![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
113 Cards in this Set
- Front
- Back

|

|
|

|

|
|
|
Name three lethal chromosomal aberrations
|
1) DIcentric
2) Ring 3) Anaphase Bridge (technically a chromatid aberration) |
|
|
What molecular technique can be used to detect chromosomal translocations?
|

FISH.
|
|
|
53BP-1
|
DNA repair protein that partially regulates whether a DSB is handled via homologous recombination or non-homologous end-joining
- Inhibits homologous recombination |
|
|
A DNA DSB occurs. Which repair process is most likely used?
In G1? In S/G2? |

|
|
|
Acute vs Late Radiation Effects
|
Acute Effects: The target cell is usually apparent and can be repaired fairly rapidly.
- The timing of onset is based on the turnover rate of the mature functional cells. Late Effects: May be due to both vascular damage and/or parenchymal cell loss. - May improve but is never completely reversed. - More sensitive to changes in fractionation. |
|
|
After a dose of 1-2 Gy, how many damaged bases are induced per cell?
|
>1000 per cell
|
|
|
After a dose of 1-2 Gy, how many double strand breaks are induced per cell?
|
~40 per cell
|
|
|
After a dose of 1-2 Gy, how many of single strand breaks are induced per cell?
|
~1000 per cell
|
|
|
Amifostine (WR-2721)
|
- Radioprotectant
- Prodrug and aminothiol - FDA approved for salivary gland cancers - Selectivity: Normal cells have a higher pH and higher levels of alkaline phosphatase -> greater activation of amifostine into its active form - Toxicity: N/V, hypotension - NB: Does NOT protect the CNS (cannot cross BBB) |
|
|
Apoptosis
|
- Organized cell death
- Characterized by cell shrinkage and "laddering" of DNA on a gel - Generally dependent on p53 - Steps: 1) Cell rounds up and detaches from surounding tissue 2) Chromatin condensese and nucleus fragments 3) Cytoplasmic condensation leads to cell shrinkage 4) Separation of the cell into apoptotic bodies, which are phagocytized |
|
|
Artemis
|
- DNA endonuclease that plays a role in NHEJ
- Processes any 5' or 3' overhangs, hairpins, etc. - Binds DNA-PKcs |
|
|
Ataxia Telangectasia
|

- Familial cancer syndrome caused by mutation of ATM
- Leads to cerebellar ataxia and oculocutaneous telangectasias as well as heightened sensitivity to ionizing radiation - NOT sensitive to UV light - ATM is involved in the rapid response to DSBs and other radiation damage - AT cells are notable bc they do NOT arrest in S phase in response to DNA damage (radioresistant DNA synthesis) |
|
|
Autophagy
|
- Process by which cells cannibalize themselves to procure ATP and/or molecular precursors
- Unclear whether this is a drastic attempt at survival or a step to promote death |
|
|
Base Excision Repair
|

|
|
|
bcl-2 function
|
Anti-apoptotic gene
|
|
|
Bone Marrow Assay
|
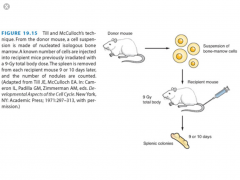
- Transplant assay used to determine the dose response of acutely responding tissues
- A donor mouse is given a test dose D --> BM cells are injected into a supralethally-radiated recipient mouse --> 9-10 days later, the donor is sacrificed --> the number of splenic colonies are counted --> the number of colonies are plated vs dose |
|
|
Bone marrow transplants may be useful after exposure to what dose range?
|
8-10 Gy
|
|
|
BRCA-1
|
- Located on 17q21
- Codes for a protein that assists with DNA repair. Most associated with HOMOLOGOUS RECOMBINATION. Thus, cells with mutated BRCA show increased genomic instability. - Mutated in 5-10% of breast cancer cases (BRCA1 and 2 together) |
|
|
Caretaker Genes: What are they? Examples?
|
- Monitor the stability of the genome
- Dysfunction indirectly influences oncogenesis by leading to genomic instability and an increased mutation rate - No direct influence on tumor growth - Examples: ATM, XP, BRCA1, BRCA2, MSH6, NBS |
|
|
cdc2
|
- Codes for a kinase
- Same as Cdk1 - Pair with Cyclin A and B |
|
|
Cyclin A
|
- Associates with cdk2 and then cdk1
- Accumulates at G1/S and persists through S phase - Its activity is needed for entry into S phase, progression through S and entry into M phase - Can inactivate E2F |
|
|
Cyclin B
|
- Associated with cdk1
- Must be degraded for cells to exit M phase |
|
|
Cyclin D1, D2 and D3
|
- Associate with cdk4 and cdk6
- Targets Rb for phosphorylation |
|
|
Cyclin E
|
- Associates with cdk2
- Required for the G1/S checkpoint - Maintain Rb in a phosphorylated state, leading to accumulation of active E2F |
|
|
Define: D10
|
- The dose required to kill 90% of a cell population
- Equal to 2.3 x D0 |
|
|
Describe the death receptor apoptotic pathway.
|

