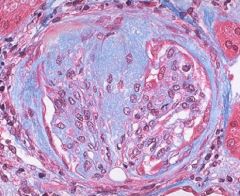
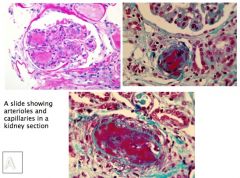
What is nephropathy is pictured? What stain? What stains blue?
|
• Focal segmental glomerularsclerosis
• Trichrome stain - to show that hyalinosis is infact, sclerosis • blue stains collagen |
|
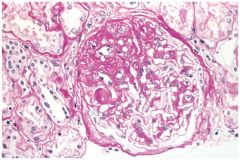
What nephropathy is shown?
What stain? What key features can be seen? |
• Focal segmental glomerularsclerosis
• PAS stain • Can see mass of scarred, obliterated capillary lumens w/ accumulation of matrix material, that has replaced a portion of the glomerulus (aka: hyalinosis & sclerosis) |
|
What nephropathy is pictured?
What is the characteristic appearance? |
• Membranoproliferative Glomerularnephritis
• Characterisitc apperance is "tram-tracking" due to splitting of the basement membrane because of sub-ENDOTHELIAL (Type I) or intramembranous depositis (Type II). |
|
|
Most common cause of nephrotic syndrome in children
|
Minimal change disease
(Liphoid nephrosis) |
|
|
Characterized by glomeruli that:
• have normal appearance in light microscope • show diffuse effacement of podocyte foot processes when viewed with EM • proximal convoluted tubules laden w/ protein droplets & lipids |
Minimal change disease
(Liphoid nephrosis) PCT laden w/ protein & lipid droplest is 2º to the 1º disorder and is due to reabsorption of lipoproteins passing through the diseased glomeruli |
|
|
Is Minimal change disease present with selective or non-selective proteinuria?
Where is the lesion located? |
• Selective proteinuria
• Lesion is located in the visceral epithelium (podocytes are effaced) |
|
|
What does effacement of the podocytes in Minimal change disease cause?
|
• Defect in charge barrier (loss of negative charge)
• Obliterates the network of arcade between the podocytes and glomerular BM |
|
|
What causes the loss of negative charge in the glomerular basement membrane in Minimal change disease?
|
T-cell cytokines
[Pathology due to defect in charge barrier (loss of negative charge) and podocyte effacement --> obliterates the network of arcade between the podocytes and glomerular BM] |
|
|
What is the most common 1º cause of nephrotic syndrome in adults?
|
Membranous Nephropathy
|
|
|
Characterized by:
• the presence of *subEPITHELIAL Ig-containing deposits* along the GBM (caused by in-situ immune complex formation) • Granular staining in immunofluorescence • late in the disease may show *diffuse thickening* of the capillary wall |
Membranous Nephropathy
|
|
|
Membranous nephropathy can be 2º to what diseases?
|
• Infections
(Chronic HepB, syphilis, schistosomiasis, malaria) • Malignant tumors (particularly carcinoma of lung & colon and melanoma) •SLE • Exposure to inorganic salts (Gold, mercury) • Drugs (penicillamine, captopril, NSAIDS) |
|
|
While membranous nephropathy is characterized by the presence of *subEPITHELIAL Ig-containing deposits* along the GBM (caused by in-situ immune complex formation), what exactly causes the capillary wall to become leaky?
|
• Diffuse Membranous Nephropathy
• Complement Membrane attack complex (C5b-C9) forms pores in the podocytes that then liberate oxidants that damage the capillary walls |
|
|
Is Membranous nephropathy selective or non-selective? Why?
|
• Non-selective.
• Complement Membrane attack complex (C5b-C9) forms pores in the podocytes that then liberate oxidants that damage the capillary walls, not just the effacement of podocytes |
|
|
How does Membranous nephropathy appear of immunofluorescense?
|
• Granular pattern due to the presence of *subEPITHELIAL Ig-containing deposits* along the GBM
(caused by in-situ immune complex formation) |
|
|
While membranous nephropathy is characterized by the presence of *subEPITHELIAL Ig-containing deposits* along the GBM (caused by in-situ immune complex formation), what exactly causes the capillary wall to become leaky?
|
Complement Membrane attack complex (C5b-C9) forms pores in the podocytes that then liberate oxidants that damage the capillary walls
|
|
|
What nephropathy shows ↑ mesangial matrix, obliterated capillary lumens, and deposition of hyaline masses (hyalinosis) & lipid droplets?
|
Focal Segmental Glomerularsclerosis
|
|
|
What nephropathy is often associated with people who have HIV, use IV heroin, or have sickle-cell disease? (Commonly presents in young African-american males)
|
Focal Segmental Glomerularsclerosis
|
|
|
The recurrence of Focal segmental glomerularsclerosis in pts with transplanted kidneys suggests?
|
That there is a circulating mediator that causes damage to podocytes
|
|
|
What nephropathy is characterized by alteration in the GBM and mesangium that is caused by the proliferation of glomerular cells?
|
Membranoproliferative Glomerularnephritis
|
|
|
What nephropathy presents as hematuria or proteinuria in the non-nephrotic range whereas other’s have a combined nephrotic-nephritic picture? What is the pathogenesis?
