![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
65 Cards in this Set
- Front
- Back
|
Signs of intraneural injection
|
- high injection pressures
- pain on injection - low current thresholds when using a nerve stimulator - failure to of the evoked contractions to disappear at the start of LA injection - swelling of the nerve if visualised with US (Note, recent studies suggest that intraneural injection is not always painful, not always difficult, and not always dangerous. However, it should still be avoided) |
|
|
INTERSCALENE BLOCK
Definition |
Regional Anaesthetic technique to anaesthetise the brachial plexus between the scalene muscles
|
|
|
INTERSCALENE BLOCK
Indications and Contraindications |
INDICATIONS:
Intraoperative and postoperative anaesthesia and analgesia of the shoulder Mobilising and physiotherapy for the shoulder CONTRAINDICATIONS Specific to Interscalene Block - Contralateral phrenic nerve palsy - Severe COPD or respiratory impairment Common to regional anaesthetic techniques - Patient refusal - Local anaesthetic allergy - Coagulopathy - Local infection |
|
|
INTERSCALENE BLOCK
Anatomy |
Interscalene block aims to anaesthetise C5-C7 nerve roots of the brachial plexus that lie in the interscalene groove (between scalenus anterior and scalenus medius)
Relevant Landmarks - Lateral border of SCM - Level of C6 (cricoid cartilage) Roots of brachial plexus exit intervertebral foraminae and lie - Posterior to the vertebral artery as it runs in the transverse process gutter - Posterior to the phrenic nerve (the phrenic nerve runs along the anterior wall of scalenus anterior) - Superior to apex of pleurae (apices of pleurae lie 4cm above clavicle) - Superior and posterior to stellate ganglion (sympathetic ganglion on C8 and T1) |
|
|
INTERSCALENE BLOCK
Technique - Traditional |
Position
- Patient supine with head neutral or turned away from site block - Can also be lateral with operative side up Traditional Placement - Identify lateral border of SCM at level of C6, lateral to the SCM lies the scalenus anterior and medius muscles and the interscalene groove. - Insert needle perpendicular to skin or in a slightly caudal direction - If using a nerve stimulator – set at 0.5-0.8mA expecting to see activation of o Pectoralis muscle o Deltoid muscle o Triceps muscles o Biceps muscle o Any twitch of the hand or forearm o NOT trapezius or diaphragm - Brachial plexus is shallow with the interscalene approach, expect to contact at approx 1-2cm Injection Small volume, high concentration block Typically 10-15mL 0.75% Ropivicaine, or 1:1 1%Lignocaine and 0.75% Ropivicaine. Can also use 0.5% Bupivicaine |
|
|
INTERSCALENE BLOCK
Technique - US Guided |
Position
- Patient supine with head neutral or turned away from site block - Can also be lateral with operative side up USS guided - Place on neck in axial oblique plane o Can commence medially at trachea at level of C6 and move laterally until interscalene groove is identified o Alternative, commence supraclavicular position, identify subclavian artery and trunks of brachial plexus and move superiorly unril interscalene groove is identified - Identify C5 – C7 Nerve roots in interscalene groove - In plane approach from posterior aspect with needle (via SM) Injection Small volume, high concentration block Typically 10-15mL 0.75% Ropivicaine, or 1:1 1%Lignocaine and 0.75% Ropivicaine. Can also use 0.5% Bupivicaine |
|
|
INTERSCALENE BLOCK
Draw the sonoanatomy |
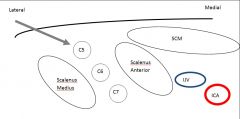
|
|
|
INTERSCALENE BLOCK
Complications |
Complications
Specific - Phrenic nerve palsy - Horner’s syndrome - Pneumothorax - Epidural injection - Intrathecal injection Common to regional anaesthetic techniques - Incorrect injection and needle placement o Intravascular Vertebral arteries, IJV, ICA o Intramuscular injection SCM, SA, SM o Intraneural injection - Inadequate Block/Failed block - Local anaesthetic toxicity - Haematoma - Infection |
|
|
SUPRACLAVICULAR BLOCK
Definition |
Supraclavicular block involves local anaesthetic blockade of the brachial plexus at the level of the divisions
|
|
|
SUPRACLAVICULAR BLOCK
Indications and Contraindications |
The supraclavicular block covers the entire upper limb except for the shoulder which is better covered by an interscalene block or by supplementing the supraclavicular block with a superficial cervical plexus block
Contraindications: Absolute - Patient refusal Relative - Outpatient procedure - Significant respiratory disease |
|
|
SUPRACLAVICULAR BLOCK
Anatomy |
Structures:
1st Rib Brachial Plexus Subclavian Artery Cupola of lung At the supraclavicular level the brachial plexus lies ‘cephaloposterior’ to the subclavian artery |
|
|
SUPRACLAVICULAR BLOCK
Technique |
The classical approach involves insertion of the needle in the middle of the clavicle, 1 cm above the clavicle (or just lateral to palpation of the subclavian artery in the supraclavicular fossa). The needle is directed caudally parallel to the floor and medial direction is avoided in order to minimize risk of injury to lung.
