![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
Preload, afterload in different cardiac diseases
|
Preload, afterload in different cardiac diseases (very important for Board examination): Preload (volume work) is increased in valvular insufficiency (e.g., aortic insufficiency, mitral insufficiency, tricuspid insufficiency) and in left-to-right shunt (e.g., VSD). Cardiac chambers are dilated. Management: reduce preload Afterload (pressure work) is increased in valvular stenosis (e.g., aortic stenosis, mitral stenosis) andcoarctation oftheaorta. Management: reduce afterload. Afterload is decreased in high-output failure (e.g., large systemic arteriovenous fistualas) which has normal myocardial function, decrease peripheral vascular resistance, and increase myocardial contractility
|
|
|
Maximum decline of pulmonary pressure a
|
Maximum decline of pulmonary pressure after birth:first 2-3 days of life,decline occurs mostly in first hour of birth.
|
|
|
Which organ gets maximum blood supply in fetal life from cardiac output?
|
Which organ gets maximum blood supply in fetal life from cardiac output? Placenta (65%). All other organs get 35%.
|
|
|
Most important factor causing pulmonary vasoconstriction?
|
Most important factor causing pulmonary vasoconstriction? Hypoxia. Other factors are acidosis, sepsis (group B Strep,
which releases thromboxane A2, which causes puhnonary vasoconstriction |
|
|
Time to close functionally:
|
Time to close functionally:
Foramen ovale: by 3 months ofage. Ductus arteriosus: by10-15 hours, but anatomic obliteration ofductus does not occur until after first week oflife |
|
|
Most important factor in ductal closure of neonate:
|
Most important factor in ductal closure of neonate: oxygen. (Hyperoxia closes duct, hypoxia opens it.)
|
|
|
Factors closing duct
|
Factors closing duct indomethacin, hyperoxia, alkalosis.
|
|
|
Factors opening duct:
|
Factors opening duct: hypoxia, prostaglandin E1, S, acidosis.
|
|
|
Which heart disease is most common in high altitudes
|
Which heart disease is most common in high altitudes? PDA.
|
|
|
When first child has congenital heart disease, what is chance that 2nd child will also?
|
When first child has congenital heart disease, what is chance that 2nd child will also? 2-6%.
|
|
|
When two siblings have congenital heart disease, what is chance that 3rd child will also?
|
When two siblings have congenital heart disease, what is chance that 3rd child will also? 20-30%.
|
|
|
Most common cause of congenital heart disease
|
Most common cause of congenital heart disease: unknown, but genetics factor play animportant role.
|
|
|
Which heart disease is most common in high altitudes?
When first child has congenital heart disease, what is chance that 2nd child will also? |
Which heart disease is most common in high altitudes? PDA.
When first child has congenital heart disease, what is chance that 2nd child will also? 2-6%. |
|
|
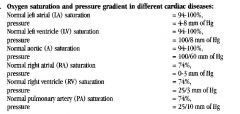
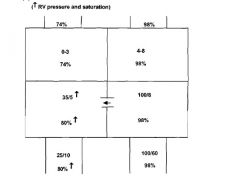
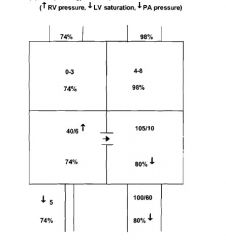
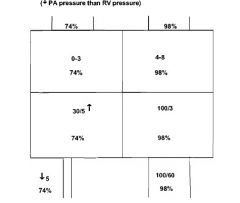
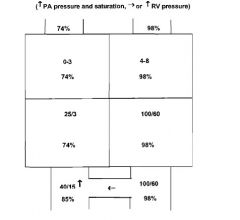
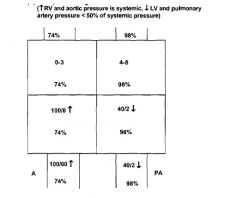
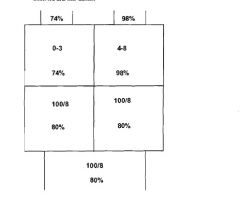
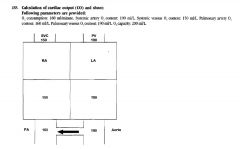
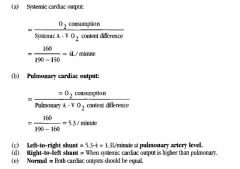
Oxygen saturation and pressure gradient in different cardiac diseases:
|
|
|
|
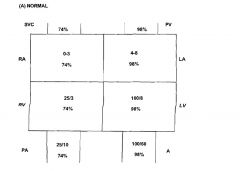
normal
|
|
|
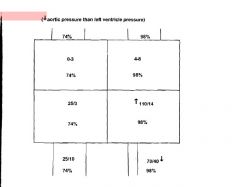
AS
|
|
|
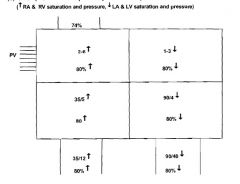
TAPVR (Total anomalous pulmonary venous return)
|
|
|
vsd
|
|
|
tof
|
|
|
ps
|
|
|
PDA
|
|
|
TRANSPOSITION OF GREAT VESSELS
|
|
|
TRUSCUS
|
|
|
|
|
|
Which organ gets maximum blood supply in fetal life from cardiac output?