1) Fas ligand binds Fas (other death-inducing ligand combos exist)
2) The intracellular death domain interacts with pro-caspase 8 to create DISC (death-inducing signalling complex) 3) DISC activates caspase 8 4) Initiator caspase 8 activates the effector caspases --> apoptosis |
|
|
Describe the general process of homologous recombination.
|
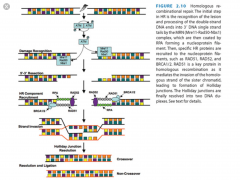
1) Recognition --> phosphorylation of ATM
2) MRN complex is recruited to create 3' single-stranded ends 3) The newly created ends are wrapped in RPA 4) RAD51, RAD52 and BRCA 1/2 are recruited and help the homologous strand invade 5) Formation of a Holliday junction 6) Resolution of the Holliday junction and ligation |
|
|
Describe the general steps of mismatch repair.
|
1) Recognize damage
2) Recruit MMR factors 3) Identify which strand is new --> excision of incorrect nucleotides 4) Re-synthesis and ligation |
|
|
Describe the mitochondrial death pathway.
|
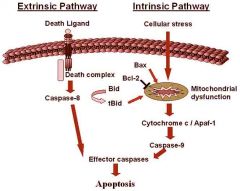
1) Disruption of the mitochondrial membrane
2) Release of cytochrome-c 3) Cytochrome-c and APAF-1 interact to activate caspase 9 4) Initiator caspase 9 activates the effector caspases --> apoptosis |
|
|
Describe the regulation of the HIF pathway
|
A: Under normoxic conditions, a group of enzymes called prolyl hydroxylases (HPHs) add hydroxyl groups (OH) to two proline residues of HIF-1α. The hydroxylation of HIF-1α by HPH allows the VHL tumor-suppressor gene to bind and promotes the addition of ubiquitin groups. The addition of ubiquitin groups targets HIF-1α for degradation in the proteasome. B: Under hypoxic conditions, the HPHs cannot hydroxylate HIF-1α on proline residues owing to their requirement for molecular oxygen, and HIF-1α becomes stabilized. It then binds with the HIF-1β subunit in the nucleus and promotes transcription of at least 50 target genes that regulate angiogenesis, erythropoiesis, tissue remodeling, and glycolysis. Most of the studies to date have shown that HIF is essential for tumor growth.
|
|
|
Describe the role HIF plays in tumorogenesis
|
When oxygen levels decrease, HIF-1A and HIF-1B combine to promote transcription of 50+ hypoxia-related gene. Among other things, these genes regulate angiogenesis, erythropoesis, tissue remodeling and glycolysis.
|
|
|
Describe the steps of non-homologous end joining.
|