|
Membranoproliferative Glomerularnephritis
• Caused by alteration in the GBM and mesangium that is due to the proliferation of glomerular cells |
|
|
What type of Membranoproliferative glomerularnephritis (MPGN) has an underlying pathology like serum sickness?
|
• Type I MPGN
• Caused by circulating immune complexes that deposit subENDOTHELIALLY • May also be associated w/ HepB&C, SLE, Shistosomiasis |
|
|
In what nephropathy does:
presence of C3 Nephritic factor (an auto-Ig to C3 convertase) --> prevent the degredation of C3 convertase --> sustained activation of C3 --> resulting in low levels of C3 ?? |
Membranoproliferative Glomerularnephritis Type II
|
|
|
What nephropathy presents w/ hypocomplementemia and either nephrotic or nephritic characteristics?
|
Membranoproliferative Glomerularnephritis Type II
|
|
|
How does Membranoproliferative Glomerularnephritis Type II present? What appears on EM? What is the pathogenesis?
|
• Presents w/ hypocomplementemia
• On EM you see intramembranous deposits (deposits w/in the basement membrane) • Due to persistent activation of C3, because c3 convertase is stabilized by C3 Nephrotic factor (C3NeF) |
|
|
What nephropathy shows proliferation of mesangial & endothelial cells, a thickened GBM, and “tram-track” appearance of silver or PAS stains?
|
Membranoproliferative Glomerularnephritis
|
|
|
What nephropathy is characterized by discrete subENDOTHELIAL electron-dense deposits?
|
Membranoproliferative Glomerularnephritis Type I
|
|
|
What nephropathy has a GBM that is transformed into an irregular, ribbon-like, extremely electron dense structure?
|
Membranoproliferative Glomerularnephritis Type II
• Resulting from the deposition of a material of unknown composition (referred to as dense deposits) in the basement membrane • Due to persistent activation of C3 (due to stabilized C3 convertase) |
|
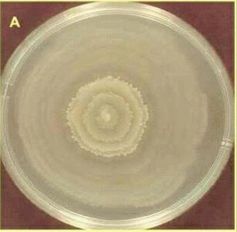
What test is shown? What is it used to detect? What makes this bacteria unique w/r/t UTIs?
|
• Swarming test
• Proteus mirabilis • Proteus mirabilis is well known for being urease(+). The enzyme urease breaks down of urea into carbon dioxide and ammonia. This alters urine pH, leads to the production of Staghorn calculus stones (Mg & Ph), and alkaline urine that smells of ammonia. |
|

What opportunistic pathogen is likely pictured? How do you know? What shape is this bacteria and G( )?
|
• Pseudomonas aeruginosa
• grows with pyocyanin or pyoverdin (Blue-green) colonies • Pseudomonas aeruginosa are G(-) rods |
|
|
What type of pathogens are the most common causes of UTIs? How do they occur? What is the normal defense mechanism?
|
• Normal flora
• They occur by ascending the urethra • Major defense mechanism ≈ flow of urine |
|
|
Definition: bladder or kidney infxns in healthy, young, non-pregnant women
|
Acute uncomplicated UTIs
|
|
|
Definition: bladder or kidney infections in individuals with underlying structural or functional abnormalities of the genitourinary tract (in men & women) associated w/ a condition that increases risk of failing Tx (multi-drug resistant pathogen)
|
Complicated UTIs
|
|
|
Definition: bacteria in the urine w/o symptoms or signs attributable to a UTI
|
Asymptomatic bacteriuria
|
|
|
Why do women have a higher susceptibility to UTIs?
|
• Shorter urethra
• Proximity to source of infection (anus) • Sex facilitates migration of pathogens • Use of spermicide ↑ risk of UTIs |
|
|
What can increase the risk for UTIs in men?
|
↑ risk correlated with onset of prostate hypertrophy
|
|
|
What is the main virulence factor involved in UTIs? What are the others?
|
• Main virulence factor: adhesion to epithelial cells (major determinant in pathogenicity)
• Other virulence factors: - capsular antigens - hemolysins - *urease* - intraoital colonization |
|
|
What bacteria are can be implicated in UNcomplicated UTIs?
|
• E.coli (80%)
• Staph saprophyticus (15%) • Other enterobacteriacae: --- Proteus mirabellus --- Klebsiella pneumoniae |
|
|
What bacteria are can be implicated in *complicated* UTIs?
|
• E.coli (20%)
The other 80%: • Proteus mirabellus • Klebsiella pneumoniae • Enterobacteriacae • Serratia • Pseudomonas aeruginosa • Enterococcus species • Group B strep • Staphylococcus aureus |
|
|
What are the characteristics of enterobacteriaceae?