On ultrasound the brachial plexus is visualized as a ‘bunch of grapes’ lateral to the subclavian artery. The number of nerves varies depending on the exact division from trunks to anterior and posterior divisions (three to six hypoechoic circles are common). Injection: 15 – 20 mls of local anaesthetic can be injected. Depending on need (or not) for akinesis, varying strengths of ropivacaine can be used. |
|
|
SUPRACLAVICULAR BLOCk
Complications |
Complications:
• The most important is pneumothorax which has an incidence of 0.5-5% depending on user experience • Phrenic Nerve Block occurs in 30-50% of patients • Subclavian artery puncture – usually managed conservatively |
|
|
SUPRACLAVICULAR
Sonoanatomy |

|
|
|
FEMORAL NERVE BLOCK
Definition |
Regional anaesthetic technique to anaesthetise the femoral nerve with an anterior approach
|
|
|
FEMORAL NERVE BLOCK
Indications and Contraindications |
Indications:
Intraoperative and/or postoperative anaesthesia/analgesia of the hip, anterior thigh or knee (anterior aspect only) Mobilisation/physiotherapy of the hip and knee (e.g post TKJR for mobilisation) Fractures of the hip and femur (caution compartment syndrome with femoral fracture) Contraindications Specific - Previous femoral bypass surgery Common to regional anaesthetic techniques - Patient refusal - Local anaesthetic allergy - Coagulopathy - Local infection |
|
|
FEMORAL NERVE
Anatomy |
Femoral nerve formed from anterior rami of L2-L4 from lumbar plexus
Supplies - Motor to quadriceps femoris (knee extension) - Sensory to anterior thigh Lies lateral to femoral artery vein, outside of femoral sheath in inguinal area. Lies deep fascia lata and fascia iliaca, superficial to iliacus muscle |
|
|
FEMORAL NERVE BLOCK
Technique |
Traditional
- Identify inguinal ligament from pubic tubercle to ASIS - Identify femoral artery below inguinal ligament (approx 2cm) - Insert needle lateral to artery (palpating artery at all times), may feel 2 “pops” through fascia lata and fascia iliaca, inject - If paraesthesia encountered, withdraw needle and inject Nerve stimulator technique - Landmarks as for traditional technique - Stimuplex needle 50mm - 0.5mA - Advance needle watching for knee extension (quads activation) - Inject Ultrasound technique - High frequency probe (>7Hz) placed below and in line with inguinal ligament - Identify femoral vessels - Locate femoral nerve lateral to femoral artery (may indistinct and difficult to define) - In plane or out of plane approach acceptable - Insert needle toward femoral nerve Injection High concentration, low volume e.g. 10-15mL 0.75%ropivicaine |
|
|
FEMORAL NERVE BLOCK
Ultrasound technique and sonoanatomy |
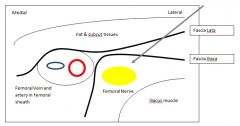
Ultrasound technique
- High frequency probe (>7Hz) placed below and in line with inguinal ligament - Identify femoral vessels - Locate femoral nerve lateral to femoral artery (may indistinct and difficult to define) - In plane or out of plane approach acceptable - Insert needle toward femoral nerve Injection High concentration, low volume e.g. 10-15mL 0.75% ropivicaine |
|
|
FEMORAL NERVE BLOCK
Complications |
Intravascular injection – femoral vein or artery
Haematoma Intraneural injection Infection Failed/inadequate block |
|
|
FASCIA ILIACA BLOCK
Definition |
Triple block of the anterior nerves of the thigh
|
|
|
FASCIA ILIACA BLOCK
Indications and Contraindications |
Indications:
Leg surgery Knee examination Femoral fracture Muscle biopsy including for MH Contraindications: As per regional blocks Previous Fem pop bypass |
|
|
FASCIA ILIACA BLOCK
Anatomy |

|
|
|
SCIATIC NERVE BLOCK