1) Recognition of damage --> KU binding
2) Recruitment of DNA-PKcs (holds DNA together?) 3) End processing via Artemis 4) Fill-in Synthesis (if needed) 5) Ligation via PNK/XRCC4/DNA ligase IV/XLF |
|
|
Dose modification factor
|
Used to describe the effect of a radiation protector.
DMF = [Dose of RT required to produce a given effect in the PRESENCE of a drug]/[Dose of RT required to produce that same effect in the ABSENCE of the drug] |
|
|
E2F
|
- Transcription factor
- Normally bound to Rb protein in G0 and G1 (inactive) - When Rb is phosphorylated, E2F is released, initiates transcription and leads to progression into S phase |
|
|
Equation for a decade of cell kill
|
D10=2.3*D0
|
|
|
Equation for Survival Fraction in-vitro
|

|
|
|
Equation: Finding the skin gap for matching fields at depth
|
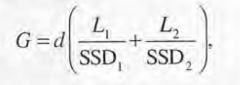
|
|
|
Equation: Survival fraction using the linear-quadratic model
|

|
|
|
Explain the oxygen fixation hypothesis
|
After damage by radiation-induced free radicals, many ionized target molecules can subsequently repair themselves and function normally. In the presence of oxygen, however, an organic peroxide is formed, which cannot be easily reversed. The radiation damage is thus said to "fix," or make permanent, the damage.
(pg. 88) |
|
|
For in utero radiation exposure, when is a fetus most susceptible to the development of mental retardation?
|
Greatest susceptibility: 8-15 weeks
Less susceptibility: 16-25 weeks (4x less risk) Very little risk: <8 weeks or >25 wks NB: Based on Abomb data |
|
|
Gatekeeper genes: What are they? Examples?
|
- Directly regulate tumor growth by inhibiting cell division or promoting apoptosis
- Both copies of a gatekeeper gene must be inactivated to disable its function - Examples: APC (colon), VHL (renal cell) |
|
|
Give an example of oncogene activation via translocation.
|
1) t(9;22) bcr-abl in CML
2) t(8;14) c-myc in Burkitt's Lymphoma 3) t(14;18) bcl-2 in DLBCL |
|
|
HNPCC
|
- Familial cancer syndrome
- Caused by defective mismatch repair |
|
|
Homologous recombination: Error-prone or error-free?
|
Mostly error free due to the involvement of a template strand.
|
|
|
How does dose rate affect biological effectiveness?
|
In general, biological effectiveness goes down as dose rate is decreased (and exposure time is consequently lengthened)
|
|
|
How does Her-2/neu act as an oncogene?
|
Encodes a growth factor receptor that, when mutated, no longer requires its ligand to become active
In other words, the kinase becomes constitutively active. |
|
|
If 10^7 cells were irradiated according to single hit kinetics so that the average number of hits per cell is one, how many cells would survive?
|

|
|
|
Inverse Dose-Rate Effect
|
Phenomenon where decreasing the dose rate results in increased cell killing. Postulated to occur because a low dose rate allows the cell to continue to cycle until it arrests in G2, a radiation sensitive period. Higher dose rates, in contrast, make the cell arrest wherever it is at the start of irradiation, which is likely less radiosensitive than G2.
|
|
|
Jejunal Assay
|
- Used to determine the dose response of acutely responding tissues
- Radiation mice using 11-16 Gy --> wait 3-5 days --> sacrifice and count the number of regenerating crypts per circumference --> plot number vs dose - Limitations: Have to use >10 Gy to see an effect, only know the NUMBER of surviving crypts and not the survival FRACTION |
|
|
Kidney Tubule Assay
|

- Used to determine the dose response of LATE responding tissues
- A single kidney per mouse is irradiated --> wait 60 weeks --> sacrifice and count number of regenerated tubules --> plot versus dose |
|
|
KU70 and KU80
|
- Genes involved in repair of DNA DSBs by binding to the free ends.
- First step in non-homologous end joining - If defective, the cell's ability to repair DSBs is reduced --> increased radiosensitivity |
|
|
Law of Bergonie and Tribondeau
|
Greater radiosensitivity tends to be associated with those cells that:
1) are less differentiated 2) have greater proliferative potential 3) divide more rapidly |
|
|
LET
|
The energy transferred per unit track length.
Unit: keV/micrometer |
|
|
Li-Fraumeni Syndrome
|
- Autosomal dominant
- Germ line missense mutation in p53 - Associated with increased incidence of sarcomas, leukemia, brain tumors, lung and breast cancer |
|
|
Mismatch repair
|
- Repair process whereby the cell detects irregularities between the two strands of DNA
- Usually uses methylation to identify the "old" strand - Defective in HNPCC and Lynch Syndrome - Defective MMR genes can be detected using a microsatellite instability assay |
|
|
Mitotic Death
|
- Primary mode of radiation-induced cell death
- Causes inflammation of surrounding tissue, cell swelling and a DNA smear in gel - Often preempted by an asymmetric exchange-type chromosomal aberration (ring or dicentric) |
|
|
Mitotic shake-off
|
- Cells are synchronized in M phase
|
|
|
Mouse Skin Cell Assay
|