Shape? G( )? Catalase? Oxidase? Other metabolic characteristics? |
• Gram (-) rods • Catalase (+) • *Oxidase (-)*
• Facultative anaerobes • Simple nutritional requirements • Ferment glucose • *Ferment lactose* • Reduce nitrAtes to nitrItes • resistant to bile salts mne: COG rod +-- “C= catalase, O = oxidase, G = gram” |
|
|
What does the enterobacteriacea use for adhesion? What does it use for movement? What other things are pili employed for?
|
• adhesion = common fimbirae pili
• movement: peritrichous flagella • sex pili: genetic transfer b/w bacteria (conjugated plasmids) |
|
|
What UTI-causing bacteria uses a Type III secretion system? What is a Type III secretion system?
|
• Enterobacteriacae
• Type III secretion system = a protein appendage found in several G(-) bacteria. In pathogenic bacteria, the needle-like structure is used as a sensory probe to detect the presence of eukaryotic organisms and secrete proteins that help the bacteria infect them. The proteins are secreted directly from the bacterial cell into the eukaryotic cell, also known as "the host" cell. |
|
|
What are the virulence factors of Enterobacteriacae?
|
• Exotoxins (lipopolysaccharide)
• adhesion factors (pili) • capsule • antigenic phase variation • *Type III secretion system* • Abx resistance |
|
|
What are the three components of the endotoxin of enterbacteriacae?
|
• Outer most ≈ somatic O polysaccharide
• Core & common to all entero. protein • Lipid A: mediates the toxic effects. Released at cell lysis --> systemic manifestations of G(-) bacterial infxns: activation of complement --> release of cytokines --> leukocytosis --> role in septic shock |
|
|
What are the antigens present on enterobacteriaceae? How are they distinct? How are they detected?
|
• O antigen: specific polysaccharides in the outer membrane - always present
• H: flagellar H proteins - only present on motile cells • K: Capsular polysaccharide antigens (not always present) • Detected via agglutination w/ specific Ig • Example: E.coli serovar O157:H7 |
|
|
What are the characteristics of Escheria coli?
Shape? G( )? Catalase? Oxidase? Other metabolic characteristics? |
• Gram (-) rods
• *Ferment lactose* (Lactose +) • Urease (-) |
|
|
What stains/agars are used to detect Escheria coli? How will they appear?
|
• MacConkey agar:
On MacConkey agar, deep red colonies b/c E.coli is lactose (+), & fermentation of this sugar will cause the medium's pH to drop, leading to darkening of the medium • Levine EMB agar: produces black colonies with greenish-black metallic sheen |
|
|
What pathologies can Escheria coli cause?
|
• UTIs
• Diarrheas • Neonatal meningits • Septicemia |
|
|
What are the virulence factors associated with Escheria coli?
|
Adherence:
• Pyelonephritis-associated pilus (P-pilus or PAP). *Binds to the digalactose (Gal-Gal) receptor on uroepithelial cells* • FimH (mannose-sensitive pilus): binds manosyalted proteins that line the bladder mucosa Damage: • Hemolysin: pore-forming cytotoxin • Lipopolysaccharide: inflammatory response |
|
|
What are the virulence factors of Escheria coli that are associated with adherence?
|
• Pyelonephritis-associated pilus (P-pilus or PAP). *Binds to the digalactose (Gal-Gal) receptor on uroepithelial cells*
• FimH (mannose-sensitive pilus): binds manosyalted proteins that line the bladder mucosa |
|
|
What are the virulence factors of Escheria coli that are associated with damage to the host cell?
|
• Hemolysin: pore-forming cytotoxin
• Lipopolysaccharide: inflammatory response |
|
|
What are the characteristics of Proteus mirabilis?
|
• G(-) rod
• Swarming motility • Urease (+) - important in the formation of stones and yields an alkaline urine • Lactose (-) |
|
|
What UTI causing G(-) rod is urease(+)?
|
Proteus mirabilis
|
|
|
What UTI causing G(-) rod is lactose(-)?
|
Proteus mirabilis
|
|
|
What UTI causing G(-) rod is urease(-)?
|
Escheria coli
|
|
|
What UTI causing G(-) rod is lactose(+)?
|
Escheria coli
|
|
|
What bacteria is most likely responsible for community and hospital acquired UTIs?
|
Proteus mirabilis
|
|
|
What are the virulence factors associated with Proteus mirabilis?
|
• Adhesins
• Motility (swarming) • Endotoxin --> Inflammatory response • Urease production --> higher pH = toxic to renal cells & potentiates the formation of urinary stones |
|
|
How does urease fxn as a virulence factor in UT infections? What bacteria produces it?
|
• Urease --> higher pH
---- toxic to renal cells ---- *↑ the formation of urinary stones* • Urease produced by Proteus mirabilis • Proteus mirabilis can lie dormant in urinary stones --> chronic infections • Stones can also block the flow of urine, ↓ natural cleansing mechanisms *Magnesium ammonium phosphate (MAP) stone (called "Staghorn calculus" or struvite) associated w/ urease producers; alkaline urine pH, urine smells like ammonia |
|
|
What other enterobacteriacea are associated with community & hospital acquired (catheter related) UTIs? What are their characteristics, shape? G( )? Nutritional requirements? Urease +/-?
|
• Klebsiella pneumoniae: G(-) non-motile, encapsulated rod. Lactose (+), Urease (-), Oxidase (-)
• Enterobacter: G(-) *motile*, rod. Lactose (+), Urease (-), Oxidase (-) • Serratia marcescens: G(-) rod. Urease (-), Oxidase (-). Slowly ferments lactose and produced a brick-red pigment |
|
|
What are the virulence factors associated with Enterobacteriaceae family? What are the most famous members of that group?
|
• Pili/adhesin: adherence to urinary epithelium
• Capsule: interferes w/ complement activtation, antiphagocytosis • Endotoxin: causes fever, inflammation (Lipopolysaccharide) |
|
|
What does the McConkey agar test discern?
|
McConkey agar is a culture medium used to grow G(-) bacteria and stain them for lactose fermentation.