Definition |
Local anaesthetic blockade of the Sciatic Nerve
|
|
|
SCIATIC NERVE BLOCK
Indications and Contraindications |
Indications:
Anaesthesia for lower limb surgery in combination with femoral, saphenous, LCFN etc Analgesia for ankle/tibial fractures preoperatively/transport of the injured patient Distal amputation surgery Contraindications: General Specific: possibility of compartment syndrome (relative) |
|
|
SCIATIC NERVE
Anatomy |
Formed from nerve roots of L4-S3
Also can be thought of as two nerves running together: • Tibial Nerve (medial) – Ventral branches of L4-S3 ventral rami • Peroneal Nerve (lateral) – Dorsal branches of L4-S3 ventral rami The nerve roots come together on the lateral anterior aspect of the sacrum and the plexus lies anterior to the piriformis as it exits the pelvis inferiorly. The posterior cutaneous nerve of the thigh and the sciatic nerve run together at this point. The sciatic nerve runs deep to gluteus maximus and divides into its tibial and peroneal nerve components superior to the popliteal fossa (although the point at which it divides is variable). |
|
|
SCIATIC NERVE BLOCK
Technique |
Labat technique:
the patient is positioned laterally (Recovery position) with the side to be blocked superior. A line is drawn from the PSIS to the middle of the great trochanter. A second line is drawn from the GT to the Sacral Hiatus. A third line is drawn perpendicular from the midpoint of the PSIS/GT line in a mediocaudal direction. This point that transects the GT/SH line marks the needle insertion site. Skin depth of needle: 5-10cm Largest nerve in the body (20mm) - implications for speed of onset • Paresthesia?!)(&^ • Nerve Stimulator – Contraction of foot, calf or hamstrings is acceptable Twitches: Tibial component - plantar flexion of the foot (optimal) Common peroneal component - eversion of the foot (withdraw needle and aim more medially) Gluteal muscles - direct stimulation; needle too shallow • U/S: curved, low frequency probe (due to depth required) IP or OOP Difficult to visual nerve and keep tip of needle in plane Often need two needle positions (medial and lateral) to get adequate circumferential spread LA DOSE: 15-30mL (but take care with maximum dosage if using in combination with femoral or lumbar plexus block) |
|
|
SCIATIC NERVE BLOCK
Complications |
As for general regional risks
|
|
|
LUMBAR PLEXUS BLOCK
Definition |
Regional anaesthetic technique to anaesthetise the lumbar plexus at the anterior rami via the posterior approach
|
|
|
LUMBAR PLEXUS BLOCK
Indications and Contraindications |
Indications
Intraoperative and/or postoperative anaesthesia and/or analgesia of the hip and anterior thigh Differentiation of chronic pain from hip and knee Physiotherapy and Mobilisation of painful hip joint post hip replacement Contraindications Common to Regional anaesthesia - Refusal - Local infection - Coagulopathy (risk of epidural/intrathecal injection) - Local anaesthetic allergy |
|
|
LUMBAR PLEXUS
Anatomy |
Lumbar plexus formed from anterior rami of L1-L4
- L1 forms ilioinguinal and iliohypogastric nerves - L1 and L2 forms genitofemoral nerve - L2 and L3 forms lateral cutaneous nerve of thigh - L2-L4 forms femoral and obturator nerves Psoas muscles originates from transverse processes of lumbar vertebrae. Nerve roots of lumbar plexus are embedded in psoas muscle immediately and divide into anterior and posterior rami within the psoas muscle. |
|
|
LUMBAR PLEXUS BLOCK
Technique |
Technique