Allows you to plot the number of surviving skin cells (NOT survival fraction) vs dose
|
|
|
MSH, MLH and PSM proteins
|
- Mismatch repair proteins
- Mutations in these proteins can lead to microsatellite instability and carcinogenesis - Associated with HNPCC |
|
|
myc
|
- Oncogene that can lead to either proliferation or apoptosis depending on the tumor microenvironment
|
|
|
Name four mechanisms for oncogene activation.
|

1) Retrovirus integration (viral promoter)
2) Mutation 3) Gene amplification 4) Translocation |
|
|
Name the effector caspases
|
3, 6, and 7
|
|
|
Name the initiator caspases
|
2, 8, 9 and 10
|
|
|
Name two DNA-associated proteins that can be tagged in order to assay DNA damage.
|
γH2AX and 53BP-1
|
|
|
Name two methods for assaying DNA DSBs.
|

1) Pulsed field gel electrophoresis (PGFE)
2) Single cell electrophoresis (comet assay) |
|
|
NBS
|
- Direct phosphorylation target of ATM
- Necessary for DSB repair in response to radiation - Creates a complex with MRE11 and Rad50 |
|
|
NHEJ primarily occurs in what stage of the cell cycle?
|
G1 (no sister chromatid that can be used for repair)
|
|
|
Non-homologous end-joining: Faithful or error-prone?
|
Very error prone, as it doesn't use a template strand.
|
|
|
Northern Blot
|
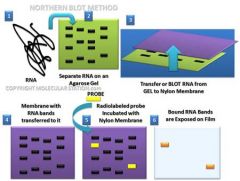
Technique for:
- Detecting the presence of a specific RNA sequence (RNA-ssDNA) - Determining the relative amount of mRNA present - Detecting relative RNA size |
|
|
Nucleotide Excision Repair
|

- Repairs bulky adducts, such as those caused by UV light and alkylating agents
- Mutations in this system do NOT lead to radiosensitivity; however, they do increase sensitivity to UV light, such as in XERODERMA PIGMENTOSUM - Two systems: global genome repair and transcription-coupled - Steps: 1) Recognize damage 2) Excise damage 3) Repair damaged strand via polymerase 4) Ligate |
|
|
Obstetrical x-rays have been conclusively linked with an increased risk of childhood cancer. True or false?
|
True. Initial studies were done by Stewart in the UK in the 1950s. Currently studies suggest that an obstetrical x-ray increases the risk of childhood cancer by 40% over baseline (6% per Gy absolute excess risk).
|
|
|
OER for neutrons
|
~1.6
|
|
|
OER for sparsely ionizing radiation ie x-rays
|
2.5-3.5
Tends to be larger for larger doses |
|
|
p53
|
- Proapoptotic tumor suppressor gene
- Mutated in Li-Fraumeni syndrome - Levels are usually kept low due to binding of MDM2 and subsequent proteolysis |
|
|
p53: Tumor suppressor or oncogene?
|
Tumor suppressor
- Loss of function lead to anti-apoptotic pathways |
|
|
Parallel Organs at Risk
|
- Functional damage will not occur until a critical number of FSUs have been inactivated
- Consequently, parallel organs exhibit a theshold volume, above which function begins to be compromised - Once the threshold volume has been exceeded, function declines in a graded way (not all-or-none) - Examples: Lung, liver |
|
|
Pig Skin Assay
|
- Functional assay used to determine skin effects of radiation
- Acute assay: A rectangle of pig skin is radiated --> the reaction is watched and graded --> avg reaction over a given period of time is plotted vs dose - Late assay: A rectangle is tattooed on pig skin --> radiated --> the size of the rectangle is charted over time vs dose - Because pigs are large and expensive, rodent skin can also be used |
|
|
PNK/XRCC4/DNA ligase 4/XLF
|
- Ligase complex used in non-homologous end joining
|
|
|
Potentially Lethal Damage
|
The component of radiation damage that can be modified by post-irradiation environmental conditions.
i.e. This damage generally causes cell death under ordinary circumstances, but death can be averted by changing the post-RT environment. |
|
|
RAD51
|
Protein involved in the repair of DNA damage via homologous recombination
|
|
|
Rb:
|
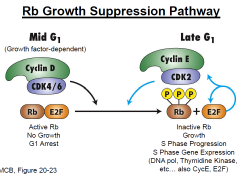
- Tumor suppressor gene that regulates the cell cycle
- Requires inactivation of both copies for loss of function - Active only in G1 cells - Phosphorylation of the protein releases E2F (transcription factor) -> cell cycle progression into S phase - Mutations are commonly found in retinoblastoma, osteosarcoma and small cell |
|
|
RBE
|
Relative Biological Effectiveness
RBE= Dose of 250 keV xrays required to produce a given effect/Dose of test radiation required to produce the same effect |
|