• Lac(+): E. coli, Klebsiella. pneumoinae, Enterobacter • Lac (+/-): Serraita marcescens (slow fermentation - brick red) • Lac(-): Proteus mirabilis |
|
|
What does a urease test test for when culturing a common UTI culprit?
|
Tests (+) for Proteus mirabilis.
• Urease will change pH and change the color of the test: Red(+), Orange(-) • Urease catalyzes the breakdown of urea into CO2 and ammonia which alters urine pH --> formation of stones & alkaline urine |
|
|
What aerobic, motile G(-) rod that is oxidase (+) and does not ferment anything (adaptable to minimal nutritional requirements) is involved in many opportunistic infections, particularly those in cystic fibrosis patients?
|
Psuedomonas aeruginosa
|
|
|
What are the virulence factors associated with Pseudomonas aeruginosa?
|
• Adhesins (pili) --> adhesion to epithelial cells
• Polysaccharide capsule --> protection from phagocytosis • Endotoxin --> inflammation • Extracellular enzymes & toxins (Exotoxin A) --> tissue damage |
|
|
What G(-) rod and opportunistic pathogen sometimes associated with UTIs also produces mucoid?
|
Psuedomonas aeruginosa
|
|
|
What is the #1 cause of meningits in newborns?
|
Group B Streptococcus ≈ Streptococcus agalactiae
|
|
|
What G(+) cocci that appears like irregular clusters (grapelike) is implicated in 10-20% of the uncomplicated UTIs in sexually active young women?
|
Staphylococcus saprophyticus
|
|
|
What shape is Staphylococcus saprophyticus? G( )? Catalase ( )? Coagulase( )? Urease( )? Lipase( )? Phosphatase( )? Which feature distinguishes it from staphylococcus aureus?
|
• G(+) cocci, growing in grapelike clusters
• Catalase (+) • Coagulase (-) • Urease (+) • Lipase (+) • Phosphatase(-) • *Being coagulase (-) distinguishes it from Staph aureus which is coagulase (+)* |
|
|
What are the known virulence factors of Staphyloccus saprophyticus?
|
• adhesin: mediates attachment to bladder cells
|
|
|
A urine sample is cultured and there shows growth on blood agar with γ hemolysis and novobiocin resistance. What bacteria is most likely?
|
Staphylococcus saprophyticus
|
|
|
How does Staphylococcus saprophyticus present in a urine culture?
|
• Grows on blood agar
• Shows γ hemolysis (does not induce hemolysis) • Resistant to novobiocin |
|
|
What shape is enterococcus faecalis & faecium? G( )? Catalase ( )? Any other defining characteristics?
|
• G(+) diplococci or short chains
• Catalase (-) • Lancefield’s group D antigen |
|
|
What UTI causing bacteria is a G(+) diplococci (or short chain), catalase (-) and has a lancefields group D antigen? What other pathology does this bacteria present in?
|
• Enterococcus faecalis & faecium
• Also presents in endocarditis, wound infections, & bacteremia |
|
|
What is the source of infection if infected w/ Enterococcus faecalis & faecium?
|
• Endogenous flora
|
|
|
What are the virulence factors associated w/ enterococci?
|
• Not well known
• Adhesins • Toxins & enzymes: cytolysin, gelatinase, serine protease • *All strains carry some drug resistance* • Some strains are vancomycin-resistant! |
|
|
A urine culture is performed. When first cultured on blood agar there was no hemolysis. On a subsequent culture (later urine sample) there was partial hemolysis. The bacteria are also resistant to 40% bile salts, 6.5% NaCl, bacitracin & optochin, what is the most likely bacteria?
|
• Enterococcus faecalis & faecium
|
|
|
How does enterococcus present when cultured on blood agar?
|
• α or γ hemolysis
|
|
|
What tests are enterococcus resistant to?
|
• 40% bile salts
• 6.5% NaCl • bacitracin & optochin mne: makes sense, survives in gut where there is bile, salt, and sometimes abx |
|
|
What test can be used to clench the diagnosis of enterococci? What is it detecting the presence of?
|
• PYR (L-pyrrolidonyl-B-naphthylamide) test: to detect the presence of pyrrolidonyl peptidase
|
|
|
What is the sister strain to Group A streptococcus pneumoniae? What characteristics do they share?
|
Streptococcus agalactiae (Group B strep)
Shared characteristics: • G(+) cocci in short chains Different characteristics: • Group B Lancefield antigen • Strep. agalactiae = β-hemolytic • Strep. pneumoniae = α-hemolytic |
|
|
What bacteria that causes asymptomatic UTIs in pregnant women is a G(+) cocci in short chains, β-hemolytic, and is bile resistant?
|
• Group B Strep ≈ Streptococcus agalactiae
|
|
|
What bacteria that is in the same group as Streptococcus pyogenes causes asymptomatic UTI in pregnant women? What is a sequelae of that infection?
|
• Group B Strep ≈ Streptococcus agalactiae
• Sequelae = neonatal meningitis |
|
|
How does streptococcus agalactiae present when cultured on blood?
