![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
While excreting wastes, the essential components of glomerular filtrate need to be saved. How is this achieved?
Where is mass reabsorption? |
Tubular reabsorption.
Mass reabsorption of glomerular filtrate (2/3) in the proximal tubule. |
|
|
What is the primary role of the proximal tubule?
|
Reabsorb most of the filtered water and solutes (important for regulation of ECF volume)
|
|
|
What is the equation for the rate of flow in the proximal tubule?
|
![GFR- reabsorption [+secretion] = rate of flow in LOH](https://images.cram.com/images/upload-flashcards/11/15/81/5111581_m.png)
GFR- reabsorption [+secretion] = rate of flow in LOH
|
|
|
What are the major solutes that contribute to isotonic reabsorption in the proximal tubule?
What is the effect of distance from glomerulus on inulin concentration ratio (TF/P) |
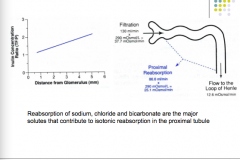
Sodium, chloride, and bicarbonate
|
|
|
How does sodium reabsorption occur?
|
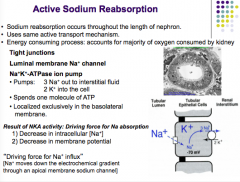
Occurs throughout the length of the nephron (active transport mechanism = consumes energy, MAJORITY OF O2 consumed by kidney)
Na-K ATPase pumps out 3Na+ into interstitium and brings in 2 K+ ions (1 molecule ATP) --> decrease in intracellular Na+ concentration and membrane potential brings in a sodium ion through the luminal Na+ membrane channel. |
|
|
What is this passive diffusion of sodium into the luminal channel also provide the energy for?
|
Reabsorption of other solutes from lumen of proximal tubule (bicarbonate, glucose, AA, organic acids)
|
|
|
True or false.
Na+ is the only quantitatively important substance whose transport is directly coupled to metabolic energy in proximal tubule. What two types of channels is the import of sodium tied to? |
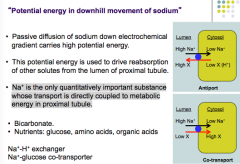
True.
Antiport and cotransport |
|
|
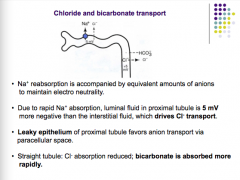
What is sodium reabsorption accompanied by? Why?
What would a leaky epithelium cause? What is absorbed in the STRAIGHT tubule? |
|
|
|
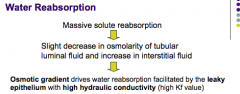
What is the pathway of water reabsorption and how it affects the osmotic gradient?
|
|
|
|
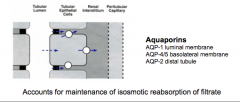
What accounts of the maintenance of isosmotic reabsorption of filtrate? Where are they located (3)?
|
|
|
|
What forces are involved in capillary uptake of fluid from interstitial fluid?
What are the three forces? What does each favor? Another name for these forces? |
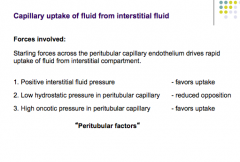
|
|
|
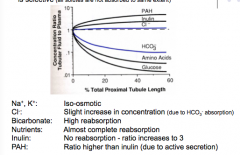
True or false.
Reabsorption from proximal tubule is iso-osmotic, but it is selective. What does this mean? |
True
All solutes are not absorbed to the same extent. |
|
|
What is the absorption of each?
Na, K, Cl, Bicarbonate, nutrients, inulin, PAH |
|
|
|
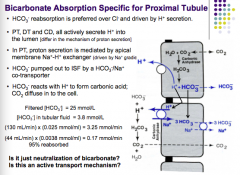
What is HCO3 preferred over an what is its reabsorption driven by?
What three components all secrete H+ into lumen? What is proton secretion mediated by in the PT? How is HCO3 pumped out to ISF? What does HCO3 react with to form carbonic acid? |
|
|
|
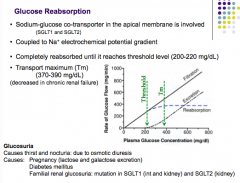
What is the transporter for glucose reabsorption?
What is it coupled to? Does it have a threshold? What are some causes of glucosuria? Symptoms? |
|
|
|
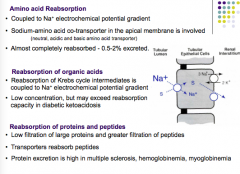
What is AA reabsorption coupled to? Is it almost completely reabsorbed?
How are organic acids reabsorbed? How are proteins and peptides reabsorbed? When is protein excretion high? |
|
|
|
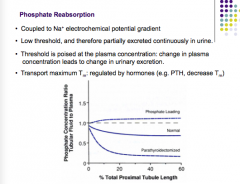
How is phosphate reabsorbed?
Does it have a low threshold? Is it partially excreted continuously in urine? What controls threshold? What regulates Tm? |
|
|
|
Cl- is passively reabsorbed due to what two things?
How much is reabsorbed due to active transport of HCO3-? |
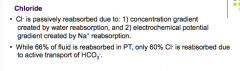
1. Concentration gradient created by water reabsorption.
2. Electrochemical potential gradient created by Na+ reabsorption. |
|
|
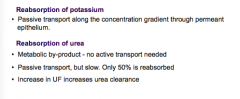
How is potassium reabsorbed?
How is urea reabsorbed? What increased urea clearance? |
|
|
|
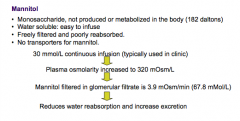
Substances that are freely filtered, but not reabsorbed, can increase what?
What is the clinical significance of this? |
Osmolarity and diuresis (excessive water excretion)
Reduction of intracranial and intraocular pressure, promote excretion of toxins, edema. |
|
|
What is a substance that can reduce water reabsorption and increase excretion? How (pathway)?
|
|
|
|
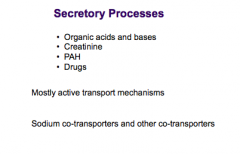
What substances are secreted in PT? How? What transporters?
|
|