Refer to the problem below. Now imagine that the cells undergo three rounds of cell division during treatment. Approximately what dose would be needed to achieve the same level of tumor control (90%)?
|

|
|
|
Serial Organs at Risk
|

- Exhibit a binary response i.e. above a threshold dose, there is loss of organ function
- As the radiation field size increases to include more FSUs, the probability of tissue complications becomes steeper and moves left (to lower doses) - Example: Spinal cord |
|
|
Spinal Myelopathy Assay
|
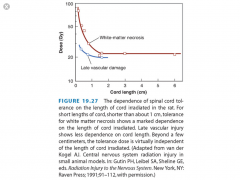
- Functional assay to determine the dose response of a serial OAR
- Irradiate a section of rat spinal cord --> wait 4-12 months --> score muscle atrophy and/or paralysis vs dose - Late spinal effects in animals peak at about 1-2 years with a large vascular component - Dose per fraction is more important than the timing of RT - For small volumes, length of spinal cord irradiated is crucial; however, the reaction becomes semi-independent of dose when >2 cm (see figure) |
|
|
Structurally Defined FSU
|
- Small, self-contained subunit that is independent of its neighbours
- Cells from one FSU cannot migrate to another so a clonogen must remain alive within the FSU to repopulate it - Examples: Kidney, lung, liver |
|
|
Structurally Undefined FSU
|
- FSUs that are not readily defined so that cells may readily migrate between them
- Cells from one FSU may migrate to repopulate another - Examples: Skin |
|
|
Sublethal Damage
|
- "Minor" damage that can usually be repaired within 24 hours.
- Can "add up" to lethal damage if not repaired - Causes the increase in survival seen with fractionation NB: Little repair of SLD is seen with high LET radiation |
|
|
Sulfhydryls
|
Radioprotectors
Use a thiol group (-SH) to scavenge free radicals Must be present within 1 second of radiation in order to have an effect Highly oxygen dependent (bc radioprotectants mitigate the indirect damage of RT) - Toxicity can be reduced by covering the thiol group with a phosphate Ex: Cysteine (causes N/V at therapeutic doses) |
|
|
Survival Fraction (in a dish)
|
SF = # of colonies counted/[#of colonies plated * plating efficiency]
|
|
|
Telomerase
|
-Reverse transcriptase that rebuikds chromosome ends to counteract the shortening that occurs with cell division
|
|
|
Testicular Assay
|
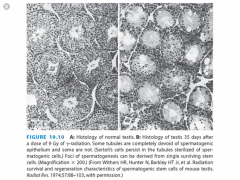
- Used to determine the dose response of acutely responding tissues
- Irradiate mice (8-16 Gy) --> wait ~6 weeks --> sacrifice and count the proportion of tubules with spermatogenic epithelium --> plot versus dose |
|
|
TGF-B
|
- Pro-inflammatory factor
- Promotes growth of connective tissue and fibrosis |
|
|
TGF-B
|
- Normally acts as an antiproliferative factor
- Normally inhibits the phosphorylation of Rb (via synthesis of p21 and p15), thus preventing the release of E2F and preventing progression from G1 to S - In transformed cells, also acts as a pro-angiogenic and immunosuppressive factor |
|
|
Tissue Rescue Unit
|
Minimum number of FSUs needed to maintain tissue function
|
|
|
TNF-Alpha
|
- Strongly proinflammatory and cytotoxic