Consent and timeout, appropriate equipment, assistance and monitoring. Nerve-stimulator technique Poition: Lateral with leg flexed and operative side up Needle: stimuplex, 22g, 15cm Landmarks: - Palpate iliac crests and determine Tuffier’s Line (intercristal line corresponds to L3/4) - Palpate PSIS - Draw line from PSIS to Tuffier’s Line - Insert needle perpendicular to skin 1/3 distance from Tuffier’s line OR insert needle approx 4cm from midline on Tuffier’s line - Nerve stimulation set at 0.5-1mA - May hit transverse process of L5 (around 5-8cm depth) o Walk up off transverse process in cephalad direction 1-3cm - Look for activation of quadriceps (knee extension, “dancing patella”) Injection High Volume, Low Concentration block – 15-30mL of local anaesthetic (e.g 0.75% Ropivicaine) |
|
|
LUMBAR PLEXUS BLOCK
Complications |
Specific
- Epidural injection - Intrathecal injection Common - Block failure/inadequate block - Haematoma - Local anaesthetic toxicity - Infection - Intravascular/intraneural injection |
|
|
SACRAL PLEXUS BLOCK
Definition |
The Sacral Plexus Block involves local anaesthetic blockade of the nerves arising from L4,L5,S1,S2,S3
This blocks the sciatic nerve (including all branches), the pudendal nerve. |
|
|
SACRAL PLEXUS BLOCK
Indications and Contraindications |
Indications:
Sacral plexus block can be used for regional anaesthesia/analgesia of the lower limb including leg, knee or foot. It can also be used in combination with a femoral nerve block (or 3:1 block) to provide anaesthesia to the entire lower limb. The well defined space also provides for catheter insertion for ongoing analgesia. Contraindications: Refusal Local infection Coagulation defects Lower limb nerve disease (relative) Acute injury compatible with compartment syndrome (relative) |
|
|
SACRAL PLEXUS BLOCK
Anatomy |
Anatomy:
The sacral plexus is formed by the lumbosacral trunk (L4/L5) joining with the S1,S2 and S3 nerve roots to form the sacral plexus. It sits on the piriformis posteriorly in the pelvis. |
|
|
SACRAL PLEXUS BLOCK
Technique |
Technique: Nerve Stimulator
• Positioning is lateral decubitus, side to be blocked should be up (same position as for classical subgluteal approach) • Lower leg should be extended straight whilst target leg should be flexed at knee and hip • Landmarks: The posterior superior iliac spine (PSIS) and the lowest point of the ischial tuberosity (IT). A line is drawn joining these points and the insertion point lies on this line ~ 6 cm (3 fingerbreadths) inferior to the PSIS. (This should be inferior to the Posterior inferior iliac spine but if not, simply walk of it caudally) • Using Nerve stimulation either plantarflexion or dorsiflexion of the ankle/foot should be attained at 2 mA to achieve correct placement and then maintained at 0.5 mA prior to injection when 1 ml LA should terminate movement Injection: 15 – 20 mls LA should be sufficient and a single injection should be sufficient at this level |
|
|
ANKLE BLOCK
Definition Indications and Contraindications |
Block of 5 nerves of the feet
Indications Surgery to toes and feet Contraindications As per any regional technique |
|
|
ANKLE BLOCK
Anatomy |

|
|
|
ANKLE BLOCK
Technique |
Saphenous n