|
Which organ gets maximum blood supply in fetal life from cardiac output? Placenta (65%). All other organs get 35%.
|
|
|
Maximum decline of pulmonary pressure after birth:
|
Maximum decline of pulmonary pressure after birth: first 2-3 days of life,decline occurs mostly in first hour of birth.
|
|
|
Most important factor causing pulmonary vasoconstriction?
|
Most important factor causing pulmonary vasoconstriction? Hypoxia. Other factors are acidosis, sepsis (group B Strep,
which releases thromboxane A2, which causes pulmonary vasoconstriction). |
|
|
Time to close functionally:
|
Time to close functionally:
Foramen ovale: by 3 months ofage. Ductus arteriosus: by10-15 hours, but anatomic obliteration of ductus does not occur until after first week oflife. |
|
|
Most important factor inductal closure of neonate:
|
Most important factor inductal closure of neonate: oxygen. (Hyperoxia closes duct, hypoxia opens it.)
|
|
|
Factors closing duct
|
Factors closing duct indomethacin, hyperoxia, alkalosis.
|
|
|
Factors opening duct
|
Factors opening duct: hypoxia, prostaglandin E1, S, acidosis.
|
|
|
A newborn has cyanosis and respiratory distress. Initially, how do you differentiate cardiac from pulmonary disease?
|
A newborn has cyanosis and respiratory distress. Initially, how do you differentiate cardiac from pulmonary disease? (Very
important) hyperoxia test. (Give 100% oxygen.) IfP02 is more than 150, then it is probably a pulmonary disease. IfP02is less than 150, then it isprobably a cardiac disease. DEFINITIVE DIAGNOSIS: echocardiogram |
|
|
A full-term newborn has hypoxia and severe respiratory distress, low apgar and history of fetal distress, and is on ventilator with
very high setting (100% oxygen). This may be due to |
A full-term newborn has hypoxia and severe respiratory distress, low apgar and history of fetal distress, and is on ventilator with
very high setting (100% oxygen). This may be due to: persistent pulmonary hypertension (PPHN |
|
|
The most useful measure of systolic function of the left ventricle:
|
The most useful measure of systolic function of the left ventricle: left ventricular ejection fraction (LVEF) (stroke volume/end-diastolic volume) Normal LVEF: above 55 %
...--Mildly reduced LVEF: 40-50 % Moderately reduced LVEF: 30-40 % Severely reduced LVEF: less than 30 % Please remember, cardiac output is a poor measure of systolic function |
|
|
The effect of diastolic dysfunction of the left ventricle (important):
|
The effect of diastolic dysfunction of the left ventricle (important): rise of left ventricular filling pressure, rise of left atrial pressure, pulmonary congestion, reduce cardiac output if ventricular filling is impaired. Ventricular relaxation (or diastole) is energy dependent. Increased interstitial fibrosis and poor cardiac relaxation: occurs in ischemia or hypoxemia, myocardial hypertrophy, and chronic volume overload
|
|
|
A patient appears with heart failure and increased preload. The drug used to reduce the preload and to improve the clinical condition (very important):
|
A patient appears with heart failure and increased preload. The drug used to reduce the preload and to improve the clinical condition (very important): diuretics or venodilating agent that reduces the venous return.
|
|
|
Preload is characterized by
|
Preload is characterized by end-diastolic volume or pressure.
(i) Normal heart with increased preload: improves systolic function. (ii) Failing heart with increased preload: does not improve systolic function but further worsen pulmonary congestion. (iii) Normal heart with decreased preload; decreases systolic function and pressure. (iv) Failing heart with decreased preload: little effect on left ventricular pressure. |
|
|
Ventricular afterload:
|
Ventricular afterload: directly proportional to systemic pressure; inversely proportional to thickness of the ventricle.
arterial pressure x the radius of the left ventricle Afterload = (arterial pressure X radius of the left ventricle Increased)/2 X thinkness of left ventricle Afterload: occurs in dilated thin ventricle at any given arterial pressure. Decreased afterload: occurs in smaller or thicker ventricle at any given arterial pressure. A patient appears with increased afterload resulting in reduced cardiac performance, Next step in management afterload should be reduced |
|
|
The most common cause of right ventricular pressure overload (important):
|
The most common cause of right ventricular pressure overload (important): left-sided heart dysfunction resulting in
pulmonary hypertension. Right-sided heart failure: due to either chronic right ventricular pressure overload (e.g., pulmonary hypertension due to cor pulmonale or pulmonary vascular disease) or to intrinsic dysfunction of right ventricle or its valves. |