- Induces the proliferation of fibroblasts, inflammatory cells and endothelial cells - When used clinically, leads to fatigue, anorexia, and weight loss |
|
|
TSP-1
|
- Normally ANTI-angiogenic and induced by p53
- When down-regulated, cells may undergo oncogenesis and angiogenesis |
|
|
VHL
|
- Mutated in Von Hippel Lindau Syndrome
- Normally inhibits HIF by targeting it for degradation - When mutated in Von Hippel Lindau, HIF is not targeted --> constitutively elevated levels of HIF --> elevated levels of VEGF --> increased angiogenesis |
|
|
What is the average Do for human cells?
|
3 Gy
|
|
|
What is the difference between acute and chronic hypoxia?
|
Acute hypoxia: Results from the temporary closure of tumor blood vessels secondary to malformed vasculature
Chronic hypoxia: Results from the limited diffusion distance of oxygen through respiring tissue. |
|
|
What is the most variable stage of the cell cycle?
|
G1
Highly variable due to differences in nutrient supply, growth factors, genomic stability and microenvironment |
|
|
What is the risk of a fatal cancer based on a given exposure? Genetic disorder? Non-fatal cancer?
|
Fatal cancer: 4%/Sv i.e. 4x10^-2 per Sievert
Genetic disorder: 0.8%/Sv i.e. 0.8 x 10^-2 per Sievert Non-fatal cancer: Same as genetic |
|
|
What is the survival fraction of irradiated cells?
|
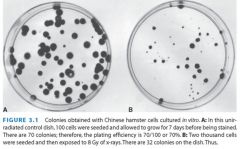
32/(2000*.7)=0.023
|
|
|
What proteins are associated with non-homologous end-joining?
|
1) KU70/KU80
2) DNA-PKcs 3) Artemis: Endonuclease that processes the DNA ends 4) DNA polymerase μ or λ: Performs any necessary fill-in synthesis 5) PNK/XRCC4/DNA ligase 4/XLF: Performs the final ligation |
|
|
What proteins are involved in homologous recombination?
|
ATM: Initial response to DNA damage
MRN complex (MRE11, RAD50, NBS1): Endonuclease complex that creates 3' single stranded DNA tails RPA: Wraps the 3' tails to create a nucleoprotein filament RAD51, RAD52, BRCA 1/2: Protein complexes that mediates invasion of the sister chromatid adjacent to the undamaged strand --> Holliday junction |
|
|
Which members of the Bcl-2 family are anti-apoptotic?
|
Bcl-2, Bcl-xl, Mcl-1
Prevents cell from dying |
|
|
Which members of the Bcl-2 family are proapoptotic?
|
Bax, Bak, Bid and Bim
Encourage cell to die |
|
|
You would like to assess DNA damage using gel electrophoresis. What conditions will be needed to assess SSBs? DSBs?
|
DSBs: Neutral solution
SSBs: Alkaline solution (needed to separate the strands so that the damaged strands can run out in the gel) |
|
|
Western Blot
|
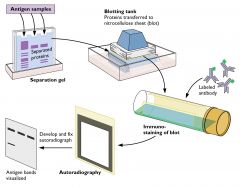
Technique to detect specific proteins (Protein-Antibody)
NB: - Native proteins are separated by 3D structure - Denatured proteins (via SDS) separate by size - Secondary and tertiary antibodies may be used to amplify the signal |
|
|
Southern Blot
|
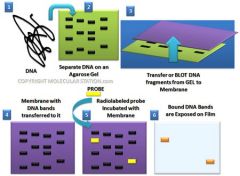
Technique used to detect the presence of a specific sequence in a DNA sample (DNA-DNA)
|
|
|
Sanger Method (DNA Sequencing)
|

Method for sequencing DNA using dideoxynucleotides (have a -H at the 3' end instead of an -OH, terminating chain elongation)
NB: Reading from the bottom up gives the sequence of the complementary strand |