|
• Full hemolysis (β-hemolysis)
|
|
|
What are the virulence factors associated with Streptococcus agalactiae?
|
• Polysaccharide capsule (antiphagocytic)
• Peptidase (inactivates C5a, a major chemo-attractant of PMNs) • Hydrolytic enzymes (tissue destruction & systemic spread) |
|
|
What is the most common cause of neonatal meningits in the US?
|
Streptococcus agalactiae (Group B strep)
|
|
|
How does the presentation of cystitis differ from pyelonephritis?
|
Cystitis:
• superficial irritaion (no invasion of mucosa) • dysuria • urgency • frequency • often cloudy urine, sometimes gross hematuria • No fever Pyelonephritis • invasive disease • **flank pain & tenderness** • systemic manifestations (i.e. fever) |
|
|
What disorder presents with pelvic & low back pain? High fever, dysuria & frequency? And retention of urine due to obstruction.
|
Acute prostatitis
|
|
|
What minimally invasive disorder presents w/:
• dysuria • urgency • frequency • often cloudy urine, sometimes gross hematuria • No fever?? |
Cystitis
|
|
|
What invasive disease presents w/
• **flank pain & tenderness** • systemic manifestations (i.e. fever)? |
Pyelonephritis
|
|
|
What does a nitrite dipstick test for?
|
Detects nitrites produced by nitrate reducing uropathogens (**e.g., E. coli & enterobacteriacea**)
• test sensitivity and specificity is 30% and 90%, respectively • Requires ∼ 4 hr for nitrate reducing uropathogens to convert nitrates to nitrites and patients with UTI frequently have increased frequency of urination, which explains the tests poor sensitivity. |
|
|
What does the leukocyte esterase dipstick screen for? And specifically, what infections?
|
Detects esterase in neutrophils (pyuria)
• ≈ 80% sensitivity • Infections: urethritis, cystitis, pyelonephritis, sterile pyuria (neutrophils present but (-) standard urine culture): Chlamydia trachomatis urethritis, tuberculosis, drug-induced interstitial nephritis |
|
|
How would you distinguish b/w true bacteriuria & contaminated urine?
|
• Colony counts. ≥10^5 Colony forming units/mL of urine --> infection
|
|
|
What is the treatment for uncomplicated cystitis? What are the most likely pathogens?
|
• 3 days empiric therapy: TMP/SMZ or nitrofurantoin
• either Escherichia coli or Staphylococcus saprophyticus |
|
|
What is the treatment for uncomplicated pyelonephritis? What are the most likely pathogens?
|
• 10-14 days empiric therapy: fluroquinolone
• Usually Escherchia coli possibly Staphylococcus aureus (if cultured in urine) |
|
|
What is the treatment for complicated UTI in pregnant women? What is the most likely pathogen?
|
• Cephalosporin
• E.coli (20%) • Proteus mirabilis, Klebsiella pneumoniae, Enterobacter, Serratia, Pseudomonas aeruginosa, enterococcus species, Group B streptococci, Staph aureus (∑ 80%) |
|
|
What UTI-causing, G(-) bacteria uses a mechanism where a needle-like protein is used as a sensory probe to detect the presence of eukaryotic organisms and secrete proteins directly into the host cell?
What is the name of this mechanism? |
• Enterobacteriae
• Viruelence mechanism ≈ Type III secretion system |
|
|
What pathogen produces a brick-red pigment when cultured? Why does this occur?
|
Serratia marcescens, from the slow fermentation of lactose
mne: think of a marchesa outfit with dark brick red nail polish. |
|
|
BK polyoma virus: enveloped? DNA or RNA? ss or ds?
What cells does it infect in the urinary tract? Who does it tend to infect and what disease does it cause in those pts? |
• Non-enveloped, dsDNA virus
• Infects the epithelial cells of the urinary tract • Causes an acute interstitial nephritis manifesting as renal dysfunction in 1-10% of RENAL TRANSPLANT pts --> graft loss in 90% • Causes hemorrhagic cystitis in bone marrow transplant pts |
|
|
A renal transplant patient presents with an acute interstitial nephritis. PCR identifies a dsDNA virus. What is the most likely cause? What are possible complications?
|
BK polyoma virus
• Complication is graft loss in up to 90% of pts |
|
|
A bone marrow transplant patient presents with hemorrhagic cystitis. PCR identifies a dsDNA virus of the papovaviridae family. What is a possible cause?
|
BK polyoma virus
|
|
|
A pediatric bone marrow transplant patient presents with hemorrhagic cystitis. PCR identifies a non-enveloped ds DNA virus. What is a possible cause?
|
• Adenovirus
• If presentation was an adult - then possibly BK polyoma virus |
|
|
A young boy presents w/ a mild hemorrhagic cystitis. PCR identifies a non-enveloped dsDNA virus. What is a possible cause?
|
• Adenovirus
|
|
|
A renal transplant patient presents with an acute interstitial nephritis. PCR identifies a dsDNA virus. What is the most likely cause? What serotypes are most likely?
|
• Adenovirus, serotypes 11 & 12
|
|
|
Adenovirus: enveloped? DNA or RNA? ss or ds?