Blocks postero-medial part of dorsum of foot Superficial infiltration around long saphenous vein anterosuperior to medial malleolus Tibial n Needle entry medial to Achilles tendon or lateral to posterior tibial artery at upper border of medial malleolus Determine depth with paraesthesia, nerve stimulator or 1 cm superficial to tibia Alternatively infiltration either side of artery behind medial malleolus Blocks sole, plantar surface of digits Deep peroneal n Needle entry between extensor hallucis longus and tibialis anterior tendons or lateral to anterior tibial artery Blocks first web space and short toe extensors Superficial peroneal n Superficial infiltration from lateral border of tibia to upper part of lateral malleolus Blocks dorsum of foot and toes except first web space Sural n Superficial infiltration from Achilles tendon to lateral malleolus Blocks lateral side of foot and fifth digit Sedation for pain Start with deep blocks to avoid deformation of superficial anatomy. Consider NS for deep peroneal and posterior tibial Injection High volume necessary for all nerves – 20mls of 0.5%, and 2% lignocaine |
|
|
SUBTENON
Definition |
Regional anaesthetic technique to produce anaesthesia and akinesia of the orbital globe by an episcleral injection
|
|
|
SUBTENON
Indications and Contraindications |
Indications
Intraocular surgery e.g. - Cataract extraction and intraocular lens insertion - Trabeculectomy - Vitrectomy - Strabismus surgery Contraindications Penetrating eye injury Disruption of the scleral surface and tenon capsule - Scleromalacia - Staphyloma - Previous scleral surgery - Previous subtenon block in that quadrant |
|
|
SUBTENON
Anatomy |
Anatomy
Tenon capsule - Elastic white connective tissue layer - Deep to conjunctiva - Encapsulates sclera - Merges with conjunctiva approx 1mm from limbus - Extends posteriorly to attach to fibrous ring around optic nerve Subtenon space - Potential space between tenon capsule and sclera |
|
|
SUBTENON
Technique |
Equipment
- subtenon cannula (flat, blunt and curved) - Lid retractors - Moorefield’s forceps - Wescott spring scissors Position - Supine, patient looking “up and out” Topical local anaeshetic drops to eye - 1-2 drops of oxybuprocaine 1% Prep eye with iodine antiseptic Place lid retractors Inferonasal quadrant - Grasp conjunctiva and tenon capsule with moorefield’s forceps - Make small incision with wescott spring scissors - Enlarge incision and form tract by inserting scissors closed and gently opening in subtenon space to blunt dissect anterior adhesions between sclera and tenon capsule - Insert subtenon cannula - Inject solution into subtenon space o Solution will progress to retrobulbar and then extraconal space with volume and time Injection 4-6mL 10mL solution - 2mL 10% lignocaine = 2% lignocaine - 8mL 0.75% Ropivicaine = approx 0.6% ropivicaine - Hyalase 30 units/mL To get Hylase 30units/mL - Take 1 ampoule of hyalase (1500 units) - Reconstitute in 10mL (of 10%Lignocaine) - Take 2mL of solution = 300 units - Dilute to 10mL (i.e add 8mL 0.75% ropivicaine) |
|
|
SUBTENON
Complications |
Complications
Subconjunctival injection Inadequate anaesthesia/akinesia Subconjuntival haemorrhage Pain Globe perforation (rare) |
|
|
RETROBULBAR
Definition |
Retrobulbar Nerve Block is an eye block in which local anaesthetic is injected intraconally at low volume to attain anaesthesia and akinesis of the eye
|
|
|
PERIBULBAR
Definition |
Peribulbar Nerve Block is an eye block in which local anaesthetic is injected extraconally with higher volume to attain anaesthesia and akinesis of the eye
|
|
|
RETROBULBAR AND PERIBULBAR
Indications and Contraindications |
Indications:
In Surgery for corneal, anterior chamber or lens procedures Contraindications: • Child • Refusal or uncooperative patient • Infected orbit • Uncontrolled body movements or unable to lie flat (Parkinson’s, severe COAD) • Uncontrolled sneezing or coughing • Serious (poorly controlled) psychiatry problems |
|
|
RETROBULBAR AND PERIBULBAR
Anatomy |
The orbit is an irregular four shaped pyramid with its apex posteromedially and its bases forming the cornea.
