![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
Acute kidney injury (AKI) criteria
|
an absolute increase in the serum creatinine level of 0.3 mg/dL (26.5 µmol/L) or above from baseline within 48 hours; an increase in the serum creatinine level of 50% or more, or urine output less than 0.5 mL/kg/h for more than 6 hours.
|
|
|
Frequent manifestations of AKI include
|
Frequent manifestations of AKI include retention of metabolic waste products such as urea and creatinine and failure to regulate the content of the extracellular fluid that may result in metabolic acidosis, hyperkalemia, disturbances in body fluid homeostasis, and secondary end-organ dysfunction.
|
|
|
Patients with suspected AKI should undergo a thorough history including evaluation of any nephrotoxic exposures such as
|
Patients with suspected AKI should undergo a thorough history including evaluation of any nephrotoxic exposures such as iodinated contrast agents, NSAIDs, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers, and cyclooxygenase-2 inhibitors.Physical examination should include evaluation of volume status and a search for extrarenal manifestations that may suggest a cause of the AKI; for example, the presence of palpable purpura is suggestive of a vasculitic cause.
|
|
|
urine analysis
GN |
dipstic3+ protein
sediment- dysmorphic protreinuria eryt casts |
|
|
urine analysis minimal change disease
focal segmrmtal glomurulosclerosis |
dipstic 3+ protein
sediment oval fat bodies fatty cats |
|
|
urine analysis
acute tubular nectrosis |
dipstick- 1+ protein
muddy brown casts renal epithelial cells and casts |
|
|
urine analysis
acute interstitial nephritis utrinary tract infection |
dipstick- 1+ protein
leukocytes leukocyte casts eosinophil uria |
|
|
urine analysis
cholesterol emboli |
minimal abnormalirty
few cells minimal protein sedimeny- dysmorphic hematuria erytr casts |
|
|
urine analysis
trombocytic micro anguiopathy |
muddy brown casts
renal epithelial cells and casts distic" minimal abnormalirty few cells minimal protein |
|
|
urine analysis
pigment nephropathy)rhabdomyolsis with acute tubular necrosis) |
rhabdomyolsis with acute tubular necrosis
dipstick: blood on dipstick and no blood on micrscopic muddy brown casts, renal tubular epitjelial cells and casts |
|
|
urine analysis
drug toxicity urate crystals phosphate crystals TLS Ca oxalate cristalls ethylene glycol orlistat |
sediment- cristalluria
|
|
|
UA obstructin stome
|
cristal uria
monomorphic hematuria |
|
|
obstr tumor
kidney infarct renal vein thrombosis |
monomorphic hematuria
dipstic- minimal abn few cells. minimal protein |
|
|
Prerenal azotemia develops when
|
Prerenal azotemia develops when autoregulation of kidney blood flow can no longer maintain GFR. This condition generally occurs in patients with a mean arterial pressure below 60 mm Hg but may occur at higher pressures in individuals with CKD or in those who take medications that can alter local glomerular hemodynamics, such as NSAIDs.
Patients with prerenal azotemia may have a history of fluid losses and decreased fluid intake accompanied by physical examination findings consistent with extracellular fluid volume depletion, such as postural hypotensio |
|
|
Intrarenal Disease
|
* Acute Tubular Necrosis
* Contrast-Induced Nephropathy * Rhabdomyolysis and Pigment Nephropathy * Acute Interstitial Nephritis * Thrombotic Microangiopathies |
|
|
Acute tubular necrosis is the most common form
Onset of this condition usually occurs after a sustained |
Acute tubular necrosis is the most common form of intrarenal disease that causes AKI in hospitalized patients. Onset of this condition usually occurs after a sustained period of ischemia or exposure to nephrotoxic agents. Acute tubular necrosis may resolve over 1 to 3 weeks or result in permanent end-stage kidney disease, depending on the duration and severity of the ischemic or nephrotoxic insult.
|
|
|
have the greatest risk of developing contrast-induced nephropathy, especially if concurrent diabetes mellitus is
|
Patients undergoing coronary angiography who have a serum creatinine level of 1.5 mg/dL (132.6 µmol/L) or higher or a GFR below 60 mL/min/1.73 m2 have the greatest risk of developing contrast-induced nephropathy, especially if concurrent diabetes mellitus is present.
|
|
|
The most effective intervention to decrease the incidence and severity of contrast-induced nephropathy is volume expansion with either isotonic saline or sodium bicarbonate (
|

|
|
|
Alternatives to Iodinated Contrast Agents
|
Digital subtraction angiography with carbon dioxide contrast is an appropriate alternative imaging study in high-risk patients. However, this technique cannot be used for imaging above the diaphragm because of the risk of cerebral toxicity.