What urinary tract presentations are possible? Who does it tend to infect? |
• Adenovirus ≈ non-enveloped dsDNA virus
• Causes hemorrhagic cystitis • Commonly affects: renal transplant pts, *pediatric* bone marrow transplant pts, or healthy children [esp. boys] |
|
|
What are the unifying pathological features of HIV-associated nephropathy?
|
• Hyperplastic injury w/in the glomerulus
• Podocyte proliferation • Glomerular sclerosis • Promintent tubular dilation & interstitial inflammation |
|
|
What are the common renal afflictions faced by HIV Patients? What demographic is affected more often?
|
• HIV-associated nephropathy & Focal Segmental Glomerularnephropathy. *Must be distinguished from medication toxicity*
• More often affects African Americans |
|
|
What is the term for Igs that precipitate in the cold < 37º C and go into solution at 37ºC? What are they associated with?
|
• Cryoglobulins
• Associated w/ chronic viral infxns like HIV, hepatitis B or C |
|
|
How does cryoglobulinemia present? Who does it tend to afflict?
|
• Presents as renal disease & small vessel vasculitis
• Tends to affect pts w/ chronic viral infxs like HIV, Hep B or HepC |
|
|
Hantavirus: enveloped? DNA or RNA? ss or ds?
What family is the virus a part of? How does it present? |
• enveloped ssRNA viruses.
• Member of the Bunyavirus family • Presents as hemorrhagic fever with renal symptoms. |
|
|
Hanta virus causes an acute interstitial nephritis w/ tubular necrosis. What is the pathology due to?
|
• Damage to the vascular endothelium
|
|
|
How is Hanta virus spread?
|
Rodent contact only (aerosolization & inhalation of dried rodent urine or excreta)
|
|
|
How is Korean Hanta virus treated?
|
Ribavirin
|
|
|
A patient presents with moderate-severe illness with fever, oliguria, proteinuria, abdominal pain, and hemorrhaging. He described earlier fever, flushed face, periorbital edema, and small red dots in his throat. He also had mild headache, lumbar pain, and eye pain. What virus is possible?
|
Hanta virus.
|
|

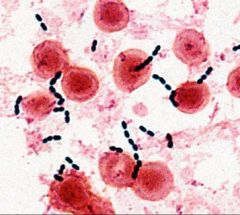
What bacteria is pictured?
• G( )? shape? • Use of oxygen? • Nutritional requirements? • Ferment ___? Catalase ( )? Oxidase ( )? Special traits? |
Enterobacteriacea
• G(-) rods • Facultative anaerobes • Simple nutritional requirements • ferments glucose & some ferment lactose • Catalase (+) • **Oxidase (-)** |
|

What is pictured? What family of bacteria have these structures?
|
• Peritrichous* flagella (*many extending from multiple places)
• Enterobacteriaceae |
|

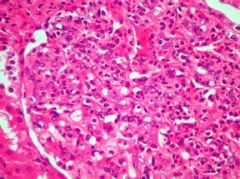
• What agar is pictured? What does it show?
• What enterobacteriaceae could be pictured on the far left? • What enterobaceriaceae species could be pictured on the far right? |
• McConkey Agar, shows the fermentation of lactose
• Left (lactose -) could be Proteus mirabillis • Right (lactose +) could be E. coli, Klebsiella pnemoniae, Enterobacter (possible Serratia marcescens) |
|
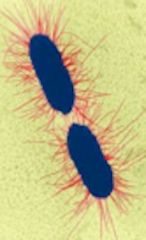
What 2 types of pili on E.coli are shown? What are they used for?
|
• P-pilus - pyelonephritis associated pilus (PAP) which binds digalactose (Gal-Gal) receptor on uroepithelial cells
• FimH - mannose-sensitive pilus: binds mannosylated proteins that line the bladder mucosa |
|

What is pictured? What bacteria is this characteristic of?
|
• Swarming (motility, colony spreading)
• Proteus mirabilis |
|

The culture of what bacteria is shown? What family is it in? What is it fermenting? Why is it distinct in reference to fermentation?
|
• Serratia marcescens
• Enterobacteriaceae • Fermenting lactose • Ferments lactose slowly (3-4 days) and produces brick-red colonies |
|

What culture is being shown? What is used in culture? What bacteria can it show?
|
• McConkey agar
• Shows fermentation of lactose • Can show E.coli, K. pneumoniae, Enterobacter, (Serratia marcescens +/-) • Test is (-) for Proteus mirabilis |
|

The opportunistic pathogen shown is called? Is G ( )? shape? Oxygen requirements? Oxidase ( )? Ferments? Nutritional requirements?
|
Pseudomonas aeruginosa
• G(-) rod • Aerobic • **Oxidase (+)** • No fermentation • Ability to adapt to minimal nutritional requirements |
|
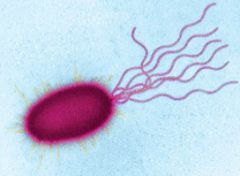
What are the virulence factors of the bacterium shown?
|
Pseudomonas aeruginosa
• Adhesins • Polysaccharide capsule (antiphagocytotic) • Endotoxin (inflammation) • Exotoxin A (tissue damage)› |
|

The culture of what bacteria is shown? G( )? Shape?