All the nerves to the globe (motor and sensory) run within the cone posteriorally aside from the trochlear nerve (superior oblique muscle) and the nerve to orbicularis oculi (Temporal and Zygomatic branches of facial nerve) Sensory nerves to the upper and lower lids and conjunctiva include extraconal components from ophthalmic and maxillary nerves which are better anaesthetized with pre-septal local anaesthetic (topical conjunctival or eyelid sharp injection). The main arterial supply to the orbit and globe is via the ophthalmic artery (a branch of the internal carotid artery). The artery runs with the optic nerve proximally but then travels medially to sit on top of the medial rectus travelling anteriorly Venous drainage is via superior and inferior ophthalmic veins |
|
|
RETRO/PERIBULBAR BLOCK
Technique |
• The patient is instructed to look directly ahead (still)
• A 27g 31 mm sharp beveled needle is inserted at the inferolateral border of the bony orbit and directed towards the apex of the orbit • A pop may be appreciated as the needle penetrates the bulbar fascia • Following careful aspiration 2-4 mls of local anaesthetic is injected • 5-10 minutes should be allowed prior to commencement of surgery to prevent operation on a patient with a haematoma, gentle pressure to lower IOP can be applied in this time Peribulbar Block technique differs in that once the equator of the globe is passed the needle is advanced along the base of the orbit instead of angling up and in Perhaps a shorter needle can be used eg 25 mm 25 g sharp needle Injection: 2-4 mls Retrobulbar 6-10 mls Peribulbar +/- medial canthus injection 8 mls of 0.75% ropivacaine with 2 mls of 2% lignocaine in 10 mls Alternatively a mix of 5 mls 1% ropivacaine 5 mls 2% lignocaine in 10 mls |
|
|
RETRO/PERIBULAR
Complications |
Local:
Retrobulbar Haemorrhage Optic Nerve Injury Risk Factors Small Orbit Needle length >31 mm Patient advised to look up and inwards (moves Optic N. medial Lateral) Globe Perforation Risk Factors: Globe (Axial) length >26 mm Posterior Staphyloma (outpouching & more common in long axial length) Enophthalmos Repeated injection Previous Scleral buckling Previous surgery Junior proceduralist Extraocular muscle damage (IR most common permanent injury) Chemosis (conjunctival oedema) Ecchymosis (subconjunctival haemorrhage) Systemic: Local anaesthetic toxicity (secondary to vascular injection) Oculocardiac reflex Total Spinal Anaesthesia secondary to subarachnoid injection (around the optic nerve) |
|
|
CAUDAL BLOCk
Definition |
Regional anaesthetic technique to deliver an epidural injection via the sacrococcygeal membrane
|
|
|
CAUDAL BLOCK
Indications and Contraindications |
Indications
Analgesia to surgery below the umbilicus (block to T10) - Circumcision - Orchidopexy - Hernia repair - Herniotomy Can be used for abdominal surgery in neonates Management of chronic sacral or facet join pain Contraindications Absolute - Patient refusal - Local infection - Coagulopathy - LA sensitivity Relative - Hypovolaemia - Haemodynamic instability - Pre-existing neurological deficit - Abnormal sacral/spinal anatomy |
|
|
CAUDAL BLOCK
Anatomy |
PSIS = S2
Sacral Hiatus =S5 - Formed due to failure of fusion of the laminae of S5 - Lies between sacral cornu - Covered by sacrococcygeal membrane Spinal cord ends at - L1 in adults - L3 in children Dural sac ends at S2 in adults and children |
|
|
CAUDAL BLOCK
Technique |
Pre-block
- Consent, time out - Equipment, assistance, monitoring Position - Lateral position - Can be prone for adults Aseptic technique (full aseptic technique for all central neuraxial techniques according to college guidelines) Identify sacral hiatus - Palpate PSIS - Draw line between PSIS - Draw equilateral triangle in caudad direction - Apex of triange lies sacral hiatus between sacral cornua Insert 22g needle or cannula at 30 degree angle to skin Note loss of resistamce once sacrococcygeal membrane penetrated then flatten needle and advance slightly in epidural space Aspirate for blood/CSF Injection 1mL/kg 0.25% Levobupivicaine or 0.2% Ropivicaine Adjuvants – opioids, ketamine, clonidine, adrenaline |
|
|
CAUDAL BLOCk
Complications |
Specific
- Incorrect injection o Intrathecal --> apnoea o Intravascular --> arrhythmia o Subcutaneous o Periosteal - Epidural haematoma - Nerve root Injury - Hypotension - Urinary retention (particularly with opioids) Common - Block failure |
|
|
TAP BLOCK
Definition |
Regional anaesthetic technique to block the nerves suppling the anterior abdominal wall with an approach within the transversus abdominis plane
|
|
|
TAP BLOCK
Indications and Contraindications |
Indications
Surgery to the anterolateral abdominal wall. NB TAP block does not block sensation to the viscera Contraindications Common - Patient refusal - Local sepsis - LA sensitivity - ?coagulopathy |
|
|
TAP BLOCK
Anatomy |
Nerves from anterior rami of T7-L1 supply skin, muscles and parietal peritoneum of anterolateral abdominal wall.