Gadolinium-containing compounds had been used as an alternative to iodinated contrast in patients with CKD but are now believed to be nephrotoxic in high-risk individuals. Furthermore, gadolinium may be associated with nephrogenic systemic fibrosis in patients with kidney dysfunction and therefore is not recommended for individuals at highest risk for contrast-induced nephropathy, especially those with a GFR below 30 mL/min/1.73 m2. |
|
|
diagnosis of rhabdomyolysis should be considered in patients with a serum creatine kinase level
|
A diagnosis of rhabdomyolysis should be considered in patients with a serum creatine kinase level above 5000 U/L (83.5 µkat/L) who demonstrate heme positivity on urine dipstick testing in the absence of hematuria. Complications of rhabdomyolysis include hypocalcemia, hyperphosphatemia, hyperuricemia, metabolic acidosis, acute muscle compartment syndrome, and limb ischemia.
|
|
|
most effective intervention to limit nephrotoxicity in patients with rhabdomyolysis.
|
Expansion of the extracellular fluid volume with isotonic saline is the most effective intervention to limit nephrotoxicity in patients with rhabdomyolysis. Calcium repletion therapy should be reserved only for hypocalcemic patients with this condition who have cardiac or neuromuscular irritability, because this therapy can cause rebound hypercalcemia in the recovery phase.
|
|
|
Acute interstitial nephritis is most commonly caused by a
|
Acute interstitial nephritis is most commonly caused by a hypersensitivity reaction to a medication, and proton pump inhibitors are now believed to be a common cause of drug-induced acute interstitial nephritis. Acute interstitial nephritis also may be caused by certain infections or autoimmune conditions
|
|
|
Drug-induced acute interstitial nephritis may manifest as
|
Drug-induced acute interstitial nephritis may manifest as rash, pruritus, eosinophilia, and fever; however, these features may be absent, particularly in acute interstitial nephritis due to use of NSAIDs and proton pump inhibitors.
|
|
|
Management of drug-induced interstitial nephritis includes
|
Management of drug-induced interstitial nephritis includes withdrawing the inciting medication. Corticosteroids may be used in patients with aggressive disease, such as those with persistent or worsening azotemia despite discontinuation of the inciting agent, and biopsy may be particularly warranted if this therapy is being considered. Patients demonstrating active inflammation in the absence of significant chronic damage seen on biopsy are more likely to benefit from cortico-steroids
|
|
|
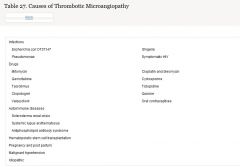
Causes of Thrombotic Microangiopathy
|
|
|
|
Manifestations of the thrombotic microangiopathies
|
Manifestations of the thrombotic microangiopathies may include AKI that is usually accompanied by microangiopathic hemolytic anemia. Approximately 50% of patients have low C3 levels. The urine sediment usually shows minimal or no abnormalities and is nondiagnostic; rarely, erythrocyte or muddy brown casts may be seen.
|
|
|
urinary tract obstruction associated with acute kidney injury
|
anage urinary tract obstruction associated with acute kidney injury.
Key Point * Nephrostomy tube placement is indicated to manage urinary tract obstruction associated with acute kidney injury when the obstruction is not relieved with bladder catheter placement. This patient most likely has urinary tract |
|
|
prerenal azotemia.
|
Nausea, vomiting, and anorexia accompanied by relatively low blood pressure in the absence of edema or urine sediment abnormalities strongly suggest prerenal azotemia. Prerenal disease is usually associated with oliguria and a fractional excretion of sodium (FENA) below 1%, but patients with chronic kidney disease have a decreased capacity for tubular sodium reabsorption and therefore may have a higher FENA in the setting of prerenal diseas
|
|
|
acute tubular necrosis usually shows
|
acute tubular necrosis usually shows muddy brown casts or tubular epithelial cell casts
|
|
|
Renal vein thrombosis i
|
Renal vein thrombosis is an uncommon cause of acute kidney injury associated with hematuria and nephrotic-range proteinuria. This condition is most often associated with membranous nephropathy, malignancy, trauma, or hypercoagulable states.
|
|
|
acute phosphate nephropathy.
|
acute phosphate nephropathy. This condition typically develops within a few days of exposure to an oral sodium phosphate bowel preparation but often remains unrecognized until laboratory studies are performed at a later time. Manifestations of acute phosphate nephropathy may include hyperphosphatemia out of proportion to the degree of kidney failure and minimal abnormalities on urinalysis.
|
|
|
postural hypotension,
|
postural hypotension, tachycardia, and progressive azotemia despite ongoing hydration with normal saline argues against prerenal azotemia. This condition also is rarely associated with a serum phosphorus level above 13 mg/dL (4.2 mmol/L).
|
|
|
Newly Described Nephrotoxic Acute Kidney Injury
|
Orlistat may cause acute oxalate nephropathy. Intravenous immune globulin therapy can induce AKI through osmotic tubular injury in preparations containing additives such as sucrose, maltose, and glycine.
Sodium phosphate–containing cathartic agents that are frequently used in preparation for colonoscopy have been associated with AKI in patients who have risk factors for acute phosphate nephropathy, such as reduced GFR; advanced age; and use of ACE inhibitors, angiotensin receptor blockers, NSAIDs, and diuretics. However, acute phosphate nephropathy also may occur in patients receiving sodium phosphate solutions for bowel preparation who have normal kidney function and no apparent risk factors |