What are the four unique characteristics of its culture? |
Pseudomonas aeruginosa
• G(-) rod • Blue green colonies (pyocyanin & pyoverdin) • Grows at 42º C • Fruity aroma • mucoid - alginate slime • Fluorescence under UV light |
|
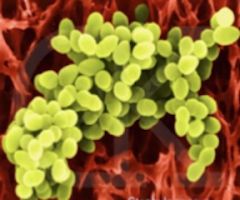
What bacteria that causes 10-20% of UTIs is shown? Shape? G ( )? Catalase ( )? Urease ( )? How can you distinguish it from another common bacteria of the same family?
|
Staphylococcus Saprophyticus
• G(+) cocci, grows in irregular clusters • Catalase (+) • Urease (+) • Can distinguish it from Staph. aureus because S. sapro is **Coagulase (-)** |
|

What test is being shown? What is it used for? How does it work?
|
Coagulase test
• it is used to distinguish b/w types of Staphylococci (S. aureus is coagulase +) • Coagulase is a protein produced that catalyzes fibrinogen --> fibrin |
|

On this culture of Staph. saprophyticus...G ( )? Shape?... What kind of hemolysis is being shown? What antibiotic is on the piece of paper in the middle of the culture?
|
• Staph saprophyticus is G(+) cocci that grow in irregular clusters
• γ- hemolysis on blood agar • Novobiocin-resistant |
|
What UTI- causing bacteria is shown? G( )? Shape? Catalase ( )? Lancefield's group ___ antigen? What makes these bacteria problematic?
|
Enterococcus faecalis & faecium
• G(+) dipplococci or short chains • Catalase (-) • Lancefields group D antigen • ***alot of drug resistance*** some are even Vancomycin resistant |
|
What bacteria of the normal flora (that often cause UTIs) is show? How does it appear on microscopy? How does it appear on blood agar? What is it resistant to?
|
Enterococci (Faecalis & faecium)
• G(+) cocci, in short chains • γ or α hemolysis on blood agar • Resistant to: 40% bile salts, 6.5% NaCl, bacitracin & optochin |
|
|
What is the Tx for acute tubular necrosis?
|
1. Avoid volume overload & hyperkalemia
2. Loop or thiazide diuretics may improve diuresis (loops may increase death, diuretics in general discouraged in critically ill) 3. Plasma ultrafiltration may be used for volume reduction in ICU pts 4. Dietary protein restriction helps prevent metabolic acidosis |
|
|
What are some of the metabolic complications of acute tubular necrosis?
|
Hyperkalemia
• Hypocalcemia • Hyperphosphatemia • Hypermagnesemia |
|
|
How do you Tx complications involving Ca+ and phosphate in acute tubular necrosis?
|
• Diet
• Phosphate binding agents to ↓ Phosphate & address hyperphosphatemia • Do NOT tx hypocalcemia in pts w/ rhadomyolysis unless symptomatic can lead to hypercalcemia |
|
|
How do you Tx complications involving magnesium in acute tubular necrosis?
|
• Tx hypermagnesemia by avoiding magnesium containing antacids & laxatives.
|
|
|
When is dialysis indicated in pts with acute tubular necrosis?
|
• Life threatening electrolyte disturbances (hyperkalemia)
• Hypervolemia (or unresponsive to diuretics) • Worsening acidosis • Uremic complications --> encephalopathy, pericarditis, or seizures |
|
|
What accounts for over 70% of the cases of interstitial nephritis?
|
• Drugs such as:
--Penicillins & cephalosporins --Sulfonamides & sulfonamide containing diuretics (most except ethacrynic acid) --NSAIDs --rifampin --phenytoin -- allopurinol -- H+pump inhibitors |
|
|
What infectious agents can cause interstitial nephritis?
|
• Streptococcal infxns
• Leptospirosis • Cytomegalovirus • Histoplasmosis • Rocky Mountain spotted fever |
|
|
What autoimmune diseases can cause interstitial nephritis?
|
• SLE
• Sjögren syndrome • Sarcoidosis • Cryoglobulinemia |
|
|
What is the Tx for interstitial nephritis?
|
• Supportive measures
• Tx underlying cause • Dialysis in 1/3 of pts • Corticosteroids may be used (methylprednisolone, prednisone) |
|
|
What does PAP do? Specifically, what does it bind to? What bacteria uses it?
|
• PAP or Pyleonephritis associated pilus binds to the di-galactose receptor on uroepithelial cells.
• Used for adhesion by E. coli |
|
|
What does FimH do? Specifically, what does it bind to? What bacteria uses it?
|
• FimH is mannose sensitive pilus: it binds the mannosylated proteins that line the bladder mucosa
• It is used for adhesion by E. coli. |
|
|
What is peritrichous? What bacteria have peritrichous ___?
|
Peritrichous refers to flagella projecting in many different directions from many different places.
• E. coli & Proteus mirabillus have peritrichous flagella |
|
|
What bacteria that is often indicated in UTIs does NOT ferment lactose and is highly motile?
|
• Proteus mirabilis does NOT ferment lactose and is highly motile due to peritrichous flagella.