Travel Lateral to medial in the plane between transersus abdominis and internal oblique. Midway through course, give off branches that pierce the internal oblique to and travel lateral in the plane between the internal and external oblique to supply the lateral wall. Remaining nerves continue in the TA plane towards the rectus abdominis |
|
|
TAP BLOCk
Technique |
Traditional
- Identify triangle of Petit o Bordered by iliac crest (inferior), latissimus dorsi (posterior), external oblique (anterior) o Floor = fascia of external and internal oblique - Needle (blunt e.g 18g tuohy needle) insertion in triangle of Petit - 2 “pop” technique - Inject 20ml local anaesthetic - Repeat bilaterally for midline incisions USS guided - Place USS probe in transverse plane in midaxilllary line midway between the costal margin and iliac crest. - Identify external oblique, internal oblique and transversus abdominis. - Insert needle in an in plane approach until needle tip reaches plane between internal oblique and transversus abdominis - Inject LA watching for expansion of the plane in a lentiform shape. Injection Volume block 40mL of LA e.g 2x20mL 0.5% Ropivicaine |
|
|
TAP BLOCK
Complications |
Specific
- Intraperitoneal injection o Bowel, splenic, hepatic injury Common - Block failure/inadequate block - Intravascular injection - Intramuscular injection - LA toxicity - haematoma |
|
|
COELIAC PLEXUS BLOCK
Definition Indications Contraindications |
Coeliac Plexus Block is a regional block performed using landmarks or (more reasonably) under fluoroscopic guidance usually in the context of chronic pain.
Indications include: • Acute: Post-operative pain relief for abdominal visceral surgery (particularly effective when combined with intercostal blocks) • Chronic (non-malignancy): eg chronic pancreatitis • Chronic (malignancy) eg pancreatic cancer Contraindications include: General: • Uncooperative or no consent • Coagulopathy • Sepsis • Local Infection • Peripheral Nerve Injury Specific: • Aortic Aneurysm |
|
|
COELIAC PLEXUS
Anatomy |
The Coeliac plexus is the largest of three sympathetic plexuses (the others being the cardiac plexus and the hypogastric plexus)
The Coeliac plexus is supplied by the greater, lesser and least splanchnic nerves. Those nerves arise from T5 to T12. The splanchnic nerves traverse the mediastinum and pass through the cura of the diaphragm above L1 and synapse in the coeliac plexus Anatomically, the coeliac plexus block can be performed either posterior to the crura of the diaphragm or anteriorly. |
|
|
COELIAC PLEXUS
Technique |
Posterior approach:
Having obtained consent, the patient should be positioned in the lateral or prone position The skin should be treated with antiseptic preparation and drapes applied Fluroscopy should be utilized to maximize safety The landmarks for the block are: • The T12 and L¬1 spinous processes which should be identified by palpation +/- fluoroscopy • Lines should be drawn 7-8 cm parallel to the spine and a mark made where these lines cross the twelfth rib • Another mark should be made between the T12 and L1 spinous process • A triangle should be drawn joining the two lateral markings over the twelfth ribs and between the twelfth rib markings and the T12 spinous process • The skin entry is marked by the lateral markings and the needle is directed at a 45 degree angle towards the midline to contact the L1 vertebral body (8-9 cm) • The needle is then withdrawn to skin and redirected to walk off the front of the vertebral body (a further 1-2 cm) where LA is injected • If aortic pulsation is palpated through the needle it should not be advanced further Local Anaesthetic (eg 0.5% levobupivacaine 10 mls each side) or Neurolytic solution (5 mls 6% aqueous phenol) should be injected depending on the indication |
|
|
COELIAC PLEXUS BLOCk
Complications |
• Neuraxial Blockade, (epidural or spinal)
• Aortic puncture in 1/3 (without fluoro) • Paraplegia has been reported (thought to be secondary to vasospasm of the artery of Admakiewicz) |

