![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Formation of the TESTIS occurs in the presence of which chromosome? |
Y chromosome
|
46 XY
|
|
|
Formation of the OVARY occurs in the absence of which chromosome? And presence of which chromosome? |
Absence of Y and presence of X |
46, XY
|
|
|
At what gestational age do GONADS begin developing? |
5-6 weeks |
|
|
|
Which gene is involved in testis determination? |
SRY gene |
|
|
|
What is required for normal ovarian development? |
A second X chromosome
|
|
|
|
What structures do the Wolffian ducts develop into? |
Epididymis |
Develop IPSI-laterally, dependent on presence/absence of local hormone synthesis |
|
|
What hormone are the Wolffian ducts dependent on? |
Testosterone
|
|
|
|
What structures do the Müllerian ducts develop into? |
Fallopian tubes |
|
|
|
What structures do the Müllerian ducts develop into?
|
Fallopian tubes |
Develop IPSI-laterally dependent on local hormone presence/absence. |
|
|
What hormone are the Müllerian ducts dependent on?
|
Antimüllerian hormone - in the ABSENCE if AMH, the Müllerian ducts proliferate |
|
|
|
Where is AMH produced?
|
Sertoli cells
|
|
|
|
Which hormone is crucial in the formation of EXTERNAL genitalia? |
DHT (dihydrotestosterone)
+DHT --> male (-)DHT --> female |
|
|
|
When does DHT start to be produced? |
7-8 weeks |
|
|
|
hCH stimulates which cells to produce more testosterone in males? |
Leydig cells |
|
|
|
When is feminization of the external genitalia complete? |
14 weeks |
|
|
|
When is masculinization of the external genitalia complete? |
16 weeks |
|
|
|
What hormones/receptors mediate decent of the testes? |
Testosterone Insuline-like Ligand 3 I-like Ligand 3 Receptor: Lgr3 |
|
|
|
What are the 3 facets of Sexual Differentiation? |
1.) Gonadal Differentiation 2.) Genital Differentiation 3.) Behavioral Differentiation |
|
|
|
At what age is sexual/gender identity established? |
2.5 years old |
|
|
|
What are the 4 types of etiology for 46, XX Maculinized Female? |
1. Congenital Adrenal Hyperplasia 2. Maternal androgen excess 3. 46,XX gonadal dysgenesis 4. 46,XX true hermaphroditism |
|
|
|
What are the 3 types CAH? |
21-hydroxylase (CYP21) deficiency (90%)
11 B-hydroxylase (CYP11B1) (5%)
3 B-hydroxysteroid dehydrogenase (BHSDII) (least common) |
|
|
|
Which form of CAH is the salt-losing form? |
21-hydroxylase deficiency - Due to low aldosterone secretion - MCC endocrine neo death - Autosomal recessive - Chromosome 6p |
|
|
|
Which form of CAH is the hypertensive form? |
11 B-hydroxylase deficiency - Due to XS corticosterone and 11-deoxycorticosterone |
|
|
|
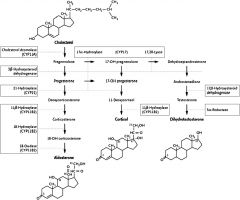
Describe the Cortisol pathway... |
|
|
|
|
Describe the mechanism of abnormal sexual differentiation with CAH |
Increased cortisol --> high ACTH --> adrenal androgens --> virilization of external genitalia )fusion of labioscrotal folds, clitoral enlargement)
normal ovaries and Mullerian ducts |
|
|
|
Clinical manifestations of untreated CAH |
- Pubic hair by age 2-4 then axillary->body->facial hair - Premature epiphyseal closure - Male habitus - Acne, deep voice, primary amenorrhea, infertility. |
|
|
|
What are the causes of Maternal Androgen Excess? |
1.) Maternal ingestion of synthetic androgens - placenta can't aromatize synthetics into estrogens
2.) Neoplasia causing T - placenta can aromatize T, thus protecting F fetus from masculinization
3.) Luteoma - makes DHT, placenta cannot aromatize DHT, so baby gets masculinized. |
Treatment is surgical correction of external genitalia abnormalities. |
|
|
Possess an "ovotestis" - testicular tubules and ovarian follicles (separately or together) |
True Hermaphroditism 46,XX |
|
|
|
What is the most common karyotype for True Hermaphroditism? |
46,XX |
|
|
|
This syndrome is assoc. w/ sensorineural deafness, pt. presents as female but fails to achieve female puberty.
Elev. gonadotropins and streak gonads = to 46,XO but lacks the congenital malformations |
Gonadal Dysgenesis (Perrault Syndrome) 46,XX |
|
|
|
What are the 7 types of etiology for 46, XX Undermasculinized Male? |
1. Complete/partial gonadal dysgenesis 2. Androgen insensitivity syndrome (complete&partial) 3. 5alpha-reductase deficiency 4. Leydig cell hypoplaisa (Sertoli cell only syndr) 5. Abnormalities of Leydig cell function 6. Isolated persistence of mullerian ducts |
|
|
|
What factors are involved in gonadal dysgenesis? |
SRY, SF-1, SOX-9, DMRT1/DMRT2, DAX-1, WNT4
Mutation of these factors can block the differentiation of the bipotent gonad into testis. |
This can result in either complete or partial gonadal dysgenesis |
|
|
What is Swyer Syndrome? |
Complete gonadal dysgenesis (SRY Deletion) |
|
|
|
What other disease can gonadal dysgenesis be confused with? Why? |
Leydig cell hypoplasia In Swyer syndrome they have a +cervix and uterus, +mullerian system. |
Always check that they have a cervix&ut, b/c they could present similarly but actually be Leydig cell hypoplasia, and be missing cervix&ut |
|
|
Describe what you see with Complete gonadal dysgenesis |
No T, so female external genitalia. Persistence of mullerian ducts due to Sertoli cell AMH. |
|
|
|
Describe what you see with Partial gonadal dysgenesis |
Partial masculinization of external genitalia, partial development of wolffian ducts cut to diminished testicular androgens and AMH. |
|