• Interestingly, it often causes stones because it is Urease+ |
|
|
What does urease do? What bacteria produces it?
|
Urea --> ammonia + CO2 (makes urine more basic, smells like ammonia)
• Proteus miabilis |
|
|
What bacteria is an aerobic G(-) rod, motile (lophotrichous), oxidase +, and does not ferment anything?
|
• Pseudomonas
• Lophotrichous ≈ many flagella from the same place (horses’ tail) |
|
A 7-year-old boy is recovering from impetigo. Physical examination shows a few honey-coloured crusts in his face. The crusts are removed, and a culture of the lesion grows group A Streptococcal pyogens. He is treated with a course of antibiotics. One week later. He develops malaise with nausea and a slight fever and passes dark brown urine.
• Describe the pattern of glomerular lesion in this patient? • What is the clinical correlate of this glomerular lesion? • What is the mechanism of this renal disorder? • What laboratory features will characterize this condition? • What is the most likely outcome? |
* Proliferative. Bowman's space is very narrow & there is an increased # of cells. **Proliferation of mesangium & endothelial cells**
• Post-streptococcal glomerularnephritis • Mechanism: ---Immune complex deposition (in skin, connective tissue, joints, kidney) ---Subendothelial "HUMPS" • ASO titer (looks for streptolysin) • 90% recovery rate |
|
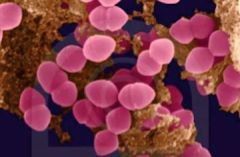
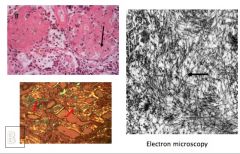
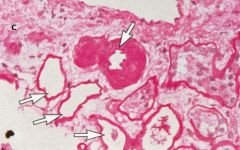
Identify some of the proliferating cells on this slide. What disease causes this?
|
• Proliferation of mesangial and endothelial cells
• Acute Diffuse Proliferative (Post-streptococcal) Glomerulonephritis |
|
A 17 year old male complains of dark urine for the past three days. He also suffers from a flu like illness for almost two weeks now. Examination reveals no abnormalities.
Urine: Red coloured urine +++++ RBC casts No proteins Blood examination: Mild increase in WBC The hematuria subsided after 3 days. The patient recovered from his upper respiratory tract infection. • What was the most likely cause of his asymptomatic hematuria? • What lab features will most likely be associated w/ the underlying renal disease? • What is the likely histological pattern in the patient's renal biopsy? |
• IgA (Berger's Disease): most common cause of asymptomatic & recurrent hematuria in adults
• Granular immunofluroescence, mesangial deposits of IgA • Histo: Proliferation of **mesAngial cells** due to IgA deposition there. • Henoch-Scherloin purpura, Liver failure, Celiac disease, rheumatoid arthritis, Reiter's disease, ankylosing spondylitis & HIV. |
|
A 79–years- old man with a history of hypertension was brought to the emergency room complaining of severe suprapubic pain associated with hematuria. On rectal examination he was found to have an enlarged prostate. He was admitted, treated for pain, and a work up for hematuria was pursued. His initial blood pressure was 200/100 mmHg, which decreased to 170/80, and subsequently to 150/82 mmHg over a period of 48hrs. The investigation of hematuria (no proteinuria) included intravenous pyelography, computerized tomography, and a surgical procedure.
1. What is the possible cause of the patient’s hematuria? 2. Describe the microscopic features of the biopsy obtained from the patient’s bladder 3. What exposures might this patient have had? |
1. Likely not related to Glomerular disease because there is no proteinuria
• Pyelonephritis (bacteria present) • Stones 2. There are epithelial cells (normally they grown in a line/layers - they line surfaces) • Abnormal growth, by definition its a tumor. • Transitional cell carcinoma. 3. Exposure to chemicals B-naphtylamine OR infection with schistosomiasis |
|
After eating cheeseburger, French fries, and ice cream for dinner one night, a 6 year old girl develops malaise, abdominal cramps, and fever. Suddenly she began to pass blood in stools and her skin showed scattered petechea developing on the extremities. Three days later she is passing a very small amount of dark urine and blood studies showed high level of BUN.
What disease does she have? What toxin causes this? What is the mechanism of the pathology? |
• Hemolytic Uremic Syndrome (HUS)
• E. coli: expresses verotoxin (also called shiga-like toxin) • Thrombocytopenia, micro-thrombi that directly damage the endothelial cells -- blood smear would show schistocytes from mechanical damage due to blockage of the vessels by microthrombi -- Uremia due to microthrombi |
|
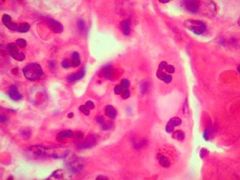
A patient presented with fatigue and back pain. Blood showed high level of high serum globulin level from the presence of monoclonal protein. X ray showed osteolytic lesions in lumbar vertebrae. Blood studies showed high levels of calcium, uric acid and BUN . Urinalysis shows Bence Jones proteins.
• What is the underlying pathology? • Why is there back pain • What is shown in the brown-stained image? |
• Multiple Myeloma (plasma cell neoplasm)
• Bone marrow tumor • Amyloid shown - from the fragments of the IgG released from the plasma cell. |
|
A 66-year old woman died of an acute myocardial infarction. At autopsy both kidneys were decreased in size with a finely granular cortical surface.
What is shown? What can you infer about the patient? |
• Hyaline arteriolosclerosis
• Chronic process due to BENIGN HTN (malignant HTN presents with onion-skinning lesions or hyperplastic arteriolosclerosis) |

